Abstract
Objectives
To explore individual weight of cardiac magnetic resonance (CMR) metrics to predict mid-term outcomes in patients with dilated cardiomyopathy (DCM), and develop a risk algorithm for mid-term outcome based on CMR biomarkers.
Materials and methods
Patients with DCM who underwent CMR imaging were prospectively enrolled in this study. The primary endpoint was a composite of heart failure (HF) death, sudden cardiac death (SCD), aborted SCD, and heart transplantation.
Results
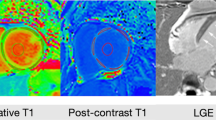
A total of 407 patients (age 48.1 ± 13.8 years, 331 men) were included in the final analysis. During a median follow-up of 21.7 months, 63 patients reached the primary endpoint. NYHA class III/IV (HR = 2.347 [1.073–5.133], p = 0.033), left ventricular ejection fraction (HR = 0.940 [0.909–0.973], p < 0.001), late gadolinium enhancement (LGE) > 0.9% and ≤ 6.6% (HR = 3.559 [1.020–12.412], p = 0.046), LGE > 6.6% (HR = 6.028 [1.814–20.038], p = 0.003), and mean extracellular volume (ECV) fraction ≥ 32.8% (HR = 5.922 [2.566–13.665], p < 0.001) had a significant prognostic association with the primary endpoints (C-statistic: 0.853 [0.810–0.896]). Competing risk regression analyses showed that patients with mean ECV fraction ≥ 32.8%, LGE ≥ 5.9%, global circumferential strain ≥ − 5.6%, or global longitudinal strain ≥ − 7.3% had significantly shorter event-free survival due to HF death and heart transplantation. Patients with mean ECV fraction ≥ 32.8% and LGE ≥ 5.9% had significantly shorter event-free survival due to SCD or aborted SCD.
Conclusion
ECV fraction may be the best independently risk factor for the mid-term outcomes in patients with DCM, surpassing LVEF and LGE. LGE has a better prognostic value than other CMR metrics for SCD and aborted SCD. The risk stratification model we developed may be a promising non-invasive tool for decision-making and prognosis.
Clinical relevance statement
“One-stop” assessment of cardiac function and myocardial characterization using cardiac magnetic resonance might improve risk stratification of patients with DCM. In this prospective study, we propose a novel risk algorithm in DCM including NYHA functional class, LVEF, LGE, and ECV.
Key Points
• The present study explores individual weight of CMR metrics for predicting mid-term outcomes in dilated cardiomyopathy.
• We have developed a novel risk algorithm for dilated cardiomyopathy that includes cardiac functional class, ejection fraction, late gadolinium enhancement, and extracellular volume fraction.
• Personalized risk model derived by CMR contributes to clinical assessment and individual decision-making.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- CMR:
-
Cardiac magnetic resonance
- DCM:
-
Dilated cardiomyopathy
- ECV:
-
Extracellular volume
- EF:
-
Ejection fraction
- GCS:
-
Global circumferential strain
- GLS:
-
Global longitudinal strain
- GRS:
-
Global radial strain
- HF:
-
Heart failure
- HRs:
-
Hazard ratios
- ICD:
-
Implantable cardioverter-defibrillator
- IDI:
-
Integrated discrimination improvement
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricular
- MOLLI:
-
Modified Look–Locker inversion recovery
- NRI:
-
Net reclassification index
- NYHA:
-
New York Heart Association
- ROC:
-
Receiver operating characteristic
- SCD:
-
Sudden cardiac death
References
Puntmann VO, Carr-White G, Jabbour A et al (2016) T1-map** and outcome in nonischemic cardiomyopathy: all-cause mortality and heart failure. JACC Cardiovasc Imaging 9:40–50
Li S, Zhou D, Sirajuddin A et al (2022) T1 map** and extracellular volume fraction in dilated cardiomyopathy: a prognosis study. JACC Cardiovasc Imaging 15:578–590
Halliday BP, Cleland JGF, Goldberger JJ, Prasad SK (2017) Personalizing risk stratification for sudden death in dilated cardiomyopathy: the past, present, and future. Circulation 136:215–231
Heidenreich PA, Bozkurt B, Aguilar D et al (2022) 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 79:e263–e421
Køber L, Thune JJ, Nielsen JC et al (2016) Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med 375:1221–30
Bardy GH, Lee KL, Mark DB et al (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352:225–37
Kadish A, Dyer A, Daubert JP et al (2004) Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 350:2151–8
Canepa M, Fonseca C, Chioncel O et al (2018) Performance of prognostic risk scores in chronic heart failure patients enrolled in the European Society of Cardiology Heart Failure Long-Term Registry. JACC Heart Fail 6:452–462
Pocock SJ, Ariti CA, McMurray JJ et al (2013) Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J 34:1404–13
Pocock SJ, Wang D, Pfeffer MA et al (2006) Predictors of mortality and morbidity in patients with chronic heart failure. Eur Heart J 27:65–75
Levy WC, Mozaffarian D, Linker DT et al (2006) The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation 113:1424–33
Li Y, Xu Y, Li W et al (2023) Cardiac MRI to predict sudden cardiac death risk in dilated cardiomyopathy. Radiology 307:e222552
Di Marco A, Brown PF, Bradley J et al (2021) Improved risk stratification for ventricular arrhythmias and sudden death in patients with nonischemic dilated cardiomyopathy. J Am Coll Cardiol 77:2890–2905
Beltrami CA, Finato N, Rocco M et al (1995) The cellular basis of dilated cardiomyopathy in humans. J Mol Cell Cardiol 27:291–305
Di Marco A, Anguera I, Schmitt M et al (2017) Late gadolinium enhancement and the risk for ventricular arrhythmias or sudden death in dilated cardiomyopathy: systematic review and meta-analysis. JACC Heart Fail 5:28–38
Muser D, Nucifora G, Muser D et al (2021) Prognostic value of nonischemic ringlike left ventricular scar in patients with apparently idiopathic nonsustained ventricular arrhythmias. Circulation 143:1359–1373
Chen W, Qian W, Zhang X et al (2021) Ring-like late gadolinium enhancement for predicting ventricular tachyarrhythmias in non-ischaemic dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 22:1130–1138
Radenkovic D, Weingartner S, Ricketts L, Moon JC, Captur G (2017) T-1 map** in cardiac MRI. Heart Fail Rev 22:415–430
Pinto YM, Elliott PM, Arbustini E et al (2016) Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J 37:1850–8
Zhuang B, Li S, Xu J et al (2020) Age- and sex-specific reference values for atrial and ventricular structures in the validated normal Chinese population: a comprehensive measurement by cardiac MRI. J Magn Reson Imaging 52:1031–1043
Nishimura RA, Otto CM, Bonow RO et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 70:252–289
Hicks KA, Tcheng JE, Bozkurt B et al (2015) 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol 66:403–69
Buxton AE, Calkins H, Callans DJ et al (2006) ACC/AHA/HRS 2006 key data elements and definitions for electrophysiological studies and procedures: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (ACC/AHA/HRS Writing Committee to Develop Data Standards on Electrophysiology). J Am Coll Cardiol 48:2360–96
Kilic A, Mathier MA, Hickey GW et al (2021) Evolving trends in adult heart transplant with the 2018 Heart Allocation Policy Change. JAMA Cardiol 6:159–167
Greenland S (1989) Modeling and variable selection in epidemiologic analysis. Am J Public Health 79:340–9
Hong H, Liu J, Zhu AX (2020) Modeling landslide susceptibility using LogitBoost alternating decision trees and forest by penalizing attributes with the bagging ensemble. Sci Total Environ 718:137231
Alba AC, Agoritsas T, Walsh M et al (2017) Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. Jama 318:1377–1384
Kerr KF, Brown MD, Zhu K, Janes H (2016) assessing the clinical impact of risk prediction models with decision curves: guidance for correct interpretation and appropriate use. J Clin Oncol 34:2534–40
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–772
ausdemSiepen F, Buss SJ, Messroghli D et al (2015) T1 map** in dilated cardiomyopathy with cardiac magnetic resonance: quantification of diffuse myocardial fibrosis and comparison with endomyocardial biopsy. Eur Heart J Cardiovasc Imaging 16:210–6
Li S, Wang Y, Yang W et al (2022) Cardiac MRI risk stratification for dilated cardiomyopathy with left ventricular ejection fraction of 35% or higher. Radiology 306:e213059
Ochs A, Riffel J, Ochs MM et al (2021) Myocardial mechanics in dilated cardiomyopathy: prognostic value of left ventricular torsion and strain. J Cardiovasc Magn Reson 23:136
Pi SH, Kim SM, Choi JO et al (2018) Prognostic value of myocardial strain and late gadolinium enhancement on cardiovascular magnetic resonance imaging in patients with idiopathic dilated cardiomyopathy with moderate to severely reduced ejection fraction. J Cardiovasc Magn Reson 20:36
Kitagawa T, Tatsugami F, Yokomachi K et al (2022) Native myocardial T1 value in predicting 1-year outcomes in patients with nonischemic dilated cardiomyopathy experiencing recent heart failure. Int Heart J 63:531–540
Funding
This study has received funding by the CAMS Innovation Fund for Medical Sciences (CIFMS) (2022-I2M-C&T-B-052), Construction Research Project of Key Laboratory (Cultivation) of Chinese Academy of Medical Sciences (2019PT310025), National Natural Science Foundation of China (Grant Nos. 81971588), and High-level research projects of the National Health Commission (2022-GSP-QZ-5).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Minjie Lu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• prospective
• observational study
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, D., Zhu, L., Wu, W. et al. A novel cardiac magnetic resonance–based personalized risk stratification model in dilated cardiomyopathy: a prospective study. Eur Radiol 34, 4053–4064 (2024). https://doi.org/10.1007/s00330-023-10415-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10415-7