Abstract
Purpose
To investigate whether coadministration of vindesine is a risk factor for acute kidney injury caused by high-dose methotrexate in patients with hematologic malignancies and identify its mechanism.
Methods
A retrospective analysis was conducted on 211 cycles of HD-MTX therapy in 178 patients with hematological malignancies. Multivariate logistic regression analysis was performed to evaluate whether VDS coadministration was a risk factor for AKI and the inhibitory effect of VDS on MTX was studied in cell models in vitro.
Results
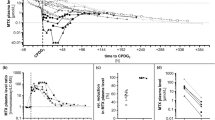
The occurrence of AKI was significantly higher in the MTX + VDS group than in the MTX group. Multivariate logistic regression analysis showed that VDS coadministration was an important risk factor for the occurrence of AKI [odds ratio (OR) = 2.62, 95% confidence interval (CI) 1.03–6.66]. After coadministration of VDS, serum MTX concentrations at 24 h, 48 h, and 72 h increased from 0.42 ± 0.46 μmol/L, 0.07 ± 0.01 μmol/L, and 0.03 ± 0.01 μmol/L to 0.98 ± 2.73 μmol/L, 0.18 ± 0.42 μmol/L, and 0.09 ± 0.21 μmol/L (p < 0.05, p < 0.01, and p < 0.01), respectively. Delayed elimination was closely related to AKI (p < 0.001). The transfected cell model results showed that VDS is an inhibitor of the transporters BCRP, MRP2, and OAT1/OAT3. VDS inhibited BCRP and MRP2-mediated transport of MTX with IC50 values of 17.91 µM and 34.73 µM, respectively.
Conclusions
Coadministration of VDS increases HD-MTX-induced AKI in patients with hematologic malignancies, which may be explained by the fact that VDS increases the exposure to and decreases the excretion of MTX by inhibiting OAT1/OAT3, BCRP, and MRP2.





Similar content being viewed by others
References
Howard SC, McCormick J, Pui CH, Buddington RK, Harvey RD (2016) Preventing and Managing Toxicities of High-Dose Methotrexate. Oncologist 21(12):1471–1482. https://doi.org/10.1634/theoncologist.2015-0164
Han X, Ji Y, Ouyang M, Zhu T, Zhou D (2017) Efficacy and safety of HD-MTX based systemic chemotherapy regimens: retrospective study of induction therapy for primary central nervous system lymphoma in Chinese. Sci Rep 7(1):17053. https://doi.org/10.1038/s41598-017-17359-1
Harrison DJ, Geller DS, Gill JD, Lewis VO, Gorlick R (2018) Current and future therapeutic approaches for osteosarcoma. Expert Rev Anticancer Ther 18(1):39–50. https://doi.org/10.1080/14737140.2018.1413939
Bath RK, Brar NK, Forouhar FA, Wu GY (2014) A review of methotrexate-associated hepatotoxicity. J Dig Dis 15(10):517–524. https://doi.org/10.1111/1751-2980.12184
May J, Carson KR, Butler S, Liu W, Bartlett NL, Wagner-Johnston ND (2014) High incidence of methotrexate associated renal toxicity in patients with lymphoma: a retrospective analysis. Leukemia Lymphoma 55(6):1345–1349. https://doi.org/10.3109/10428194.2013.840780
Widemann BC, Balis FM, Kempf-Bielack B, Bielack S, Pratt CB, Ferrari S, Bacci G, Craft AW, Adamson PC (2004) High-dose methotrexate-induced nephrotoxicity in patients with osteosarcoma. Cancer 100(10):2222–2232. https://doi.org/10.1002/cncr.20255
Tsurusawa M, Gosho M, Mori T, Mitsui T, Sunami S, Kobayashi R, Fukano R, Tanaka F, Fujita N, Inada H, Koh K, Takimoto T, Saito A, Fujimoto J, Nakazawa A, Horibe K, lymphoma committee of the Japanese Pediatric Leukemia/lymphoma Study G (2015) Statistical analysis of relation between plasma methotrexate concentration and toxicity in high-dose methotrexate therapy of childhood nonHodgkin lymphoma. Pediatr Blood Cancer 62(2):279–284. https://doi.org/10.1002/pbc.25305
Kawase A, Yamamoto T, Egashira S, Iwaki M (2016) Stereoselective inhibition of methotrexate excretion by glucuronides of nonsteroidal anti-inflammatory drugs via multidrug resistance proteins 2 and 4. J Pharmacol Exp Ther 356(2):366–374. https://doi.org/10.1124/jpet.115.229104
Santucci R, Leveque D, Lescoute A, Kemmel V, Herbrecht R (2010) Delayed elimination of methotrexate associated with co-administration of proton pump inhibitors. Anticancer Res 30(9):3807–3810
Jia Y, Liu Z, Wang C, Meng Q, Huo X, Liu Q, Sun H, Sun P, Yang X, Ma X, Liu K (2016) P-gp, MRP2 and OAT1/OAT3 mediate the drug–drug interaction between resveratrol and methotrexate. Toxicol Appl Pharmacol 306:27–35. https://doi.org/10.1016/j.taap.2016.06.030
Blum R, Seymour JF, Toner G (2002) Significant impairment of high-dose methotrexate clearance following vancomycin administration in the absence of overt renal impairment. Ann Oncol 13(2):327–330
Suzuki K, Doki K, Homma M, Tamaki H, Hori S, Ohtani H, Sawada Y, Kohda Y (2009) Co-administration of proton pump inhibitors delays elimination of plasma methotrexate in high-dose methotrexate therapy. Br J Clin Pharmacol 67(1):44–49. https://doi.org/10.1111/j.1365-2125.2008.03303.x
Jue Zhang YZ, Li **n, Bai Yan, Liu Yali, ** Runming (2016) Comparison of the efficacy, safety and economic cost of vindesine and vincristine fro newly diagnosed pediatric acute lymphoblastic leukemia: a retrospective analysis. J China Pediatric Blood Cancer 21(4):185–190
Chioukh R, Noel-Hudson MS, Ribes S, Fournier N, Becquemont L, Verstuyft C (2014) Proton pump inhibitors inhibit methotrexate transport by renal basolateral organic anion transporter hOAT3. Drug Metabol Disposition: Biological Fate Chem 42(12):2041–2048. https://doi.org/10.1124/dmd.114.058529
Narumi K, Sato Y, Kobayashi M, Furugen A, Kasashi K, Yamada T, Teshima T, Iseki K (2017) Effects of proton pump inhibitors and famotidine on elimination of plasma methotrexate: evaluation of drug–drug interactions mediated by organic anion transporter 3. Biopharm Drug Dispos 38(9):501–508. https://doi.org/10.1002/bdd.2091
Liu Q, Wang C, Meng Q, Huo X, Sun H, Peng J, Ma X, Sun P, Liu K (2014) MDR1 and OAT1/OAT3 mediate the drug–drug interaction between puerarin and methotrexate. Pharm Res 31(5):1120–1132. https://doi.org/10.1007/s11095-013-1235-9
Maeda A, Tsuruoka S, Ushijima K, Kanai Y, Endou H, Saito K, Miyamoto E, Fujimura A (2010) Drug interaction between celecoxib and methotrexate in organic anion transporter 3-transfected renal cells and in rats in vivo. Eur J Pharmacol 640(1–3):168–171. https://doi.org/10.1016/j.ejphar.2010.04.051
Shitara Y, Hirano M, Sato H, Sugiyama Y (2004) Gemfibrozil and its glucuronide inhibit the organic anion transporting polypeptide 2 (OATP2/OATP1B1:SLC21A6)-mediated hepatic uptake and CYP2C8-mediated metabolism of cerivastatin: analysis of the mechanism of the clinically relevant drug–drug interaction between cerivastatin and gemfibrozil. J Pharmacol Exp Ther 311(1):228–236. https://doi.org/10.1124/jpet.104.068536
Ivanyuk A, Livio F, Biollaz J, Buclin T (2017) Renal Drug Transporters and Drug Interactions. Clin Pharmacokinet 56(8):825–892. https://doi.org/10.1007/s40262-017-0506-8
Fyfe MJ, Goldman ID (1973) Characteristics of the vincristine-induced augmentation of methotrexate uptake in Ehrlich ascites tumor cells. J Biol Chem 248(14):5067–5073
Bender RA, Bleyer WA, Frisby SA, Oliverio VT (1975) Alteration of methotrexate uptake in human leukemia cells by other agents. Cancer Res 35(5):1305–1308
Warren RD, Nichols AP, Bender RA (1977) The effect of vincristine on methotrexate uptake and inhibition of DNA synthesis by human lymphoblastoid cells. Cancer Res 37(9):2993–2997
Tubiana N, Lena N, Barbet J, Imbert AM, Lejeune C, Maraninchi D, Sainty D, Sebahoun G, Gastaut JA, Cano JP et al (1985) Methotrexate-vindesine association in leukemia: pharmacokinetic study. Med Oncol Tumor Pharmacother 2(2):99–102
Smeland E, Bremnes RM, Bessesen A, Jaeger R, Aarbakke J (1993) Interactions of vinblastine and vincristine with methotrexate transport in isolated rat hepatocytes. Cancer Chemother Pharmacol 32(3):209–214. https://doi.org/10.1007/bf00685837
Bremnes RM, Smeland E, Slordal L, Wist E, Aarbakke J (1991) The effect of vindesine on methotrexate hydroxylation in the rat. Biochem Pharmacol 42(8):1561–1568. https://doi.org/10.1016/0006-2952(91)90425-5
El-Sheikh AA, Greupink R, Wortelboer HM, van den Heuvel JJ, Schreurs M, Koenderink JB, Masereeuw R, Russel FG (2013) Interaction of immunosuppressive drugs with human organic anion transporter (OAT) 1 and OAT3, and multidrug resistance-associated protein (MRP) 2 and MRP4. Translational research: the journal of laboratory and clinical medicine 162(6):398–409. https://doi.org/10.1016/j.trsl.2013.08.003
Hou Z, Matherly LH (2014) Biology of the major facilitative folate transporters SLC19A1 and SLC46A1. Curr Top Membr 73:175–204. https://doi.org/10.1016/B978-0-12-800223-0.00004-9
Acknowledgements
This study was supported by the National Natural Science Foundation of China (grant number: 81773820), the National Key New Drug Creation Special Programs (2017ZX09304-021), the Jiangsu Provincial Medical Talent (ZDRCA2016048), and the Suzhou Key Laboratory of Drug Clinical Research and Personalized Medicine (SZS201719).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, C., **a, F., Xue, L. et al. Coadministration of vindesine with high-dose methotrexate therapy increases acute kidney injury via BCRP, MRP2, and OAT1/OAT3. Cancer Chemother Pharmacol 85, 433–441 (2020). https://doi.org/10.1007/s00280-019-03972-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-019-03972-6