Abstract
Purpose
We aimed to report surgical outcomes in female urethral diverticula and to investigate the risk factors for diverticula recurrence.
Methods
A total of 66 patients underwent urethral diverticulectomies from January 2009 to October 2015 at out institution. Patient and diverticula characteristics were collected. Mean follow-up was 28.8 months (range 4–85 months). Recurrence was defined as requiring a repeat diverticulectomy.
Results
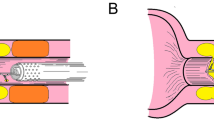
Mean age was 44.9 years. Mean duration of symptoms was 28.1 months. Seven cases had previous urethral surgeries. Mean diverticula size was 2.8 cm. Main clinical symptoms included dribbling (n = 41), vaginal mass (n = 41), dysuria (n = 33), frequency/urgency (n = 29), infection (n = 24), stress urinary incontinence (SUI) (n = 20) and dyspareunia (n = 8). 10 cases had proximal diverticula, 10 cases had multiple diverticula, and 35 cases had horseshoe/circumferential diverticula. Postoperatively, the recurrence rate was 19.7 %. Preoperative SUI disappeared in 14 cases, and de novo SUI was developed in six cases. One case developed urethral stricture, and no cases reported urinary fistula. Among 60 cases with pathological results, neoplastic change was seen in one case (1.7 %). Besides, atypical hyperplasia (n = 2) and metaplasia (n = 3) were observed. Univariate analysis suggested that age, duration, follow-up, diverticula size and diverticula shape were not associated with surgical outcomes. Patients with multiple diverticula (p = 0.032), proximal diverticula (p = 0.042) and those with previous urethral procedures (p = 0.004) were at risk of recurrent diverticula confirmed by multivariate logistic regression analysis.
Conclusions
The surgical outcomes of urethral diverticulectomies were acceptable. Multiple diverticula, proximal diverticula and previous urethral surgery were three independent risk factors for recurrent diverticula.


Similar content being viewed by others
References
Aspera AM, Rackley RR, Vasavada SP (2002) Contemporary evaluation and management of the female urethral diverticulum. Urol Clin North Am 29:617–624
Andersen MJ (1967) The incidence of diverticula in the female urethra. J Urol 98:96–98
Romanzi LJ, Groutz A, Blaivas JG (2000) Urethral diverticulum in women: diverse presentations resulting in diagnostic delay and mismanagement. J Urol 164:428–433
Crescenze IM, Goldman HB (2015) Female urethral diverticulum: current diagnosis and management. Curr Urol Rep 16:71
Han DH, Jeong YS, Choo MS et al (2007) Outcomes of surgery of female urethral diverticula classified using magnetic resonance imaging. Eur Urol 51:1664–1670
Bodner-Adler B, Halpern K, Hanzal E (2015) Surgical management of urethral diverticula in women: a systematic review. Int Urogynecol J. doi:10.1007/s00192-015-2862-y
Ockrim JL, Allen DJ, Shah PJ et al (2009) A tertiary experience of urethral diverticulectomy: diagnosis, imaging and surgical outcomes. BJU Int 103:1550–1554
Reeves FA, Inman RD, Chapple CR (2014) Management of symptomatic urethral diverticula in women: a single-centre experience. Eur Urol 66:164–172
Ingber MS, Firoozi F, Vasavada SP et al (2011) Surgically corrected urethral diverticula: long-term voiding dysfunction and reoperation rates. Urology 77:65–69
Porpiglia F, Destefanis P, Fiori C et al (2002) Preoperative risk factors for surgery female urethral diverticula. Our experience. Urol Int 69:7–11
Greenwell TJ, Spilotros M (2015) Urethral diverticula in women. Nat Rev Urol 12:671–680
Huffman JW (1948) The detailed anatomy of the paraurethral ducts in the adult human female. Am J Obstet Gynecol 55:86–101
Athanasopoulos A, McGuire EJ (2008) Urethral diverticulum: a new complication associated with tension-free vaginal tape. Urol Int 81:480–482
Chang YL, Lin AT (2010) Female urethral diverticula—an update. Urol Sci 21:23–29
Antosh DD, Gutman RE (2011) Diagnosis and management of female urethral diverticulum. Female Pelvic Med Reconstr Surg 17:264–271
Thomas AA, Rackley RR, Lee U et al (2008) Urethral diverticula in 90 female patients: a study with emphasis on neoplastic alterations. J Urol 180:2463–2467
Foster RT, Amundsen CL, Webster GD (2007) The utility of magnetic resonance imaging for diagnosis and surgical planning before transvaginal periurethral diverticulectomy in women. Int Urogynecol J Pelvic Floor Dysfunct 18:315–319
Chou CP, Levenson RB, Elsayes KM et al (2008) Imaging of female urethral diverticulum: an update. Radiographics 28:1917–1930
Acknowledgments
This work was supported by Grant Nos. 81300579, 31370951, 81470927 and 81300579 from the National Natural Science Foundation of China, Grant No. JH2015017 from the Applied Key Project of Sichuan Province, Grant No. JH2014053 from the Foundation for Reserve Candidates of Science and Technology leader of Sichuan Province and Grant No. 2014SCU04B21 from the Foundation for Outstanding Young in Sichuan University, Grant No. 2014SZ0028 from the Support Project of the Ministry of Science and Technology of Sichuan Province and 1.3.5. Project for disciplines of excellence, West China Hospital, Sichuan University.
Authors’ contribution
Liang Zhou was involved in data collection, data analysis, manuscript writing and follow-up. De-Yi Luo was involved in data collection and manuscript writing. Shi-Jian Feng took part in data analysis. The pathological data and imaging data were collected by Qi Liu and **n Wei, respectively. Yi-Fei Lin and Tao ** were involved in follow-up. Hong Li participated in manuscript revision. Kun-Jie Wang took part in project development and manuscript revision. Hong Shen was involved in project development, manuscript revision and performing surgeries.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Liang Zhou and De-Yi Luo have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhou, L., Luo, DY., Feng, SJ. et al. Risk factors for recurrence in female urethral diverticulectomy: a retrospective study of 66 patients. World J Urol 35, 139–144 (2017). https://doi.org/10.1007/s00345-016-1815-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1815-5