Abstract
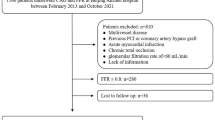
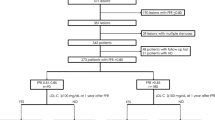
Cardiovascular events can occur after deferred revascularization, and malondialdehyde-modified low-density lipoprotein (MDA-LDL) has been suggested to be an atherogenic marker. We investigated the relationship between serum MDA-LDL levels and clinical outcomes in patients with fractional flow reserve (FFR)-guided deferral of revascularization. Among 3084 patients undergoing coronary angiography, we retrospectively analyzed 127 patients with intermediate stenosis and deferred revascularization based on FFR > 0.80. Median follow-up interval was 30.4 months, and serum MDA-LDL was measured prior to the measurement of FFR. We evaluated the composite of major adverse cardiac events (MACEs), including cardiac death, myocardial infarction, ischemia-driven deferred lesion revascularization, and any revascularization. MACEs occurred in 18 (14.2%) patients. The MACE group presented with significantly higher MDA-LDL levels than the non-MACE group (134.9 ± 33.3 U/L vs. 95.6 ± 32.2 U/L, P < 0.001). In analysis of the receiver operating characteristics curve for the prediction of MACEs, MDA-LDL presented a significantly larger area under the curve than low-density lipoprotein-cholesterol (LDL-C; 0.810 vs. 0.687, P = 0.042). Univariate Cox regression analysis indicated a significant relationship between MACEs and MDA-LDL (per 10 U/L, HR 1.20; P = 0.004), as did the multivariate model (per 10 U/L, HR 1.17; P = 0.019). When compared according to the median LDL-C (98 mg/dL), the MACE group had significantly higher MDA-LDL in both the high (147.2 ± 27.3 U/L vs. 113.9 ± 31.2 U/L, P = 0.001) and low (103.2 ± 27.3 U/L vs. 80.2 ± 24.0 U/L, P = 0.045) LDL-C groups. Serum MDA-LDL levels were associated with cardiac events in patients with deferral of revascularization based on FFR.




Similar content being viewed by others
References
Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Koolen BJ, Koolen JJ (1996) Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 334(26):1703–1708
Barbato E, Toth GG, Johnson NP, Pijls NH, Fearon WF, Tonino PA, Curzen N, Piroth Z, Rioufol G, Jüni P, De Bruyne B (2016) A prospective natural history study of coronary atherosclerosis using fractional flow reserve. J Am Coll Cardiol 68(21):2247–2255
Xaplanteris P, Fournier S, Pijls NHJ, Fearon WF, Barbato E, Tonino PAL, Engstrøm T, Kääb S, Dambrink JH, Rioufol G, Toth GG, Piroth Z, Witt N, Fröbert O, Kala P, Linke A, Jagic N, Mates M, Mavromatis K, Samady H, Irimpen A, Oldroyd K, Campo G, Rothenbühler M, Jüni P, De Bruyne B, FAME 2 Investigators (2018) Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med 379(3):250–259
Zimmermann FM, Ferrara A, Johnson NP, van Nunen LX, Escaned J, Albertsson P, Erbel R, Legrand V, Gwon HC, Remkes WS, Stella PR, van Schaardenburgh P, Bech GJ, De Bruyne B, Pijls NH (2015) Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J 36(45):3182–3188
Kennedy MW, Kaplan E, Hermanides RS, Fabris E, Hemradj V, Koopmans PC, Dambrink JH, Marcel Gosselink AT, Van’t Hof AW, Ottervanger JP, Roolvink V, Remkes WS, van der Sluis A, Suryapranata H, Kedhi E (2016) Clinical outcomes of deferred revascularization using fractional flow reserve in patients with and without diabetes mellitus. Cardiovasc Diabetol 15:100
Masrani Mehta S, Depta JP, Novak E, Patel JS, Patel Y, Raymer D, Facey G, Zajarias A, Lasala JM, Singh J, Bach RG, Kurz HI (2015) Association of lower fractional flow reserve values with higher risk of adverse cardiac events for lesions deferred revascularization among patients with acute coronary syndrome. J Am Heart Assoc 4(8):e002172
Barbero U, D’Ascenzo F, Campo G, Kleczyński P, Dziewierz A, Menozzi M, Jiménez Díaz VA, Cerrato E, Raposeiras-Roubín S, Ielasi A, Rognoni A, Fineschi M, Kanji R, Jaguszewski MJ, Picchi A, Andò G, Soraci E, Mancone M, Sardella G, Calcagno S, Gallo F, Huczek Z, Krakowian M, Verardi R, Montefusco A, Omedè P, Lococo M, Moretti C, D’Amico M, Rigattieri S, Gaita F, Rinaldi M, Escaned J (2018) Safety of FFR-guided revascularization deferral in Anatomically prognostiC diseasE (FACE: CARDIOGROUP V STUDY): a prospective multicentre study. Int J Cardiol 270:107–112
Tanaka N, Nakamura M, Akasaka T, Kadota K, Uemura S, Amano T, Shiode N, Morino Y, Fujii K, Hikichi Y, Registry CVIT-DEFER, Investigators. (2017) One-year outcome of fractional flow reserve-based coronary intervention in japanese daily practice-CVIT-DEFER registry. Circ J 81(9):1301–1306
Doh JH, Nam CW, Koo BK, Park SH, Lee JH, Han JK, Yang HM, Lim HS, Yoon MH, Cho YK, Hur SH, Lee SY, Kim HS, Tahk SJ (2015) Long-term patient-related and lesion-related outcomes after real-world fractional flow reserve use. J Invasive Cardiol 27(9):410–415
Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, Daemen MJ, Demer LL, Hegele RA, Nicholls SJ, Nordestgaard BG, Watts GF, Bruckert E, Fazio S, Ference BA, Graham I, Horton JD, Landmesser U, Laufs U, Masana L, Pasterkamp G, Raal FJ, Ray KK, Schunkert H, Taskinen MR, van de Sluis B, Wiklund O, Tokgozoglu L, Catapano AL, Ginsberg HN (2020) Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J 41(24):2313–2330
Amaki T, Suzuki T, Nakamura F, Hayashi D, Imai Y, Morita H, Fukino K, Nojiri T, Kitano S, Hibi N, Yamazaki T, Nagai R (2004) Circulating malondialdehyde modified LDL is a biochemical risk marker for coronary artery disease. Heart 90:1211–1213
Matsuo Y, Kubo T, Okumoto Y, Ishibashi K, Komukai K, Tanimoto T, Ino Y, Kitabata H, Hirata K, Imanishi T, Akagi H, Akasaka T (2013) Circulating malondialdehyde-modified low-density lipoprotein levels are associated with the presence of thin-cap fibroatheromas determined by optical coherence tomography in coronary artery disease. Eur Heart J Cardiovasc Imaging 14:43–50
Ito T, Ichihashi T, Fujita H, Sugiura T, Ohte N (2018) Impact of malondialdehyde-modified low-density lipoprotein on coronary plaque vulnerability in patients not receiving lipid-lowering therapy: a whole coronary analysis with multislice-computed tomography. Heart Vessels 33(4):351–357
Yokoi M, Ito T, Fujita H, Sugiura T, Seo Y, Ohte N (2020) Increased serum malondialdehyde-modified low-density lipoprotein and coronary angiographic progression after drug-eluting stent implantation in patients with stable angina. Circ J 84(10):1837–1845
Ito T, Fujita H, Tani T, Ohte N (2015) Malondialdehyde-modified low-density lipoprotein is a predictor of cardiac events in patients with stable angina on lipid-lowering therapy after percutaneous coronary intervention using drug-eluting stent. Atherosclerosis 239:311–317
Kotani K, Maekawa M, Kanno T, Kondo A, Toda N, Manabe M (1994) Distribution of immunoreactive malondialdehyde-modified low-density lipoprotein in human serum. Biochim Biophys Acta (BBA)/Lipids Lipid Metab 1215:121–125
Sugiuchi H, Irie T, Uji Y, Ueno T, Chaen T, Uekama K, Okabe H (1998) Homogeneous assay for measuring low-density lipoprotein cholesterol in serum with triblock copolymer and α-cyclodextrin sulfate. Clin Chem 44:522–531
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, Egusa G, Hiro T, Hirobe K, Iida M, Kihara S, Kinoshita M, Maruyama C, Ohta T, Okamura T, Yamashita S, Yokode M, Yokote K, Japan Atherosclerosis Society Committee for Epidemiology and Clinical Management of Atherosclerosis (2014) Diagnosis of atherosclerosis: executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan-2012 version. J Atheroscler Thromb 21:296–298
Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, Umemoto S, Egusa G, Ohmura H, Okamura T, Kihara S, Koba S, Saito I, Shoji T, Daida H, Tsukamoto K, Deguchi J, Dohi S, Dobashi K, Hamaguchi H, Hara M, Hiro T, Biro S, Fujioka Y, Maruyama C, Miyamoto Y, Murakami Y, Yokode M, Yoshida H, Rakugi H, Wakatsuki A, Yamashita S, Committee for Epidemiology and Clinical Management of Atherosclerosis (2018) Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J Atheroscler Thromb 25(9):846–984
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction (2018) Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 72(18):2231–2264
Tanaka N, Kohsaka S, Murata T, Akasaka T, Kadota K, Uemura S, Amano T, Shiode N, Morino Y, Fujii K, Hikichi Y, Nakamura M (2019) Treatment strategy modification and its implication on the medical cost of fractional flow reserve-guided percutaneous coronary intervention in Japan. J Cardiol 73(1):38–44
Hamaya R, Yonetsu T, Kanaji Y, Usui E, Hoshino M, Hada M, Kanno Y, Murai T, Lee T, Kakuta T (2019) Interrelationship in the prognostic efficacy of reginal coronary flow reserve, fractional flow reserve, high-sensitivity cardiac troponin-I and NT-pro BNP in patients with stable coronary artery disease. Heart Vessels 34(3):410–418
Madamanchi NR, Vendrov A, Runge MS (2005) Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol 25(1):29–38
Ley K, Miller YI, Hedrick CC (2011) Monocyte and macrophage dynamics during atherogenesis. Arterioscler Thromb Vasc Biol 31(7):1506–1516
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yokoi, M., Ito, T., Fujita, H. et al. Impact of malondialdehyde-modified low-density lipoprotein on clinical outcomes after fractional flow reserve-guided deferral of revascularization. Heart Vessels 36, 605–614 (2021). https://doi.org/10.1007/s00380-020-01731-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-020-01731-9