Abstract
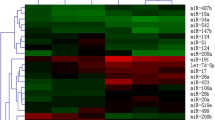
MicroRNAs, or miRNAs, may involve in coagulation and inflammation pathways caused by severe Coronavirus disease (COVID-19). Accordingly, this attempt was made to explore the behavior of peripheral blood mononuclear cells (PBMCs) miRNAs as effective biomarkers to diagnose COVID-19 patients with normal and abnormal coagulation indices. We selected the targeted miRNAs (miR-19a-3p, miR-223-3p, miR-143-5p, miR-494-3p and miR-301a-5p) according to previous reports, whose PBMC levels were then determined by real-time PCR. Receiver operating characteristic (ROC) curve was obtained to clarify the diagnostic potency of studied miRNAs. The differentially expressed miRNA profiles and corresponding biological activities were predicted in accordance with bioinformatics data. Targeted miRNAs' expression profiles displayed a significant difference between COVID-19 subjects with normal and abnormal coagulation indices. Moreover, the average miR-223-3p level expressed in COVID-19 cases with normal coagulation indices was significantly lower than that in healthy controls. Based on data from ROC analysis, miR-223-3p and miR-494-3p are promising biomarkers to distinguish the COVID-19 cases with normal or abnormal coagulation indices. Bioinformatics data highlighted the prominent role of selected miRNAs in the inflammation and TGF-beta signaling pathway. The differences existed in the expression profiles of selected miRNAs between the groups introduced miR-494-3p and miR-223-3p as potent biomarkers to prognosis the incidence of COVID-19.





Similar content being viewed by others
Abbreviations
- qRT-PCR:
-
Quantitative real-time polymerase chain reactions
- COVID-19:
-
Coronavirus disease of 2019
- ROC:
-
Receiver operating characteristic
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- ssRNA:
-
Single-strand RNA viruses
- ARDS:
-
Acute respiratory distress syndrome
- ACE2:
-
Angiotensin-converting enzyme 2
- TNF-α:
-
Tumor necrosis factor alpha
- DIC:
-
Disseminated intravascular coagulation
- TF:
-
Tissue factor
- NF-κB:
-
Nuclear factor kappa-light-chain-enhancer of activated B cells
- IL-2:
-
Interleukin-2
- RdRp:
-
RNA-dependent RNA polymerase
- STRING:
-
Search tool for the retrieval of interacting genes/proteins
- IFITM1:
-
IFN-induced transmembrane protein 1
- STAT:
-
Signal transducer and activator of transcription
- RIG-I:
-
Retinoic acid-inducible gene I
- ZMAT3:
-
Zinc finger matrin-type 3
- MXD1:
-
MAX dimerization protein 1
- ESR1:
-
Estrogen receptor 1
- RRAGD:
-
Ras related GTP binding D
- NFIA:
-
Nuclear factor I A
References
Rasizadeh R, Baghi HB (2023) Increase in rabies cases during COVID-19 pandemic: Is there a connection? J Infect Dev Count 17:335–336
Eslami N, Aghbash PS, Shamekh A, Entezari-Maleki T, Nahand JS, Sales AJ, Baghi HB (2022) SARS-CoV-2: receptor and co-receptor tropism probability. Curr Microbiol 79:1–13
Hamidi Z, Jabraeili-Siahroud S, Taati-Alamdari Y, Aghbash PS, Shamekh A, Baghi HB (2023) A comprehensive review of COVID-19 symptoms and treatments in the setting of autoimmune diseases. Virology Journal 20:1–11
Hong L-Z, Shou Z-X, Zheng D-M, ** X (2021) The most important biomarker associated with coagulation and inflammation among COVID-19 patients. Mol Cell Biochem 476:2877–2885
Farzi R, Aghbash PS, Eslami N, Azadi A, Shamekh A, Hemmat N, Entezari-Maleki T, Baghi HB (2022) The role of antigen-presenting cells in the pathogenesis of COVID-19. Pathol Res Pract 233:153848
Biswas S, Thakur V, Kaur P, Khan A, Kulshrestha S, Kumar P (2021) Blood clots in COVID-19 patients: simplifying the curious mystery. Med Hypotheses 146:110371
Connors JM, Levy JH (2020) COVID-19 and its implications for thrombosis and anticoagulation. Blood 135:2033–2040
Atallah B, Mallah SI, AlMahmeed W (2020) Anticoagulation in COVID-19. Eur Heart J Cardiovasc Pharmacotherapy 6:260–261
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506
Boroumand H, Badie F, Mazaheri S, Seyedi ZS, Nahand JS, Nejati M, Baghi HB, Abbasi-Kolli M, Badehnoosh B, Ghandali M (2021) Chitosan-based nanoparticles against viral infections. Front Cell Infect Microbiol 11:643953
Hum C, Loiselle J, Ahmed N, Shaw TA, Toudic C, Pezacki JP (2021) MicroRNA mimics or inhibitors as antiviral therapeutic approaches against COVID-19. Drugs 81:517–531
Momekov G, Momekova D (2020) Ivermectin as a potential COVID-19 treatment from the pharmacokinetic point of view: antiviral levels are not likely attainable with known dosing regimens. Biotechnol Biotechnol Equip 34:469–474
Hemmat N, Mokhtarzadeh A, Aghazadeh M, Jadidi-Niaragh F, Baradaran B, Bannazadeh Baghi H (2020) Role of microRNAs in epidermal growth factor receptor signaling pathway in cervical cancer. Mol Biol Rep 47:4553–4568
Donyavi T, Bokharaei-Salim F, Baghi HB, Khanaliha K, Janat-Makan MA, Karimi B, Nahand JS, Mirzaei H, Khatami A, Garshasbi S (2021) Acute and post-acute phase of COVID-19: analyzing expression patterns of miRNA-29a-3p, 146a-3p, 155-5p, and let-7b-3p in PBMC. Int Immunopharmacol 97:107641
Jankowska KI, Sauna ZE, Atreya CD (2020) Role of microRNAs in hemophilia and thrombosis in humans. Int J Mol Sci 21:3598
Vossen CY, van Hylckama VA, Teruel-Montoya R, Salloum-Asfar S, de Haan H, Corral J, Reitsma P, Koeleman BP, Martínez C (2017) Identification of coagulation gene 3′ UTR variants that are potentially regulated by microRNAs. Br J Haematol 177:782–790
Ali HO, Arroyo AB, González-Conejero R, Stavik B, Iversen N, Sandset PM, Martínez C, Skretting G (2016) The role of microRNA-27a/b and microRNA-494 in estrogen-mediated downregulation of tissue factor pathway inhibitor α. J Thromb Haemost 14:1226–1237
Yu X (2021) Another new application of heparin in COVID-19: more than anticoagulation and antiviral. J Invest Med 69:1258
Zhang X, Yu H, Lou JR, Zheng J, Zhu H, Popescu N-I, Lupu F, Lind SE, Ding W-Q (2011) MicroRNA-19 (miR-19) regulates tissue factor expression in breast cancer cells. J Biol Chem 286:1429–1435
Li S, Chen H, Ren J, Geng Q, Song J, Lee C, Cao C, Zhang J, Xu NJA (2014) MicroRNA-223 inhibits tissue factor expression in vascular endothelial cells. Atherosclerosis 237:514–520
Eisenreich A, Rauch U (2013) Regulation of the tissue factor isoform expression and thrombogenicity of HMEC-1 by miR-126 and miR-19a. Cell Biol: Res Ther 2(1):2
Zhang R, Lu S, Yang X, Li M, Jia H, Liao J, **g Q, Wu Y, Wang H, **ao F (2021) miR-19a-3p downregulates tissue factor and functions as a potential therapeutic target for sepsis-induced disseminated intravascular coagulation. Biochem Pharmacol 192:114671
Haneklaus M, Gerlic M, O’Neill LA, Masters S (2013) miR-223: infection, inflammation and cancer. J Intern Med 274:215–226
Edén D (2020) Tissue factor regulation, signaling and functions beyond coagulation with a focus on diabetes. Dissertation, Acta Universitatis Upsaliensis
Patel N, Tahara SM, Malik P, Kalra VK (2011) Involvement of miR-30c and miR-301a in immediate induction of plasminogen activator inhibitor-1 by placental growth factor in human pulmonary endothelial cells. Biochem J 434:473–482
Hirahata M, Osaki M, Kanda Y, Sugimoto Y, Yoshioka Y, Kosaka N, Takeshita F, Fujiwara T, Kawai A, Ito H (2016) PAI-1, a target gene of miR-143, regulates invasion and metastasis by upregulating MMP-13 expression of human osteosarcoma. Cancer Med 5:892–902
Lui W (2016) Characterisation of miR-494 in coagulation. Dissertation, Murdoch University
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative CT method. Nat Protoc 3:1101–1108
Ramakers C, Ruijter JM, Deprez RHL, Moorman AF (2003) Assumption-free analysis of quantitative real-time polymerase chain reaction (PCR) data. Neurosci Lett 339:62–66
Zeng C, Waheed AA, Li T, Yu J, Zheng Y-M, Yount JS, Wen H, Freed EO, Liu S-L (2021) SERINC proteins potentiate antiviral type I IFN production and proinflammatory signaling pathways. Sci Signal 14:eabc7611
Rosa A, Ballarino M, Sorrentino A, Sthandier O, De Angelis F, Marchioni M, Masella B, Guarini A, Fatica A, Peschle C (2007) The interplay between the master transcription factor PU. 1 and miR-424 regulates human monocyte/macrophage differentiation. Proc Natl Acad Sci 104:19849–19854
Wu YZ, Chan KYY, Leung KT, Lam HS, Tam YH, Lee KH, Li K, Ng PC (2021) The miR-223/nuclear factor I-A axis regulates inflammation and cellular functions in intestinal tissues with necrotizing enterocolitis. FEBS Open Bio 11:1907–1920
Hu Y-W, Zhao J-Y, Li S-F, Huang J-L, Qiu Y-R, Ma X, Wu S-G, Chen Z-P, Hu Y-R, Yang J-Y (2015) RP5-833A20. 1/miR-382-5p/NFIA-dependent signal transduction pathway contributes to the regulation of cholesterol homeostasis and inflammatory reaction. Arterioscl Thrombosis Vasc Biol 35:87–101
Minamino T, Orimo M, Shimizu I, Kunieda T, Yokoyama M, Ito T, Nojima A, Nabetani A, Oike Y, Matsubara H (2009) A crucial role for adipose tissue p53 in the regulation of insulin resistance. Nat Med 15:1082–1087
Vilborg A, Glahder JA, Wilhelm MT, Bersani C, Corcoran M, Mahmoudi S, Rosenstierne M, Grandér D, Farnebo M, Norrild B (2009) The p53 target Wig-1 regulates p53 mRNA stability through an AU-rich element. Proc Natl Acad Sci 106:15756–15761
Spinelli R, Florese P, Parrillo L, Zatterale F, Longo M, D’Esposito V, Desiderio A, Nerstedt A, Gustafson B, Formisano P (2022) ZMAT3 hypomethylation contributes to early senescence of preadipocytes from healthy first-degree relatives of type 2 diabetics. Aging Cell 21:e13557
Camaioni C, Gustapane M, Cialdella P, Della Bona R, Biasucci LMJI, Medicine E (2013) Microparticles and microRNAs: new players in the complex field of coagulation. Intern Emergency Med 8:291–296
Salloum-Asfar S, Teruel-Montoya R, Arroyo AB, García-Barberá N, Chaudhry A, Schuetz E, Luengo-Gil G, Vicente V, González-Conejero R, Martínez CJPO (2014) Regulation of coagulation factor XI expression by microRNAs in the human liver. PLoS ONE 9:e111713
Jose RJ, Manuel A (2020) COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med 8:e46–e47
Milenkovic M, Hadzibegovic A, Kovac M, Jovanovic B, Stanisavljevic J, Djikic M, Sijan D, Ladjevic N, Palibrk I, Djukanovic M (2022) D-dimer, CRP, PCT, and IL-6 levels at admission to ICU can predict in-hospital mortality in patients with COVID-19 pneumonia. Oxidat Med Cell Long 2022:1
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, **ang J, Wang Y, Song B, XJTI Gu (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054–1062
Tang N, Li D, Wang X, Sun Z (2020) Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18:844–847
Fayyad-Kazan M, Makki R, Skafi N, El Homsi M, Hamade A, El Majzoub R, Hamade E, Fayyad-Kazan H, Badran B (2021) Circulating miRNAs: potential diagnostic role for coronavirus disease 2019 (COVID-19). Infect Genet Evol 94:105020
Oto J, Navarro S, Larsen AC, Solmoirago MJ, Plana E, Hervás D, Fernández-Pardo Á, España F, Kristensen SR, Thorlacius-Ussing O (2020) MicroRNAs and neutrophil activation markers predict venous thrombosis in pancreatic ductal adenocarcinoma and distal extrahepatic cholangiocarcinoma. Int J Mol Sci 21:840
Chen H, Li X, Liu S, Gu L, Zhou X (2017) MircroRNA-19a promotes vascular inflammation and foam cell formation by targeting HBP-1 in atherogenesis. Sci Rep 7:12089
Chow JT, Salmena L (2020) Prediction and analysis of SARS-CoV-2-Targeting MicroRNA in human lung epithelium. Genes (Basel) 2020:11
Arghiani N, Nissan T, Matin MMJB, Pharmacotherapy (2021) Role of microRNAs in COVID-19 with implications for therapeutics. Biomed Pharmacother 144:112247
Villadsen S, Bramsen J, Ostenfeld M, Wiklund E, Fristrup N, Gao S, Hansen T, Jensen T, Borre M, Ørntoft TJBjoc (2012) The miR-143/-145 cluster regulates plasminogen activator inhibitor-1 in bladder cancer. Br J Cancer 106:366–374
Tiedt S, Prestel M, Malik R, Schieferdecker N, Duering M, Kautzky V, Stoycheva I, Böck J, Northoff BH, Klein MJCR (2017) RNA-Seq identifies circulating miR-125a-5p, miR-125b-5p, and miR-143-3p as potential biomarkers for acute ischemic stroke. Circ Res 121:970–980
Zeng Z, **a L, Fan X, Ostriker AC, Yarovinsky T, Su M, Zhang Y, Peng X, **e Y, Pi LJTJ (2019) Platelet-derived miR-223 promotes a phenotypic switch in arterial injury repair. J Clin Invest 129:1372–1386
Alexandru N, Constantin A, Nemecz M, Comariţa IK, Vîlcu A, Procopciuc A, Tanko G, Georgescu AJFIM (2019) Hypertension associated with hyperlipidemia induced different microRNA expression profiles in plasma, platelets, and platelet-derived microvesicles; effects of endothelial progenitor cell therapy. Front Med 280:1
Morales L, Oliveros JC, Enjuanes L, Sola IJM (2022) Contribution of host miRNA-223-3p to SARS-CoV-induced lung inflammatory pathology. MBio 13:e03135-e3221
Rezk N, Elsayed Sileem A, Gad D, Khalil AOJZUMJ (2022) miRNA-223-3p, miRNA-2909 and cytokines expression in COVID-19 patients treated with ivermectin. Zagazig Univ Med J 28:573–582
Leierseder S, Petzold T, Zhang L, Loyer X, Massberg S, Engelhardt S (2013) MiR-223 is dispensable for platelet production and function in mice. Thromb Haemost 110:1207–1214
Nahand JS, Karimzadeh MR, Nezamnia M, Fatemipour M, Khatami A, Jamshidi S, Moghoofei M, Taghizadieh M, Hajighadimi S, Shafiee AJIL (2020) The role of miR-146a in viral infection. IUBMB Life 72:343–360
Letafati A, Najafi S, Mottahedi M, Karimzadeh M, Shahini A, Garousi S, Abbasi-Kolli M, Sadri Nahand J, Tamehri Zadeh SS, Hamblin MRJC, Letters MB (2022) MicroRNA let-7 and viral infections: focus on mechanisms of action. Cell Mol Biol Lett 27:1–47
Jafarzadeh A, Naseri A, Shojaie L, Nemati M, Jafarzadeh S, Baghi HB, Hamblin MR, Akhlagh SA, Mirzaei HJII (2021) MicroRNA-155 and antiviral immune responses. Int Immunopharmacol 101:108188
Nahand JS, Shojaie L, Akhlagh SA, Ebrahimi MS, Mirzaei HR, Baghi HB, Mahjoubin-Tehran M, Rezaei N, Hamblin MR, Tajiknia VJMT-NA (2021) Cell death pathways and viruses: role of microRNAs. Mol Therapy Nucl Acids 24:487–511
Hazra B, Kumawat KL, Basu A (2017) The host microRNA miR-301a blocks the IRF1-mediated neuronal innate immune response to Japanese encephalitis virus infection. Sci Signal 10:eaaf5185
Hazra B, Chakraborty S, Bhaskar M, Mukherjee S, Mahadevan A, Basu A (2019) miR-301a regulates inflammatory response to japanese encephalitis virus infection via suppression of NKRF activity. J Immunol (Baltimore, Md: 1950) 203:2222–2238
Jankowska KI, Sauna ZE, Atreya CD (2020) Role of microRNAs in hemophilia and thrombosis in humans. Int J Mol Sci 21:1
He C, Shi Y, Wu R, Sun M, Fang L, Wu W, Liu C, Tang M, Li Z, Wang PJG (2016) miR-301a promotes intestinal mucosal inflammation through induction of IL-17A and TNF-α in IBD. Gut 65:1938–1950
Parray A, Mir F, Doudin A, Iskandarani A, Danjuma IM, Kuni R, Abdelmajid A, Abdelhafez I, Arif R, Mulhim M (2021) Blood snoRNAs and miRNAs as predictors of COVID-19 Severity. Res Square 2021:1
Acknowledgements
Not applicable.
Funding
This project was supported by the Infectious and Tropical Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran (IR.TBZMED.REC.1401.276), and Iraqi Ministry of Higher Education and Scientific Research, Iraq.
Author information
Authors and Affiliations
Contributions
NF and HBB design the experiments and supervised the research. AKHAK, JSN, AS, HM, MM, carried out the experiment, analyzed data, wrote and revised the manuscript. AB, PSH and RR contributed to the data collection and drafting of the manuscript. Each scholar verified the resulting version to submit the paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to report.
Consent for Publication
Not applicable.
Ethics Approval and Consent to Participate
The research protocol was approved by the Medical Ethics Committee of Tabriz University of Medical Sciences, Iran (IR.TBZMED.REC.1401.276). All research units signed an informed written consent according to the declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kasho, A.K.A., Nahand, J.S., Salmaninejad, A. et al. PBMC MicroRNAs: Promising Biomarkers for the Differential Diagnosis of COVID-19 Patients with Abnormal Coagulation Indices. Curr Microbiol 80, 248 (2023). https://doi.org/10.1007/s00284-023-03365-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-023-03365-2