Abstract
Purpose
Distal humeral fractures are rare, but severe injuries, the treatment of which is often accompanied by serious complications and its outcome strongly depends on the quality of surgical therapy. Non-union is a common entity, compromising clinical results and requiring revision surgery. Osteonecrosis is an underestimated etiologic factor in the development of non-union. The present study aims to display the distribution patterns of the arterial vessels at the distal humerus, to correlate the displayed vessels with local nutrient foramina and to disclose an endangerment of these structures by common osteosynthetic implants.
Methods
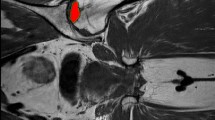
Eight plastinated fresh frozen upper extremities were digitally analyzed regarding the vascular density of the cancellous bone, by calculating the ratio of area comprised by arterial vessels and the area comprised by cancellous bone on sagittal cuts of the distal humerus. Possible differences in the vascular density of the medial epicondylar region, the lateral epicondylar region and a watershed area between the epicondyles and distal to the supracondylar region were investigated. On the basis of 200 macerated humeri, the distribution pattern of cortical nutrient foramina and their anatomic relation to properly applied common distal humerus plates were documented.
Results
The data show a significantly higher density of vessels per cancellous bone in the epicondylar regions than in the watershed region (p < 0.000, median 0.148 vs. 0.103). The analysis of the nutrient foramina showed distinct distribution patterns with a single foramen over the medial epicondyle (55 specimens, 27.5 %) and an area of several foramina at the posterior part of the lateral epicondyle (200 of the specimens, 100 %). In almost every specimen, the application of the osteosynthetic implants led to an overlay over the investigated nutrient foramina.
Discussion
Osteonecrosis and non-union are severe complications in the surgical treatment of distal humeral fractures. The biology of the bone, especially the blood supply, has to be respected as much as possible during open procedures, to optimize bony healing. This has to be considered when performing periosteal strip** or applying osteosynthetic plates over the postero-lateral and medial epicondyle. The watershed area of the distal humerus has to be considered as being prone to minor arterial blood supply and thereby non-union is possible, if the arterial vessels coming from the epicondyles are destroyed.








Similar content being viewed by others
References
Arnander MW, Reeves A, MacLeod IA, Pinto TM, Khaleel A (2008) A biomechanical comparison of plate configuration in distal humerus fractures. J Orthop Trauma 22(5):332–336
Carroll SE (1963) A study of the nutrient foramina of the humeral diaphysis. J Bone Joint Surg Br 45:176–181
Crock HV (ed) (1996) An atlas of vascular anatomy of the skeleton and spinal cord. Taylor and Francis Ltd, London
Haraldsson S (1957) The intra-osseous vasculature of the distal end of the humerus with special reference to capitulum; preliminary communication. Acta Orthop Scand 27(2):81–93
Joshi H, Doshi B, Malukar O (2011) A study of the nutrient foramina of the humeral diaphysis. Nat J Integrat Res Med 2(2):14–17
Kimball JP, Glowczewskie F, Wright TW (2007) Intraosseous blood supply to the distal humerus. J Hand Surg Am 32(5):642–646
Kizilkanat E, Boyan N, Ozsahin ET, Soames R, Oguz O (2007) Location, number and clinical significance of nutrient foramina in human long bones. Ann Anat 189(1):87–95
Korner J, Diederichs G, Arzdorf M, Lill H, Josten C, Schneider E et al (2004) A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma 18(5):286–293
Korner J, Lill H, Muller LP, Hessmann M, Kopf K, Goldhahn J et al (2005) Distal humerus fractures in elderly patients: results after open reduction and internal fixation. Osteoporos Int 16(Suppl 2):S73–S79
Kundel K, Braun W, Wieberneit J, Ruter A (1996) Intraarticular distal humerus fractures. Factors affecting functional outcome. Clin Orthop Relat Res 332:200–208
Laing PG (1956) The arterial supply of the adult humerus. J Bone Joint Surg Am 38(5):1105–1116
Lob G, Burri C, Feil J (1984) Operative treatment of distal intra-articular humerus fractures; results of 412 follow-up cases (AO-collected statistics). Langenbecks Arch Chir 364:359–361
Murlimanju BV, Prashanth KU, Prabhu LV, Saralaya VV, Pai MM, Rai R (2011) Morphological and topographical anatomy of nutrient foramina in human upper limb long bones and their surgical importance. Rom J Morphol Embryol 52(3):859–862
O’Driscoll SW (2005) Optimizing stability in distal humeral fracture fixation. J Shoulder Elbow Surg 14((1 Suppl S)):S186–S194
O’Driscoll SW (2009) Parallel plate fixation of bicolumn distal humeral fractures. Instr Course Lect 58:521–528
Rath B, Notermans HP, Franzen J, Knifka J, Walpert J, Frank D et al (2009) The microvascular anatomy of the metatarsal bones: a plastination study. Surg Radiol Anat 31(4):271–277
Rubberdt A, Surke C, Fuchs T, Frerichmann U, Matuszewski L, Vieth V et al (2008) Preformed plate-fixation system for type AO 13C3 distal humerus fractures: clinical experiences and treatment results taking access into account. Unfallchirurg 111(5):308–322
Sodergard J, Sandelin J, Bostman O (1992) Mechanical failures of internal fixation in T and Y fractures of the distal humerus. J Trauma 33(5):687–690
Stoffel K, Cunneen S, Morgan R, Nicholls R, Stachowiak G (2008) Comparative stability of perpendicular versus parallel double-locking plating systems in osteoporotic comminuted distal humerus fractures. J Orthop Res 26(6):778–784
Tien YC, Chen JC, Fu YC, Chih TT, Huang PJ, Wang GJ (2006) Supracondylar dome osteotomy for cubitus valgus deformity associated with a lateral condylar nonunion in children. Surgical technique. J Bone Joint Surg Am 88(Suppl 1 Pt 2):191–201
Wiggers JK, Ring D (2011) Osteonecrosis after open reduction and internal fixation of a bicolumnar fracture of the distal humerus: a report of four cases. J Hand Surg Am 36(1):89–93
Yamaguchi K, Sweet FA, Bindra R, Morrey BF, Gelberman RH (1997) The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am 79(11):1653–1662
Zalavras CG, Vercillo MT, Jun BJ, Otarodifard K, Itamura JM, Lee TQ (2011) Biomechanical evaluation of parallel versus orthogonal plate fixation of intra-articular distal humerus fractures. J Shoulder Elbow Surg 20(1):12–20
Conflict of interest
The biomechanical laboratory of the Department of Trauma Surgery is supported by a yearly grant by the “Medartis” Company, but not specifically for this study. K.J.B. and L.P.M. did not and will not receive any financial benefit in any form. No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Prof Koebke tragically deceased in February 2012.
Rights and permissions
About this article
Cite this article
Wegmann, K., Burkhart, K.J., Koslowsky, T. . et al. Arterial supply of the distal humerus. Surg Radiol Anat 36, 705–711 (2014). https://doi.org/10.1007/s00276-013-1240-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-013-1240-z