Abstract
Background
Traditional spine magnetic resonance imaging (MRI) protocols require sedation in young children and uncooperative patients. There is an increased interest in non-sedated pediatric MRI protocols to reduce risks associated with anesthetic agents and improve MRI access.
Objective
To evaluate the image quality of pediatric non-sedated fast spine MRI.
Materials and methods
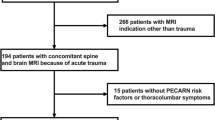
We retrospectively reviewed 69 pediatric non-sedated fast spine MRI exams performed in 57 patients. Two blinded readers provided image quality ratings for the evaluation of bones, cranio-cervical junction, cerebrospinal fluid (CSF) spaces, spinal cord, soft tissues, ligaments, and overall diagnostic quality on a 1–5 scale, and determined whether there was evidence of syringomyelia, abnormal conus medullaris position, or filum terminale abnormality.
Results
Mean patient age was 7.2 years (age range ≤ 1–17). Indications included syringomyelia (n=25), spinal dysraphism (n=4), combination of both syringomyelia and spinal dysraphism (n=8), and other miscellaneous indications (n=32). The inter-observer agreement ranged between moderate and very good for each variable (Cohen’s weighted kappa] range=0.45–0.69). The highest image quality ratings were given to CSF spaces (mean image quality=3.5/5 ± 0.8) and cranio-cervical junction evaluations (3.5/5 ± 0.9). Overall diagnostic quality was worst in the <5 years group (P=0.006). Readers independently identified a cervical spinal cord syrinx in 6 cases, and 1 mm spinal cord central canal dilation in one case. Readers agreed on the position of the conus medullaris in 92% of cases (23/25 cases).
Conclusion
Non-sedated pediatric spine MRI can be an effective diagnostic test to evaluate for spine pathology, especially syringomyelia, Chiari malformation, and conus medullaris anatomy.
Graphical abstract





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Tompane T, Bush R, Dansky T, Huang JS (2013) Diagnostic imaging studies performed in children over a nine-year period. Pediatrics 131:e45–e52
Uffman JC, Tumin D, Raman V et al (2017) MRI utilization and the associated use of sedation and anesthesia in a pediatric ACO. J Am Coll Radiol 14:924-930
Iskandar BJ, Sansone JM, Medow J, Rowley HA (2004) The use of quick-brain magnetic resonance imaging in the evaluation of shunt-treated hydrocephalus. J Neurosurg 101:147–151
Patel DM, Tubbs RS, Pate G et al (2014) Fast-sequence MRI studies for surveillance imaging in pediatric hydrocephalus. J Neurosurg Pediatr 13:440-447
Ashley WW Jr, McKinstry RC, Leonard JR et al (2005) Use of rapid-sequence magnetic resonance imaging for evaluation of hydrocephalus in children. J Neurosurg 103:124-130
Koral K, Blackburn T, Bailey AA, Koral KM, Anderson J (2012) Strengthening the argument for rapid brain MR imaging: estimation of reduction in lifetime attributable risk of develo** fatal cancer in children with shunted hydrocephalus by instituting a rapid brain MR imaging protocol in lieu of Head CT. AJNR Am J Neuroradiol 33:1851–1854
Lindberg DM, Stence NV, Grubenhoff JA, Lewis T, Mirsky DM, Miller AL, O’Neill BR, Grice K, Mourani PM, Runyan DK (2019) Feasibility and accuracy of fast MRI versus CT for traumatic brain injury in young children. Pediatrics 144(4). e20190419. https://doi.org/10.1542/peds.2019-0419
Kabakus IM, Spampinato MV, Knipfing M et al (2021) Fast brain magnetic resonance imaging with half-Fourier acquisition with single-shot turbo spin echo sequence in detection of intracranial hemorrhage and skull fracture in general pediatric patients: preliminary results. Pediatr Emerg Care 37:e1168-e1172
Shope C, Alshareef M, Larrew T et al (2021) Utility of a pediatric fast magnetic resonance imaging protocol as surveillance scanning for traumatic brain injury. J Neurosurg Pediatr 27:475-481
Kessler BA, Goh JL, Pajer HB, Asher AM, Northam WT, Hung SC, Selden NR, Quinsey CS (2021) Rapid-sequence MRI for evaluation of pediatric traumatic brain injury: a systematic review. J Neurosurg Pediatr 28(3):278–286. https://doi.org/10.3171/2021.2.PEDS20852
Malviya S, Voepel-Lewis T, Eldevik OP et al (2000) Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth 84:743-748
Wang X, Xu Z, Miao CH (2014) Current clinical evidence on the effect of general anesthesia on neurodevelopment in children: an updated systematic review with meta-regression. PLoS ONE 9:e85760
Chang YM, Ebrahimzadeh SA, Griffin H, Bhadelia RA (2022) Shortened total spine MRI protocol in the detection of spinal cord compression and pathology for emergent settings: a noninferiority study. Emerg Radiol 29:329–337
Robertson WD, Jarvik JG, Tsuruda JS et al (1996) The comparison of a rapid screening MR protocol with a conventional MR protocol for lumbar spondylosis. AJR Am J Roentgenol 166:909-916
Gewirtz JI, Skidmore A, Smyth MD et al (2020) Use of fast-sequence spine MRI in pediatric patients. J Neurosurg Pediatr 26:676-681
Ryan ME, Jaju A, Rychlik K et al (2022) Feasibility of rapid spine magnetic resonance evaluation for spinal cord syrinx in the pediatric population. Neuroradiology 64:1879-1885
Khalatbari H, Perez FA, Lee A, Shaw DWW (2020) Rapid magnetic resonance imaging of the spine in neonates with spinal dysraphism. World Neurosurg 144:e648–e659
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Patel MR, Klufas RA, Alberico RA, Edelman RR (1997) Half-fourier acquisition single-shot turbo spin-echo (HASTE) MR: comparison with fast spin-echo MR in diseases of the brain. AJNR Am J Neuroradiol 18:1635–1640
O’Neill BR, Pruthi S, Bains H et al (2013) Rapid sequence magnetic resonance imaging in the assessment of children with hydrocephalus. World Neurosurg 80:e307-312
Tekes A, Senglaub SS, Ahn ES, Huisman T, Jackson EM (2018) Ultrafast brain MRI can be used for indications beyond shunted hydrocephalus in pediatric patients. AJNR Am J Neuroradiol 39:1515–1518
Yamashita Y, Namimoto T, Abe Y et al (1997) MR imaging of the fetus by a HASTE sequence. AJR Am J Roentgenol 168:513-519
Glenn OA (2010) MR imaging of the fetal brain. Pediatr Radiol 40:68–81
Del Grande F, Santini F, Herzka DA et al (2014) Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics 34:217-233
Kumar Y, Hayashi D (2016) Role of magnetic resonance imaging in acute spinal trauma: a pictorial review. BMC Musculoskelet Disord 17:310
Mascalchi M, Dal Pozzo G, Bartolozzi C (1993) Effectiveness of the short TI inversion recovery (STIR) sequence in MR imaging of intramedullary spinal lesions. Magn Reson Imaging 11:17–25
Deshmane A, Gulani V, Griswold MA, Seiberlich N (2012) Parallel MR imaging. J Magn Reson Imaging 36:55–72
Sayah A, Jay AK, Toaff JS et al (2016) Effectiveness of a rapid lumbar spine MRI protocol using 3D T2-weighted SPACE imaging versus a standard protocol for evaluation of degenerative changes of the lumbar spine. AJR Am J Roentgenol 207:614-620
Chiavassa H, Sans N, Galy-Fourcade D et al (2000) [HASTE sequence and cine-MRI evaluation of the cervical spinal canal: evaluation in 11 healthy subjects]. J Radiol 81:611-617
Burke CJ, Samim M, Alizai H et al (2021) Clinical feasibility of 2D dynamic sagittal HASTE flexion-extension imaging of the cervical spine for the assessment of spondylolisthesis and cervical cord im**ement. Eur J Radiol 134:109447
Duerinckx AJ, Yu WD, El-Saden S et al (1999) MR imaging of cervical spine motion with HASTE. Magn Reson Imaging 17:371-381
Walter WR, Alizai H, Bruno M et al (2021) Real-time dynamic 3-T MRI assessment of spine kinematics: a feasibility study utilizing three different fast pulse sequences. Acta Radiol 62:58-66
Author information
Authors and Affiliations
Contributions
M. V. S., M. Y., and R. E. conceived the study. M. V. S. and M. Y. supervised and supported the study. M. V. S. analyzed the data, performed the statistical analysis, and drafted the initial manuscript. C. A., M. K., A. T, and G. L. collected and organized the data. M. Y. and J. C. interpreted the images. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Maria V. Spampinato: Siemens, Research grant not related to the subject of the paper; Bayer, Research grant, not related to the subject of the paper. No other financial relationships with commercial interests to disclose. Justin Chetta. Claire Adcock, Madison Kocher, Abigail Truitt, Georgia Lydon, Ramin Eskandari, Milad Yazdani: None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Spampinato, M.V., Chetta, J.A., Adcock, C. et al. Non-sedated fast spine magnetic resonance imaging in pediatric patients. Pediatr Radiol 53, 2478–2489 (2023). https://doi.org/10.1007/s00247-023-05760-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05760-0