Abstract
Purpose
To evaluate the impact of the fiber–tissue distance on histological parameters in a porcine kidney model.
Methods
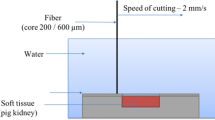
Four lasers were tested at 60 W using a 600-µm bare-ended fiber: a continuous wave (cw) thulium fiber laser (TFL), a super pulsed (SP) TFL, a Ho:YAG laser, and a blue diode laser (BDL). All tissue samples were mounted on a motorized XY-translation stage. The fiber–tissue distance was changed within a range from 0to 6 mm. Ten incisions were made with each laser at each distance. Afterwards, the tissue samples were sliced with a microtome for lactate dehydrogenase staining to determine zones of thermal damage.
Results
In contact mode, the largest incision depth was found for the cw TFL (1.7 ± 0.1 mm) compared to the SP TFL (1.0 ± 0.1 mm), BDL (0.9 ± 0.1 mm) and HoYAG laser (1.1 ± 0.1 mm), respectively. With regard to the coagulative properties, the SP TFL and the Ho:YAG laser showed comparable coagulation depths with 0.7 ± 0.1 and 0.6 ± 0.1 mm, respectively. At 2 mm fiber–tissue distance, the Ho:YAG laser was the only laser that vaporized tissue (incision depth: 0.2 ± 0.1 mm). The BDL was the only laser that caused coagulation at a distance of 3–5 mm.
Conclusion
Our results support the clinical observation that cw TFL must be defocused for best coagulation, while the coagulation depth of the SP TFL remains nearly constant within the range of 0–3 mm. Increasing the distance of the laser fiber to the tissue up to 5 mm did not cause significant differences with regard to coagulation depth using the BDL.


Similar content being viewed by others
References
Herrmann TRW, Liatsikos EN, Nagele U et al (2012) EAU guidelines on laser technologies. Eur Urol 61:783–795. https://doi.org/10.1016/j.eururo.2012.01.010
Bach T, Muschter R, Sroka R et al (2012) Laser treatment of benign prostatic obstruction: basics and physical differences. Eur Urol 61:317–325. https://doi.org/10.1016/j.eururo.2011.10.009
Enikeev D, Okhunov Z, Rapoport L et al (2018) Novel thulium fiber laser for enucleation of prostate: a retrospective comparison with open simple prostatectomy. J Endourol. https://doi.org/10.1089/end.2018.0791
Becker B, Enikeev D, Glybochko P et al (2019) Effect of optical fiber diameter and laser emission mode (cw vs pulse) on tissue damage profile using 1.94 µm Tm:fiber lasers in a porcine kidney model. World J Urol. https://doi.org/10.1007/s00345-019-02944-y
Jiang D-L, Yang Z, Liu G-X et al (2019) A novel 450-nm blue laser system for surgical applications: efficacy of specific laser-tissue interactions in bladder soft tissue. Lasers Med Sci 34:807–813. https://doi.org/10.1007/s10103-018-2668-5
Braun A, Kettner M, Berthold M et al (2018) Efficiency of soft tissue incision with a novel 445-nm semiconductor laser. Lasers Med Sci 33:27–33. https://doi.org/10.1007/s10103-017-2320-9
Traxer O, Rapoport L, Tsarichenko D et al (2018) V03–02 first clinical study on superpulse thulium fiber laser for lithotripsy. J Urol 199:e321–e322. https://doi.org/10.1016/j.juro.2018.02.827
Traxer O, Keller EX (2019) Thulium fiber laser: the new player for kidney stone treatment? A comparison with Holmium:YAG laser. World J Urol. https://doi.org/10.1007/s00345-019-02654-5
Kronenberg P, Traxer O (2019) The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol 8:S398–S417. https://doi.org/10.21037/tau.2019.08.01
Ishikawa I, Okamoto T, Morita S et al (2011) Blue-violet light emitting diode (LED) irradiation immediately controls socket bleeding following tooth extraction: clinical and electron microscopic observations. Photomed Laser Surg 29:333–338. https://doi.org/10.1089/pho.2010.2856
Emiliani E, Talso M, Haddad M et al (2018) The true ablation effect of holmium YAG laser on soft tissue. J Endourol 32:230–235. https://doi.org/10.1089/end.2017.0835
Kang HW, Choi BB (2019) Dependence of laser-induced tissue ablation on optical fiber movements for laser prostatectomy. World J Urol. https://doi.org/10.1007/s00345-019-03019-8
Fried NM, Murray KE (2005) High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol 19:25–31. https://doi.org/10.1089/end.2005.19.25
Cecchetti W, Zattoni F, Nigro F, Tasca A (2004) Plasma bubble formation induced by holmium laser: an in vitro study. Urology 63:586–590. https://doi.org/10.1016/j.urology.2003.09.010
Yaroslavsky I, Kovalenko A, Arkhipova V et al (2018) Comparison of a novel 450-nm laser with Ho:YAG (2100 nm), Tm fiber (1940 nm), and KTP (532 nm) lasers for soft-tissue ablation. In: Kang HW, Chan KF (eds) Therapeutics and diagnostics in urology 2018. SPIE, San Francisco, p 15
Sherwood ME, Flotte TJ (2007) Improved staining method for determining the extent of thermal damage to cells. Lasers Surg Med 39:128–131. https://doi.org/10.1002/lsm.20450
Enikeev D, Netsch C, Rapoport L et al (2019) Novel thulium fiber laser for endoscopic enucleation of the prostate: a prospective comparison with conventional transurethral resection of the prostate. Int J Urol 26:1138–1143. https://doi.org/10.1111/iju.14115
Enikeev D, Glybochko P, Rapoport L et al (2018) Impact of endoscopic enucleation of the prostate with thulium fiber laser on the erectile function. BMC Urol 18:87. https://doi.org/10.1186/s12894-018-0400-1
Cornu J-N, Ahyai S, Bachmann A et al (2015) A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 67:1066–1096. https://doi.org/10.1016/j.eururo.2014.06.017
Johnson DE, Cromeens DM, Price RE (1992) Use of the holmium:YAG laser in urology. Lasers Surg Med 12:353–363
Arkhipova V, Enikeev M, Laukhtina E et al (2019) Ex vivo and animal study of the blue diode laser, Tm fiber laser, and their combination for laparoscopic partial nephrectomy. Lasers Surg Med. https://doi.org/10.1002/lsm.23158
Meskawi M, Hueber P-A, Valdivieso R et al (2019) Complications and functional outcomes of high-risk patient with cardiovascular disease on antithrombotic medication treated with the 532-nm-laser photo-vaporization Greenlight XPS-180 W for benign prostate hyperplasia. World J Urol 37:1671–1678. https://doi.org/10.1007/s00345-018-2560-8
Chen C-H, Chiang P-H, Lee W-C et al (2012) High-intensity diode laser in combination with bipolar transurethral resection of the prostate: a new strategy for the treatment of large prostates (>80 ml). Lasers Surg Med 44:699–704. https://doi.org/10.1002/lsm.22081
Hess MM, Fleischer S, Ernstberger M (2018) New 445 nm blue laser for laryngeal surgery combines photoangiolytic and cutting properties. Eur Arch Otorhinolaryngol 275:1557–1567. https://doi.org/10.1007/s00405-018-4974-8
Funding
No funding was obtained.
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission have contributed sufficiently to the scientific work and therefore, share collective responsibility and accountability for the results. T: project development, data collection, data analysis, manuscript editing. N: project development, data collection, data analysis, manuscript editing. E: project development, data collection, data analysis, manuscript editing. G: project development, manuscript editing. H: project development, manuscript editing. K: project development, manuscript editing. L: project development, data collection, data analysis. G: project development, manuscript editing. B: project development, data collection, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was not necessary in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Taratkin, M., Netsch, C., Enikeev, D. et al. The impact of the laser fiber-tissue distance on histological parameters in a porcine kidney model. World J Urol 39, 1607–1612 (2021). https://doi.org/10.1007/s00345-020-03326-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03326-5