Abstract
Background
Single-stage mastopexy augmentation is a much-debated intervention due to its complexity and the associated relatively high complication rates. This study aimed to reevaluate the risk factors for these complications using a novel approach based on artificial intelligence and to demonstrate its possible limitations.
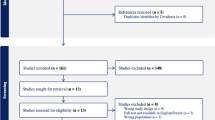
Patients and Methods
Complete datasets of patients who underwent single-staged augmentation mastopexy during 2014–2023 at one institution by a single surgeon were collected retrospectively. These were subsequently processed and analyzed by CART, RF and XGBoost algorithms.
Results
A total of 342 patients were included in the study, of which 43 (12.57%) reported surgery-associated complications, whereby capsular contracture (n = 19) was the most common. BMI represented the most important variable for the development of complications (FIS = 0.44 in CART). 2.9% of the patients expressed the desire for implant change in the course, with absence of any complications. A statistically significant correlation between smoking and the desire for implant change (p < 0.001) was revealed.
Conclusion
The importance of implementing artificial intelligence into clinical research could be underpinned by this study, as risk variables can be reclassified based on factors previously considered less or even irrelevant. Thereby we encountered limitations using ML approaches. Further studies will be needed to investigate the association between smoking, BMI and the current implant size with the desire for implant change without any complications. Moreover, we could show that the procedure can be performed safely without high risk of develo** major complications.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266






Similar content being viewed by others
References
Gonzalez-Ulloa M (1960) Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg Transplant Bull 25:15–26
Regnault P (1966) The hypoplastic and ptotic breast: a combined operation with prosthetic augmentation. Plast Reconstr Surg 37(1):31–37
Swanson E (2016) All seasons vertical augmentation mastopexy: a simple algorithm, clinical experience, and patient-reported outcomes. Plast Reconstr Surg Glob Open 4(12):e1170
Spear S (2003) Augmentation/mastopexy: “surgeon, beware.” Plast Reconstr Surg 112(3):905–906
Swanson E (2013) Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammaplasty, performed individually and in combination. Plast Reconstr Surg 132(1):30e–45e
Xue AS, Dayan E, Rohrich RJ (2020) Achieving predictability in augmentation mastopexy: an update. Plast Reconstr Surg Glob Open 8(9):e2784
Artz JD, Tessler O, Clark S, Patel S, Torabi R, Moses M (2019) Can it be safe and aesthetic? An eight-year retrospective review of mastopexy with concurrent breast augmentation. Plast Reconstr Surg Glob Open 7(6):e2272
Ali B, Choi EE, Barlas V et al (2021) Perioperative safety of combined augmentation-mastopexy: An evaluation of national database. Ann Plast Surg 87(5):493–500
Stevens WG, Macias LH, Spring M, Stoker DA, Chacón CO, Eberlin SA (2014) One-stage augmentation mastopexy: a review of 1192 simultaneous breast augmentation and mastopexy procedures in 615 consecutive patients. Aesthet Surg J 34(5):723–732
Lee MR, Unger JG, Adams WP Jr (2014) The tissue-based triad: a process approach to augmentation mastopexy. Plast Reconstr Surg 134(2):215–225
Hashimoto DA, Rosman G, Rus D, Meireles OR (2018) Artificial intelligence in surgery: promises and perils. Ann Surg 268(1):70–76
Hedén P, Jernbeck J, Hober M (2001) Breast augmentation with anatomical cohesive gel implants: the world’s largest current experience. Clin Plast Surg 28(3):531–552
Hedén P (2009) Mastopexy augmentation with form stable breast implants. Clin Plast Surg 36(1):91–104
Montemurro P, Cheema M, Hedén P, Behr B, Wallner C (2019) Benchmarking the outcomes of single-stage augmentation mastopexy against primary breast augmentation: a single surgeon’s experience of 905 consecutive cases. Plast Reconstr Surg 144(2):326–334
Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W (2003) Classification and regression tree analysis in public health: methodological review and comparison with logistic regression. Ann Behav Med 26(3):172–181
Efron B, Tibshirani R (1997) Improvements on cross-validation: the .632+ bootstrap method. J Am Stat Assoc 92(438):548–560
Breiman L (2001) Random forests. Mach Learn 45(1):5–32
Ho TK (1998) The random subspace method for constructing decision forests. IEEE Trans Pattern Anal Mach Intell 20:832–844
Chen T, Guestrin C (2016) XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining, pp 785–794
Garoosi K, Mundra L, Jabbari K et al (2023) Comorbid conditions and complications in body contouring surgery: a retrospective review. Aesthet Surg J Open Forum 5:ojad080
Messa CA, Messa CA (2019) One-stage augmentation mastopexy: a retrospective ten-year review of 2183 consecutive procedures. Aesthet Surg J 39(12):1352–1367
Luan F, Gao X, Zhao S, Cai X (2022) The roles of plastic surgeons in advancing artificial intelligence in plastic surgery. Aesthetic Plast Surg 46(Suppl 1):184–185
Wallner C, Alam M, Drysch M et al (2021) A highly reliable convolutional neural network based soft tissue sarcoma metastasis detection from chest X-ray images: a retrospective cohort study. Cancers (Basel) 13(19):4961
Schmidt SV, Drysch M, Reinkemeier F et al (2023) Improvement of predictive scores in burn medicine through different machine learning approaches. Healthcare (Basel) 11(17):2317
Montemurro P, Lehnhardt M, Behr B, Wallner C (2022) A Machine learning approach to identify previously unconsidered causes for complications in aesthetic breast augmentation. Aesthetic Plast Surg 46(6):2669–2676
Meyer A, Cypko MA, Eickhoff C, Falk V, Emmert MY (2019) Artificial intelligence-assisted care in medicine: a revolution or yet another blunt weapon?: Potentials, challenges, and the future of implementing artificial intelligence (AI) for clinical care. Eur Heart J 40(40):3286–3289
Daye D, Wiggins WF, Lungren MP et al (2022) Implementation of clinical artificial intelligence in radiology: Who decides and how? Radiology 305(3):555–563
Istasy P, Lee WS, Iansavichene A et al (2022) The impact of artificial intelligence on health equity in oncology: sco** review. J Med Internet Res 24(11):e39748
Kanevsky J, Corban J, Gaster R, Kanevsky A, Lin S, Gilardino M (2016) Big data and machine learning in plastic surgery: a new frontier in surgical innovation. Plast Reconstr Surg 137(5):890e–897e
Wallner C, Huyghebaert T, Drysch M et al (2023) Digital media play a key role in influencing female breast perception. Cyberpsychol Behav Soc Netw 26(1):11–21
Wallner C, Kruber S, Adebayo SO et al (2022) Interethnic influencing factors regarding buttocks body image in women from Nigeria, Germany, USA and Japan. Int J Environ Res Public Health 19(20):13212
Stevens WG, Freeman ME, Stoker DA, Quardt SM, Cohen R, Hirsch EM (2007) One-stage mastopexy with breast augmentation: a review of 321 patients. Plast Reconstr Surg 120(6):1674–1679
Beale EW, Ramanadham S, Harrison B, Rasko Y, Armijo B, Rohrich RJ (2014) Achieving predictability in augmentation mastopexy. Plast Reconstr Surg 133(3):284e–292e
Hubaide M, Ono MT, Karner BM, Martins LV, Pires JA (2024) Safe augmentation mastopexy: review of 500 consecutive cases using a vertical approach and muscular sling. Plast Reconstr Surg Glob Open 12(1):e5504
Zucal I, Tremp M, Duscher D et al (2023) Augmentation-mastopexy: analysis of 95 consecutive patients and critical appraisal of the procedure. J Clin Med 12(9):3213
Ganon S, Morinet S, Serror K, Mimoun M, Chaouat M, Boccara D (2021) Epidemiology and prevention of breast prosthesis capsular contracture recurrence. Aesthetic Plast Surg 45(1):15–23
Calobrace MB, Stevens WG, Capizzi PJ, Cohen R, Godinez T, Beckstrand M (2018) Risk factor analysis for capsular contracture: a 10-year sientra study using round, smooth, and textured implants for breast augmentation. Plast Reconstr Surg 141(4S):20s–28s
Qiu B, Shen Z, Yang D, Wang Q (2023) Applying machine learning techniques to predict the risk of lung metastases from rectal cancer: a real-world retrospective study. Front Oncol 13:1183072
Hong W, Zhou X, ** S et al (2022) A Comparison of XGBoost, random forest, and nomograph for the prediction of disease severity in patients with COVID-19 pneumonia: implications of cytokine and immune cell profile. Front Cell Infect Microbiol 12:819267
Wang R, Zhang J, Shan B, He M, Xu J (2022) XGBoost machine learning algorithm for prediction of outcome in aneurysmal subarachnoid hemorrhage. Neuropsychiatr Dis Treat 18:659–667
Bai BL, Wu ZY, Weng SJ, Yang Q (2023) Application of interpretable machine learning algorithms to predict distant metastasis in osteosarcoma. Cancer Med 12(4):5025–5034
Nishi H, Oishi N, Ishii A et al (2019) Predicting clinical outcomes of large vessel occlusion before mechanical thrombectomy using machine learning. Stroke 50(9):2379–2388
Shi HY, Lee KT, Chiu CC, Wang JJ, Sun DP, Lee HH (2022) 5-year recurrence prediction after hepatocellular carcinoma resection: deep learning vs. Cox regression models. Am J Cancer Res 12(6):2876–2890
Lundberg SM, Nair B, Vavilala MS et al (2018) Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat Biomed Eng 2(10):749–760
Wijnberge M, Geerts BF, Hol L et al (2020) Effect of a machine learning-derived early warning system for intraoperative hypotension vs standard care on depth and duration of intraoperative hypotension during elective noncardiac surgery: The HYPE randomized clinical trial. JAMA 323(11):1052–1060
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Patients provided written consent before their inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huyghebaert, T.A., Wallner, C. & Montemurro, P. Implementation of a Machine Learning Approach Evaluating Risk Factors for Complications after Single-Stage Augmentation Mastopexy. Aesth Plast Surg (2024). https://doi.org/10.1007/s00266-024-04142-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00266-024-04142-7