Abstract
COVID-19 raised concern regarding cardiotoxicity and QTc prolongation of hydroxychloroquine (HCQ) and chloroquine (CQ). We examined the frequency and patient factors associated with ECG testing and the detection of prolonged QTc among new HCQ/CQ users in a large academic medical system. 10,248 subjects with a first HCQ/CQ prescription (1/2015–3/2020) were included. We assessed baseline (1 year prior to and including day of initiation of HCQ/CQ through 2 months after initial HCQ/CQ prescription) and follow-up (10 months after the baseline period) patient characteristics and ECGs obtained from electronic health records. Among 8384 female HCQ/CQ new users, ECGs were obtained for 22.3%, 14.3%, and 7.6%, at baseline, follow, and both periods, respectively. Among 1864 male HCQ/CQ new users, ECGs were obtained more frequently at baseline (29.7%), follow-up (18.0%), and both periods (11.3%). Female HCQ/CQ users with a normal QTc at baseline but prolonged QTc (> 470 ms) at follow-up (13.1%) were older at HCQ/CQ initiation [mean 64.7 (SD 16.5) vs. 58.7 (SD 16.9) years, p = 0.004] and more likely to have history of myocardial infarction (41.0% vs. 21.6%, p = 0.0003) compared to those who had normal baseline and follow-up QTc. The frequency of prolonged QTc development was similar (12.4%) among male HCQ/CQ new users (> 450 ms). Prior to COVID-19, ECG testing before and after HCQ/CQ prescription was infrequent, particularly for females who are disproportionately affected by rheumatic diseases and were just as likely to develop prolonged QTc (> 1/10 new users). Prospective studies are needed to guide future management of HCQ/CQ therapy in rheumatic populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydroxychloroquine (HCQ) and chloroquine (CQ) are essential therapies for the treatment of autoimmune diseases including systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) [1]. In patients with SLE, HCQ has been shown to reduce flares, organ damage, pregnancy complications, and HCQ is the only medication proven to improve survival [2,3,4]. It is thought that all SLE patients should be taking HCQ or CQ unless there is a clear reason not to.
Although there is a wide range of HCQ toxicity, past attention has been on retinal toxicity and monitoring [5]. Potential cardiovascular adverse effects of HCQ and CQ use include cardiomyopathy, arrhythmias, and conduction system abnormalities, including prolonged QTc interval [6]. The prevalence of induced arrhythmias was brought into question during the COVID-19 pandemic when HCQ and CQ were initially used as potential treatments for COVID-19. HCQ COVID-19 clinical trials were halted because of concerns about potential heart rhythm problems especially when HCQ/CQ are taken in combination with other common medications such as antibiotics and anti-depressants [7]. Prior to COVID-19, cardiac monitoring was not routinely performed when initiating a patient on HCQ/CQ or in follow-up with some evidence suggesting that these medications may in fact have cardiovascular benefit [8, 9].
To understand how patients were being monitored for prolonged QTc while on HCQ/CQ, we retrospectively examined using initial HCQ/CQ prescriptions in a large academic medical system prior to the pandemic: 1) ECG testing frequency prior to and during the first year of HCQ/CQ initiation, 2) patient clinical and demographic factors that were associated with likelihood of ECG testing, and 3) the frequency and risk factors for the development of new prolonged QTc at follow-up.
Methods
Data source and study population
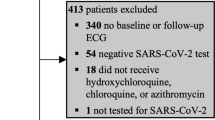
We identified our patients using an administrative dataset, the Research Patient Data Registry (RPDR), a centralized clinical data warehouse from Partners Healthcare system, linked with electronic medical records from the Mass General Brigham, Faulkner, Newton Wellesley hospitals. We included patients ≥ 18-years-old at the start of the baseline period with a new prescription of HCQ or CQ between January 1, 2015-March 1, 2020. This study was approved by the Mass General Brigham Institutional Review Board.
Study design
A patient was a new initiator of HCQ/CQ if they did not have a prescription for either medication for 12 months prior to the initial HCQ/CQ prescription. Therefore, the baseline period was defined as one year prior to and including day of initiation of HCQ/CQ and 2 months after HCQ/CQ (Supplemental Figure). Two months was chosen given the long half-life of HCQ and requirement to obtain steady state. The follow-up period was defined as 10 months after HCQ/CQ first prescribed. At baseline, patient demographics [age, sex, race, body mass index (BMI), medical insurance type] were collected. On the date of the first HCQ/CQ prescription, we searched for ICD-9/10 diagnostic codes (Supplemental table) for several autoimmune rheumatic diseases (e.g., cutaneous SLE, discoid, and other cutaneous lupus rash) and others (osteoarthritis, other joint disorder, other soft tissue disorders). We also identified concomitant diagnoses of myocardial infarction (MI), stroke, and hypothyroidism that may affect the results of the ECG.
Using the RPDR database, we obtained 12-lead resting ECGs that were performed during the baseline or follow-up period for each new initiator of HCQ/CQ. If there was more than one ECG identified during a period for a patient, then we used the closest ECG prior to starting HCQ/CQ. Machine-assisted ECG interpretations were used including assessment of the corrected QT (QTc). A QTc over the 99th percentile is considered abnormally prolonged [10, 11], which is defined as > 470 ms for females and > 450 ms for males in this study. We excluded the following ECGs: those that were interpreted as having prolonged QRS (QRS > 120 ms), the PR interval was missing, right or left bundle branch block, intraventricular conduction delay, atrial fibrillation, ventricular tachycardia, premature ventricular contraction, or premature ventricular beat. We also excluded ECGs where the QTc was not machine interpreted.
Statistical analysis
As the definition of QTc interval prolongation differs by sex, females and males were analyzed separately. The frequency of ECGs performed during the baseline or follow-up among new initiators of HCQ/CQ was calculated. Using chi-square test or t-test, we compared the demographic characteristics (age, race/ethnicity, BMI), co-morbidities (MI, stroke, hypothyroidism), medical insurance type, and rheumatological indication for HCQ/CQ between those who had an ECG vs. those that did not have an ECG during baseline or follow-up periods. The same analysis was performed for patients who had ECGs performed during both baseline and follow-up periods compared to patients who had neither performed. Among those patients who had both baseline and follow-up ECGs performed, the frequency of those who had normal QTc at baseline but then develop prolonged QTc was calculated and compared to those who had normal QTc during both periods. In a sensitivity analysis, the frequency of those who had normal QTc at baseline but then develop prolonged QTc was calculated using a modified baseline period where the two-month HCQ/CQ waiting period was moved into the follow-up period. To determine the predictors of prolonged QTc at follow-up, we performed a logistic regression model for females and males adjusting for age, race, BMI, prior MI, stroke, hypothyroidism, disease indication for HCQ/CQ. A p < 0.05 was considered statistically significant. Analyses were conducted using SAS software, version 9.4 (SAS Institute, Cary, NC).
Results
Study population
There was a total of 10,248 subjects with a new prescription of HCQ/CQ which included patients with RA (2919/10,248, 28.5%), SLE (1478/10,248, 14.4%), and other (6214/10,248, 60.6%). The number of patients prescribed HCQ was 10,221 (99.74%); 27 (0.26%) were prescribed CQ.
Frequency of ECG testing
Among all new HCQ/CQ users, 2424 (23.7%) had a baseline ECG and 1539 (15.0%) had a follow-up ECG, while only 844 (8.2%) had both. Among female HCQ/CQ new users, ECGs were obtained for 22.3% (1871/8384) during the baseline, 14.3% (1203/8384) follow-up, 7.6% (634/8384) both periods (Table 1). Those who were older at HCQ/CQ initiation, had a higher BMI, history of MI, stroke, hypothyroidism, or rheumatic disorder were more likely to have ECGs during baseline, follow-up, or both. Race and medical insurance type were also associated with ECG testing. ECGs were more frequently performed for male HCQ/CQ new users; baseline (29.7%, 553/1864), follow-up (18.0%, 336/1864), and both periods (11.3%, 210/1864) (Table 2). Males who were older at HCQ/CQ initiation, had a history of MI, stroke, hypothyroidism, or rheumatic disorder were more likely to have ECGs during baseline, follow-up, or both. Medical insurance type was also associated with ECG testing.
Prolonged QTc
Among those who had both baseline and follow-up ECGs, 13.1% (83/634) and 12.4% (26/210) for female and male new HCQ/CQ users had normal QTc at baseline but then developed prolonged QTc at follow-up (Table 3). In a sensitivity analysis where the 2-month HCQ/CQ initiation period was moved from the baseline period to the follow-up period, an even higher proportion of individuals had a normal baseline but prolonged follow-up QTc [20.5% (104/507) for females and 33.1% (41/124) for males] was observed. Among 190 females with prolonged QTc at baseline, 113 (59.5%) continued to have prolonged QTc, 77 (40.5%) returned to normal QTc at follow-up. Among 103 males with prolonged QTc at baseline, 79 (76.7%) still had prolonged QTc, 24 (23.3) returned to a normal QTc at follow-up. For the 246 males with prolonged QTc at baseline, 54 (22.0%) used HCQ/CQ for the entire follow-up period (12 months). The mean for the duration of HCQ/CQ use was 4.5 (SD 4.6) months.
When compared to new HCQ/CQ users who did not develop prolonged QTc (54.9% or 348/634 for females, 36.7% or 77/210 for males), females who were older at HCQ/CQ initiation [mean 64.7 (SD 16.5) vs. 58.7 (SD 16.9) years, p = 0.004] and more likely to have had an MI (41.0% vs. 21.6%, p = 0.0003) were more likely to develop prolonged QTc. There were no significant differences among the males. In the adjusted logistic regression model for females, age [odds ratio (OR) 1.01, 95% confidence interval (CI): 1.00–1.02] and prior MI (OR 2.52, 95% CI: 1.69–3.76) were significantly associated with the prolonged QTc in follow-up. For males, prior MI (OR 1.97, 95% CI: 1.10–3.52) was significantly associated with prolonged QTc in follow-up. The other factors race/ethnicity, BMI, stroke, hypothyroidism and disease indication for HCQ/CQ were not significant predictors.
Discussion
Prior to the COVID-19 pandemic, there was less awareness and regard for potential arrhythmias due to HCQ/CQ, largely because for decades, rheumatologists and dermatologists have been prescribing HCQ/CQ with no “obvious” cardiac safety signal. However, in retrospect, this is difficult to accept at face value if cardiac monitoring has not been routinely performed on patients on HCQ/CQ and most patients with prolonged QTc are asymptomatic. In this large retrospective analysis using linked administrative data from 2015 to 2020 (prior to the pandemic), we showed that ECGs were infrequently obtained prior to initiation of HCQ/CQ and even less so within 1 year in follow-up. ECGs were more likely to be ordered in patients already at high risk for arrhythmias, such as those with a history of MI, therefore, even when an ECG was ordered, it was likely for reasons other than to monitor for HCQ/CQ cardiotoxicity. We also identified a potential gap in care among women because although majority of new HCQ/CQ users were women and their risk of develo** prolonged QTc was similar to that of men, women were less likely to have ECG testing.
The sex difference in prolonged QTc may be explained by intrinsic cardiac electrophysiological differences between women and men. In one study using rabbits as an animal model, oophorectomy shortened QT interval while estradiol replacement lengthened the QT interval, suggesting a potential role for sex hormones [12]. Also, female rabbit ventricular myocytes have lower outward potassium currents, which determine the repolarization phase of the cardiac action potential, and current densities in the heart compared to males [13]. In a systemic review and meta-analysis that included 332 cases of torsades de pointe (TdP) associated with cardiovascular drugs that prolonged QTc, 70% (95% CI: 64–75%) were women even after adjusting for other TdP risk factors [14], suggesting that women are inherently more sensitive to drug-induced arrhythmias.
To compound the issue, rheumatic diseases such as RA and SLE increase the risk of cardiovascular disease and events such as MI, a risk factor also associated with prolonged QTc. In our study, age and prior MI were independently associated with prolonged QTc at follow-up among females and prior MI was the only predictor of prolonged QTc at follow-up among males. Indeed, a recent white paper conducted by a working group of experts spanning different subspecialties, suggested that clinicians should be aware of the potential risk of cardiotoxicity of HCQ/CQ and consider a risk and benefit assessment prior to initiation of these medications [15]. Many studies examining the risk of arrhythmia with HCQ use among SLE and RA patients, several sparked by the COVID-19 pandemic [16,17,18,19,20], are still in abstract form, limited to retrospective analysis, using electronic medical records, and/or based on small cohorts [21]. To avoid systematic biases in retrospective analyses, prospective studies of consecutive patients should be conducted to determine the impact of HCQ/CQ therapy on QTc prolongation and adverse events in patients with rheumatic diseases.
The strength of this study include that we utilized a large administrative database with detailed ECG data that allowed us to exclude cases where QTc intervals were uninterpretable. There were several limitations in this study including inability to determine the precise indication for which the ECGs were ordered, the doses of HCQ/CQ, and we did not examine other QTc prolonging medications and co-morbidities. There were also some patients who had a diagnostic code (e.g., osteoarthritis, fibromyalgia) where HCQ/CQ is not indicated. These patients likely had multiple rheumatological diagnoses, but we could not confirm the exact indication for the HCQ/CQ. It is also possible that some of these patients were started on a trial of HCQ/CQ prior to receiving a rheumatological diagnosis where HCQ/CQ is indicated. We also acknowledge that although HCQ has a prolonged half-life of 40–50 days, the effect of HCQ/CQ on QTc may happen as early as 2 days after starting the medications and that even among similar dosing in mg/kg/day, there is variability in HCQ blood levels [22,23,24]. We used the 2-month waiting period as recommended by the white paper on HCQ antimalarial HCQ/CQ toxicity [15]. Therefore, by including the 2-month after HCQ/CQ initiation period as part of the baseline period, there may have been some patients who developed prolonged QTc during the baseline period. It is also possible that patients with prior QTc prolongation would likely not be captured in our study because they would not be initiated on HCQ/CQ. Patients who developed TdP and sudden cardiac death who did not make it to the hospital, would also not be captured in our study. The study population was predominantly White and female, limiting generalizability of the results. Future studies in more diverse populations compared with non-rheumatic disease controls are needed.
In summary, the frequency of ECG testing before and after HCQ/CQ prescription was low in a large academic medical center prior to the COVID-19 pandemic. This was particularly true among women, a population more likely to be prescribed HCQ/CQ as they are disproportionately affected by rheumatic diseases. As discussed, there were limitations to this study including selection bias. Therefore, to ascertain the true risk of QT prolongation of HCQ/CQ to inform clinicians in the management of rheumatic conditions, future prospective studies are needed.
Data availability statement
All data relevant to the study are included in the article.
References
Rempenault C, Combe B, Barnetche T, Gaujoux-Viala C, Lukas C, Morel J, Hua C (2020) Clinical and structural efficacy of hydroxychloroquine in rheumatoid arthritis: a systematic review. Arthritis Care Res (Hoboken) 72(1):36–40. https://doi.org/10.1002/acr.23826
Siso A, Ramos-Casals M, Bove A, Brito-Zeron P, Soria N, Munoz S, Testi A, Plaza J, Sentis J, Coca A (2008) Previous antimalarial therapy in patients diagnosed with lupus nephritis: influence on outcomes and survival. Lupus 17(4):281–288. https://doi.org/10.1177/0961203307086503
Pons-Estel GJ, Alarcon GS, McGwin G, Jr., Danila MI, Zhang J, Bastian HM, Reveille JD, Vila LM, Lumina Study G (2009) Protective effect of hydroxychloroquine on renal damage in patients with lupus nephritis: LXV, data from a multiethnic US cohort. Arthritis Rheum 61(6):830–839. https://doi.org/10.1002/art.24538
Ruiz-Irastorza G, Ramos-Casals M, Brito-Zeron P, Khamashta MA (2010) Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: a systematic review. Ann Rheum Dis 69(1):20–28. https://doi.org/10.1136/ard.2008.101766
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, Cervera R, Doria A, Gordon C, Govoni M, Houssiau F, Jayne D, Kouloumas M, Kuhn A, Larsen JL, Lerstrom K, Moroni G, Mosca M, Schneider M, Smolen JS, Svenungsson E, Tesar V, Tincani A, Troldborg A, van Vollenhoven R, Wenzel J, Bertsias G, Boumpas DT (2019) 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 78(6):736–745. https://doi.org/10.1136/annrheumdis-2019-215089
Meeting WERG (2017) World Health Organization. The cardiotoxicity of antimalarials: Malaria Policy Advisory Committee Meeting. https://www.who.int/malaria/mpac/mpac-mar2017-erg-cardiotoxicity-report-session2.pdf. Accessed 21 Apr 2020
Cavalcanti AB, Zampieri FG, Rosa RG, Azevedo LCP, Veiga VC, Avezum A, Damiani LP, Marcadenti A, Kawano-Dourado L, Lisboa T, Junqueira DLM, de Barros ESPGM, Tramujas L, Abreu-Silva EO, Laranjeira LN, Soares AT, Echenique LS, Pereira AJ, Freitas FGR, Gebara OCE, Dantas VCS, Furtado RHM, Milan EP, Golin NA, Cardoso FF, Maia IS, Hoffmann Filho CR, Kormann APM, Amazonas RB, Bocchi de Oliveira MF, Serpa-Neto A, Falavigna M, Lopes RD, Machado FR, Berwanger O, Coalition Covid-19 Brazil II (2020) Hydroxychloroquine with or without azithromycin in mild-to-moderate covid-19. N Engl J Med 383(21):2041–2052. https://doi.org/10.1056/NEJMoa2019014
Rempenault C, Combe B, Barnetche T, Gaujoux-Viala C, Lukas C, Morel J, Hua C (2018) Metabolic and cardiovascular benefits of hydroxychloroquine in patients with rheumatoid arthritis: a systematic review and meta-analysis. Ann Rheum Dis 77(1):98–103. https://doi.org/10.1136/annrheumdis-2017-211836
Liu D, Li X, Zhang Y, Kwong JS, Li L, Zhang Y, Xu C, Li Q, Sun X, Tian H, Li S (2018) Chloroquine and hydroxychloroquine are associated with reduced cardiovascular risk: a systematic review and meta-analysis. Drug Des Devel Ther 12:1685–1695. https://doi.org/10.2147/DDDT.S166893
Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, Gorgels A, Hancock EW, Josephson M, Kligfield P, Kors JA, Macfarlane P, Mason JW, Mirvis DM, Okin P, Pahlm O, van Herpen G, Wagner GS, Wellens H, American Heart Association E, Arrhythmias Committee CoCC, American College of Cardiology F, Heart Rhythm S (2009) AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation 119(10):e241-250. https://doi.org/10.1161/CIRCULATIONAHA.108.191096
Drew BJ, Ackerman MJ, Funk M, Gibler WB, Kligfield P, Menon V, Philippides GJ, Roden DM, Zareba W, American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology tCoCN, the American College of Cardiology F (2010) Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation 121(8):1047–1060. https://doi.org/10.1161/CIRCULATIONAHA.109.192704
Drici MD, Burklow TR, Haridasse V, Glazer RI, Woosley RL (1996) Sex hormones prolong the QT interval and downregulate potassium channel expression in the rabbit heart. Circulation 94(6):1471–1474. https://doi.org/10.1161/01.cir.94.6.1471
Liu XK, Katchman A, Drici MD, Ebert SN, Ducic I, Morad M, Woosley RL (1998) Gender difference in the cycle length-dependent QT and potassium currents in rabbits. J Pharmacol Exp Ther 285(2):672–679
Makkar RR, Fromm BS, Steinman RT, Meissner MD, Lehmann MH (1993) Female gender as a risk factor for torsades de pointes associated with cardiovascular drugs. JAMA 270(21):2590–2597. https://doi.org/10.1001/jama.270.21.2590
Desmarais J, Rosenbaum JT, Costenbader KH, Ginzler EM, Fett N, Goodman S, O’Dell J, Pineau CA, Schmajuk G, Werth VP, Link MS, Kovacs R (2021) American college of rheumatology white paper on antimalarial cardiac toxicity. Arthritis Rheumatol 73(12):2151–2160. https://doi.org/10.1002/art.41934
Haj-Ali M, Belmont HM (2020) Hydroxychloroquine and QTc prolongation in a cohort of SLE patients [abstract]. Arthritis Rheumatol 72(10)
Renaldi J, Koumpouras F, Dong MX (2020) Evaluating the risk of QT-prolongation associated with hydroxychloroquine use with and without antidepressants in SLE patients with fibromyalgia [abstract]. Arthritis Rheumatol 72(10)
Restrepo JF, Escalante A, Battafarano D, Lorenzo C, Del Rincon I (2020) Hydroxychloroquine is not cardiotoxic in patients with rheumatoid arthritis [abstract]. Arthritis Rheumatol 72(10)
Nishiyama T, Kondo Y, Tsuboi H, Tabuchi D, Sugita T, Okamoto S, Terasaki T, Shimizu M, Honda F, Ohyama A, Kurata I, Yagishita M, Abe S, Takahashi H, Osada A, Hagiwara S, Matsumoto I, Sumida T, Noma H (2021) QTc interval prolongation in patients with systemic lupus erythematosus treated with hydroxychloroquine. Mod Rheumatol. https://doi.org/10.1080/14397595.2021.1879368
Azharudeen M, Thabah MM, Satheesh S, Negi VS (2020) QT interval parameters, anti-Ro antibody status, and disease activity in systemic lupus erythematosus. J R Coll Physicians Edinb 50(4):380–386. https://doi.org/10.4997/JRCPE.2020.406
Chatre C, Roubille F, Vernhet H, Jorgensen C, Pers YM (2018) Cardiac complications attributed to chloroquine and hydroxychloroquine: a systematic review of the literature. Drug Saf 41(10):919–931. https://doi.org/10.1007/s40264-018-0689-4
Bustos MD, Gay F, Diquet B, Thomare P, Warot D (1994) The pharmacokinetics and electrocardiographic effects of chloroquine in healthy subjects. Trop Med Parasitol 45(2):83–86
Tett SE, Cutler DJ, Day RO, Brown KF (1989) Bioavailability of hydroxychloroquine tablets in healthy volunteers. Br J Clin Pharmacol 27(6):771–779. https://doi.org/10.1111/j.1365-2125.1989.tb03439.x
Petri M, Elkhalifa M, Li J, Magder LS, Goldman DW (2020) Hydroxychloroquine blood levels predict hydroxychloroquine retinopathy. Arthritis Rheumatol 72(3):448–453. https://doi.org/10.1002/art.41121
Acknowledgements
There were no external editing agencies in writing or submitting the manuscript.
Funding
K.C is funded, in part, by an NIH K24 AR066109. B.W. is funded, in part, by an NIH training grant T32 HL094301 and American Heart Association Career Development Grant (Dallas, TX) 21CDA851511. M.C. is funded, in part, by a Gary Gilkeson Career Development Award from the Lupus Foundation of America.
Author information
Authors and Affiliations
Contributions
M.C. and B.W. are co-first authors. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work: all authors. Drafting the work or revising it critically for important intellectual content: all authors. Final approval of the version to be published: all authors. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: all authors.
Corresponding author
Ethics declarations
Conflict of interest
Dr. May Choi has received consulting fees from Janssen, Astra Zeneca, and MitogenDx. Dr. Costenbader has consulted for or collaborated on research projects with Janssen, Glaxo Smith Kline, Exagen Diagnostics, Eli Lilly, Merck Serono, Astra Zeneca and Neutrolis (less than $10,000 each). Marcelo DiCarli reports grants from Gilead and Spectrum Dynamics. Usha Tedrow has received teaching honoraria from Biosense Webster, Boston Scientific and Abbott medical, consulting monies from Thermedical Inc. related to a specialized ablation catheter. All other authors have no relevant disclosures.
Ethics statement
This research involves human participants. An Institutional Review Board of Brigham and Women’s Hospital approved all aspects of this study (IRB 2020-P-002154).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, M.Y., Weber, B., Stevens, E. et al. Prevalence of ECG testing and characteristics among new hydroxychloroquine and chloroquine users within a multi-center tertiary care center. Rheumatol Int 42, 1767–1774 (2022). https://doi.org/10.1007/s00296-022-05125-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05125-0