Abstract
Objectives
To establish a diagnostic tree analysis (DTA) model based on computed tomography (CT) findings and clinical information for differential diagnosis of cervical necrotic lymphadenopathy, especially in regions where tuberculous lymphadenitis and Kikuchi disease are common.
Methods
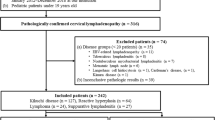
A total of 290 patients (147 men and 143 women; mean age (years), 46.2 ± 19.5; range, 3–91) with pathologically confirmed metastasis (n = 110), tuberculous lymphadenitis (n = 73), Kikuchi disease (n = 71), and lymphoma (n = 36) who underwent contrast-enhanced neck CT were included. The patients were randomly divided into training (86%, 248/290) and validation (14%, 42/290) datasets to assess diagnostic performance of the DTA model. Two sorts of DTA models were created using a classification and regression tree algorithm on the basis of CT findings alone and that combined with clinical findings.
Results
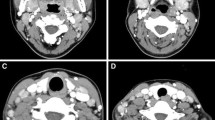
In the DTA model based on CT findings alone, perinodal infiltration, number of the necrotic foci, percentage of necrotic lymph node (LN), degree of necrosis, margin and shape of the necrotic portion, shape of the LN, and enhancement ratio (cutoff value, 1.93) were significant predictors for differential diagnosis of cervical necrotic lymphadenopathy. The overall accuracy was 80.6% and 73.8% in training and validation datasets. In the model based on imaging and clinical findings, tenderness, history of underlying malignancy, percentage of necrotic LN, degree of necrosis, and number of necrotic foci were significant predictors. The overall accuracy was 87.1% and 88.1% in training and external validation datasets.
Conclusions
The DTA model based on CT imaging and clinical findings may be helpful for the diagnosis of cervical necrotic lymphadenopathy.
Key Points
• The diagnostic tree analysis model based on CT may be useful for differential diagnosis of cervical necrotic lymphadenopathy.
• Perinodal infiltration, number of necrotic foci, percentage of necrotic lymph nodes, degree of necrosis, margin and shape of necrotic portion, lymph node shape, and enhancement ratio were the most significant predictors.




Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- CART:
-
Classification and Regression Tree
- CI:
-
Confidence interval
- CNB:
-
Core needle biopsy
- CT:
-
Computed tomography
- DTA:
-
Diagnostic tree analysis
- FNA:
-
Fine needle aspiration
- ICC:
-
Intraclass correlation coefficient
- KD:
-
Kikuchi disease
- LN(s):
-
Lymph node(s)
- Necrotic LNper :
-
Percentage of necrotic lymphadenopathy
- PACS:
-
Picture archival and communication system
- PCR:
-
Polymerase chain reaction
- ROI:
-
Region of interest
- TL:
-
Tuberculous lymphadenitis
References
King AD, Tse GM, Ahuja AT et al (2004) Necrosis in metastatic neck nodes: diagnostic accuracy of CT, MR imaging, and US. Radiology 230:720–726
Koç O, Paksoy Y, Erayman I, Kivrak AS, Arbag H (2007) Role of diffusion weighted MR in the discrimination diagnosis of the cystic and/or necrotic head and neck lesions. Eur J Radiol 62:205–213
Kato H, Kanematsu M, Kato Z et al (2013) Necrotic cervical nodes: usefulness of diffusion-weighted MR imaging in the differentiation of suppurative lymphadenitis from malignancy. Eur J Radiol 82:e28–e35
Zhang Y, Chen J, Shen J, Zhong J, Ye R, Liang B (2013) Apparent diffusion coefficient values of necrotic and solid portion of lymph nodes: differential diagnostic value in cervical lymphadenopathy. Clin Radiol 68:224–231
Eisenmenger LB, Wiggins RH 3rd (2015) Imaging of head and neck lymph nodes. Radiol Clin North Am 53:115–132
Ryoo I, Suh S, Lee YH, Seo HS, Seol HY (2015) Comparison of ultrasonographic findings of biopsy-proven tuberculous lymphadenitis and Kikuchi disease. Korean J Radiol 16:767–775
Han F, Xu M, **e T et al (2018) Efficacy of ultrasound-guided core needle biopsy in cervical lymphadenopathy: a retrospective study of 6,695 cases. Eur Radiol 28:1809–1817
Baek CH, Kim SI, Ko YH, Chu KC (2000) Polymerase chain reaction detection of mycobacterium tuberculosis from fine-needle aspirate for the diagnosis of cervical tuberculous lymphadenitis. Laryngoscope 110:30–34
Mittal P, Handa U, Mohan H, Gupta V (2011) Comparative evaluation of fine needle aspiration cytology, culture, and PCR in diagnosis of tuberculous lymphadenitis. Diagn Cytopathol 39:822–826
Lin HC, Su CY, Huang CC, Hwang CF, Chien CY (2003) Kikuchi’s disease: a review and analysis of 61 cases. Otolaryngol Head Neck Surg 128:650–653
Kucukardali Y, Solmazgul E, Kunter E, Oncul O, Yildirim S, Kaplan M (2007) Kikuchi–Fujimoto disease: analysis of 244 cases. Clin Rheumatol 26:50–54
Baek HJ, Lee JH, Lim HK, Lee HY, Baek JH (2014) Diagnostic accuracy of the clinical and CT findings for differentiating Kikuchi’s disease and tuberculous lymphadenitis presenting with cervical lymphadenopathy. Jpn J Radiol 32:637–643
Lee S, Yoo JH, Lee SW (2012) Kikuchi disease: differentiation from tuberculous lymphadenitis based on patterns of nodal necrosis on CT. AJNR Am J Neuroradiol 33:135–140
Holzapfel K, Duetsch S, Fauser C, Eiber M, Rummeny EJ, Gaa J (2009) Value of diffusion-weighted MR imaging in the differentiation between benign and malignant cervical lymph nodes. Eur J Radiol 72:381–387
Atula TS, Varpula MJ, Kurki TJ, Klemi PJ, Grénman R (1997) Assessment of cervical lymph node status in head and neck cancer patients: palpation, computed tomography and low field magnetic resonance imaging compared with ultrasound-guided fine-needle aspiration cytology. Eur J Radiol 25:152–161
Chong V (2004) Cervical lymphadenopathy: what radiologists need to know. Cancer Imaging 4:116
Wu Q, Zheng D, Shi L, Liu M, Wang M, Shi D (2017) Differentiating metastatic from nonmetastatic lymph nodes in cervical cancer patients using monoexponential, biexponential, and stretched exponential diffusion-weighted MR imaging. Eur Radiol 27:5272–5279
Yousem DM, Som PM, Hackney DB, Schwaibold F, Hendrix RA (1992) Central nodal necrosis and extracapsular neoplastic spread in cervical lymph nodes: MR imaging versus CT. Radiology 182:753–759
van den Brekel MW (2000) Lymph node metastases: CT and MRI. Eur J Radiol 33:230–238
Cui QL, Yin SS, Fan ZH, Yang W, Wang S, Yan K (2018) Diagnostic value of contrast-enhanced ultrasonography and time-intensity curve in differential diagnosis of cervical metastatic and tuberculous lymph nodes. J Ultrasound Med 37:83–92
Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY (2004) CT findings in Kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol 25:1099–1102
Na DG, Chung TS, Byun HS, Kim HD, Ko YH, Yoon JH (1997) Kikuchi disease: CT and MR findings. AJNR Am J Neuroradiol 18:1729–1732
Onciu M, Medeiros LJ (2003) Kikuchi-Fujimoto lymphadenitis. Adv Anat Pathol 10:204–211
Tilak SP, Howard JM (1964) The influence of the dual circulation on the viability of lymph nodes following interruption of their blood or lymphatic supply. Surg Gynecol Obstet 119:349–352
Saito A, Takashima S, Takayama F, Kawakami S, Momose M, Matsushita T (2001) Spontaneous extensive necrosis in non-Hodgkin lymphoma: prevalence and clinical significance. J Comput Assist Tomogr 25:482–486
Adams HJA, De Klerk JMH, Fijnheer R, Dubois SV, Nievelstein RAJ, Kwee TC (2015) Prognostic value of tumor necrosis at CT in diffuse large B-cell lymphoma. Eur J Radiol 84:372–377
Chamulak GA, Brynes RK, Nathwani BN (1990) Kikuchi-Fujimoto disease mimicking malignant lymphoma. Am J Surg Pathol 14:514–523
Dorfman RF, Berry GJ (1988) Kikuchi’s histiocytic necrotizing lymphadenitis: an analysis of 108 cases with emphasis on differential diagnosis. Semin Diagn Pathol 5:329–345
Bosch X, Guilabert A, Miquel R, Campo E (2004) Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol 122:141–152
Kim KN, Kim DW, Kim HJ, Park JH, Kim CS, Kim HS (1999) CT findings of Kikuchi disease: correlation with pathologic findings. J Korean Radiol Soc 41:879–884
Kato H, Kanematsu M, Kato Z et al (2011) MR imaging findings of cervical lymphadenopathy in patients with Kikuchi disease. Eur J Radiol 80:e576–e581
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Byungjun Kim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 5973 kb)
Rights and permissions
About this article
Cite this article
You, SH., Kim, B., Yang, KS. et al. Cervical necrotic lymphadenopathy: a diagnostic tree analysis model based on CT and clinical findings. Eur Radiol 29, 5635–5645 (2019). https://doi.org/10.1007/s00330-019-06155-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06155-2