Abstract
Introduction
The circumflex scapular artery (CSA) has been described in detail in the literature, but the groove, i.e., the circumflex sulcus (CFS), formed by the artery on the lateral pillar of the scapula has been completely neglected. The aim of the present study was to describe the variability and anatomy of the CFS.
Materials and methods
The study was based on the examination of 103 pairs of dry bone specimens of adult scapulae, i.e., 206 specimens, including 92 (46 pairs) male and 114 (57 pairs) female specimens. In the first step, quantitative criteria were defined for assessment of the CFS presence and type. Subsequently, statistical analysis of the obtained data was performed.
Results
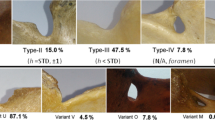
The study revealed considerable variability of the arterial groove, which was well developed in 33% (type A), shallow in 40% (type B), and absent in 27% (type C) of cases. The mean distance between CFS and the infraglenoid tubercle was 3.3 cm CI0.95 (3.1–3.3), which corresponds to the proximal third of the lateral border of the scapula.
Conclusion
The study has confirmed variability of the arterial groove (CFS) and its localization in relation to the inferior glenoid rim. The findings are clinically important, particularly in relation to the Judet approach to scapular fractures (localization of the CSA course).







Similar content being viewed by others
Availability of data and materials
Data are obtained from institutional collections—Pachner’s collection of the Institute of Anatomy of First Faculty of Medicine of Charles University and Department of Anthropology and Human Genetics of the Faculty of Science of Charles University, Prague.
References
Alfaro-Gomez U, Fuentes-Ramirez LD, Chavez-Blanco KI et al (2020) Anatomical variations of the acromial and coracoid process: clinical relevance. Surg Radiol Anat 42:877–885. https://doi.org/10.1007/s00276-020-02497-5
Al-Redouan A, Kachlik D (2022) Scapula revisited: new features identified and denoted by terms using consensus method of Delphi and taxonomy panel to be implemented in radiologic and surgical practice. J Shoulder Elbow Surg 31:e68–e81. https://doi.org/10.1016/j.jse.2021.07.020
Armitage BM, Wijdicks CA, Tarkin IS et al (2009) Map** of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am 91:2222–2228. https://doi.org/10.2106/JBJS.H.00881
Bartoníček J (2015) Scapular fractures. In: Courtbrown CH, Heckman AD, Mcmqqueen MM, Ricci WM, Tornetta P (eds) Rockwood and Green’s fractures in adults, 8th edn. Wolters Kluwer, Philadelphia, pp 1475–1501
Bartoníček J, Frič V (2011) Scapular body fractures: results of the operative treatment. Int Orthop 35:747–753. https://doi.org/10.1007/s00264-010-1072-y
Bartoníček J, Klika D, Tuček M (2018) Classification of scapular body fractures. Rozhl Chir 97:67–76
Bartoníček J, Tuček M, Luňáček L (2008) Judet posterior approach to scapula. Acta Chir Orthop Traumatol Cech 75:429–435
Burke CS, Roberts CS, Nyland JA, Radmacher PG, Acland RD, Voor MJ (2006) Scapular thickness—implications for fracture fixation. J Shoulder Elbow Surg 15:645–648. https://doi.org/10.1016/j.jse.2005.10.005
Casier SJ, Van den Broecke R, Van Houcke J, Audenaert E, De Wilde LF, Van Tongel A (2018) Morphologic variations of the scapula in 3-dimensions: a statistical shape model approach. J Shoulder Elbow Surg 27:2224–2231. https://doi.org/10.1016/j.jse.2018.06.001
Donders JCE, Prins J, Kloen P, at al, (2020) Three-dimensional topography of scapular nutrient foramina. Surg Radiol Anat 42:887–892. https://doi.org/10.1007/s00276-020-02441-7
Dupont R, Evrard H (1932) Sur une voie d’accès postérieure de l’omoplate. J Chir 39:528–534
Ebraheim NA, Xu R, Haman SP, Mielder JD, Yeasting RA (2000) Quantitative anatomy of the scapula. Am J Orthop 29:287–292
Ebraheim NA, Ramineni SK, Alla SR, Biyani S, Yeasting RA (2010) Anatomical basis of the vascular risk related to the circumflex scapular artery during posterior approach to the scapula. Surg Radiol Anat 32:51–54. https://doi.org/10.1007/s00276-009-0544-5
Edelson JG (1996) Variations in the anatomy of the scapula with reference to the snap** scapula. Clin Orthop Relat Res 322:111–115
Frazer JES (1946) The anatomy of the human skeleton. Churchill, London
Galino M, Santamaria E, Doro T (1998) Anthropometry of the scapula: clinical and surgical consideration. J Shoulder Elbow Surg 7:284–291. https://doi.org/10.1016/s1058-2746(98)90057-x
Gumina S, Postachini F, Orsina L, Cinotti G (1999) The morphometry of coracoid process—its aetiologic role in subcoracoid im**ement syndrome. Int Orthop 23:198–201. https://doi.org/10.1007/s002640050349
Hovelacque A (1933) Ostéologie. Fascicule 1. Paris, Doin & Cie.
Idrac M (1935) Fracture du col chirurgical de l´omoplate. Bull Soc Med Mil Fr 29:205–208
Johnston TB, Davies DV, Davies F (eds) (1958) Gray´s anatomy, 32nd edn. Longmans, Green and Co., London
Kalný J (1962) Foramina nutricia a canales nutricii na lopatce a na pánevní kosti. [Foramina nutricia and canales nutricii on the scapula and pelvic bone]. Plz Lék Sbor 25–34
Karelse A, Kegels L, de Wilde L (2005) The pillars of the scapula. Clin Anat 20:392–399. https://doi.org/10.1002/ca.20420
Li MM, Goetti P, Sandman E, Rouleau DM (2020) Influence of coracoid anatomy on the location of glenoid rim defects in anterior shoulder instability: 3D CT-scan evaluation of 51 patients. Surg Radiol Anat 42:895–901. https://doi.org/10.1007/s00276-020-02492-w
Mallon WJ, Brown HR, Vogler JB, Martinez S (1982) Radiographic and geometric anatomy of the scapula. Clin Orthop Rel Res 277:142–154
Ogden JA, Phillips SB (1983) Radiology of postnatal skeletal development. VII. The scapula. Skeletal Radiol 9:157–169. https://doi.org/10.1007/BF00352547
Pachner P (1937) Pohlavní rozdíly na lidské pánvi [Sex differences in the human pelvis]. In Czech. Česká akademie věd a umění, Praha
Rauber-Kopsch (1952) Lehrbuch und Atlas der Anatomie des Menschen, Band 1. 18. Auflage. Leipzig, Thieme
Shin KJ, Kim JN, Lee SH et al (2016) Arterial supply and anastomotic pattern of the infraspinous fossa focusing on the surgical significance. J Plast Reconstr Aesthet Surg 69:512–518. https://doi.org/10.1016/j.bjps.2015.12.013
Singh N, Chauhan P, Loh HK, Kohli M, Suri RK (2018) Enigma of scapular foramen and tunnels: an untold story. Surg Radiol Anat 40:327–332. https://doi.org/10.1007/s00276-017-1931-y
Strnad T, Bartoníček J, Naňka O, Tuček M (2021) The coracoglenoid notch: anatomy and clinical significance. Surg Radiol Anat 43:11–17. https://doi.org/10.1007/s00276-020-02527-2
Testut L (1904) Traité d´anatomie humaine. Doin, Paris, pp 262–267
Totlis T, Konstantidinis GA, Karanassos MT et al (2014) Bony structures related to snap** scapula: correlation to gender, side and age. Surg Radiol Anat 36:3–9. https://doi.org/10.1007/s00276-013-1130-4
Tuček M, Bartoníček J, Frič V (2011) Kostní anatomie lopatky: Její význam pro klasifikaci zlomenin těla lopatky [Osseous anatomy of scapula: Its importance for classification of scapular body]. Ortopedie 5:104–109
Tuček M, Naňka O, Malík J, Bartoníček J (2014) Scapular glenopolar angle: Standard values and side differences. Skeletal Radiol 43:1583–1587. https://doi.org/10.1007/s00256-014-1977-4
Vavken P, Heinrich KM, Koppelhuber C, Rois S, Dorotka R (2009) The use of confidence intervals in reporting orthopaedic research findings. Clin Orthop Relat Res 467:3334–3339. https://doi.org/10.1007/s11999-009-0817-7
von Schroeder HP, Kuiper SD, Botte MJ (2001) Osseous anatomy of the scapula. Clin Orthop Relat Res 383:131–139. https://doi.org/10.1097/00003086-200102000-00015
White DT, Black TM, Folkens AP (2012) Human osteology, 3rd edn. Elsevier, Amsterdam
Zhang L, Guo X, Liu Y et al (2019) Classification of the superior angle of the scapula and its correlation with the suprascapular notch: a study on 303 scapulae. Surg Radiol Anat 41:377–383. https://doi.org/10.1007/s00276-018-2156-4
Acknowledgements
The authors wish to thank Prof. Chris Colton MB BS FRCS and Ludmila Bébarová, PhD for their assistance with the editing of the manuscript, and Jan Cvrček, MA, PhD from the Department of Anthropology (National Museum, Prague, Czech Republic) for providing access to the osteological material. “The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind's overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.”
Funding
This study was supported by internal grant of The Ministry of Defense of the Czech Republic DZRVO MO1012.
Author information
Authors and Affiliations
Contributions
TS: data collection and analysis, manuscript writing JB: project development, manuscript editing MT: data analysis ON: data analysis, statistical analysis, manuscript editing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclaimer
None.
Ethics approval and consent to participate
This article does not contain any studies with human participants, or animals, performed by any of the authors.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Strnad, T., Bartoníček, J., Tuček, M. et al. Circumflex arterial sulcus of the scapula (sulcus arteriae circumflexae scapulae): its anatomy and clinical relevance. Surg Radiol Anat 44, 1111–1119 (2022). https://doi.org/10.1007/s00276-022-02993-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-022-02993-w