Abstract
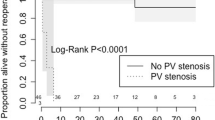
To evaluate the surgical outcomes of total anomalous pulmonary venous drainage focusing on survival, postoperative and pulmonary venous obstruction. Further investigate the role of primary sutureless technique in patients with preoperative pulmonary venous obstruction. Consecutive patients underwent total anomalous pulmonary venous drainage repair in our institution during Jan 2000 to Dec 2019 were enrolled into this retrospective analysis. Since 2016, sutureless repair was regularly applied in patients with preoperative pulmonary venous obstruction. All patients with preoperative pulmonary venous obstruction referred before 2016 had underwent traditional repair. A total of 95 patients were included. During follow-up time of 85 months, main endpoints were documented in 21 patients, including 9 (9.5%) early deaths, 3 (2.3%) late deaths and 9 (9.5%) postoperative pulmonary venous obstructions. Preoperative pulmonary venous obstruction was presented in 26 (27.4%) patients with more emergent surgery (14/26 vs 3/69, P < 0.001) was required. Main endpoints occurred more in patients with preoperative pulmonary venous obstruction (4/26 vs 5/69, P = 0.004). Patients experienced sutureless technique had a lower incidence of postoperative PVO at follow-up (0/11 versus 4/11, P = 0.045). Outcomes of surgical repair for total anomalous venous drainage are satisfactory. However, preoperative pulmonary venous obstruction may be accompanying unfavorable early deaths and postoperative pulmonary venous obstruction. Propensity matching analysis showed that sutureless technique was benefit for postoperative pulmonary venous obstruction without longer cardiopulmonary bypass and aortic cross-clamp time.


Similar content being viewed by others
References
Karamlou T, Gurofsky R, Al Sukhni E et al (2007) Factors associated with mor- tality and reoperation in 377 children with total anomalous pulmonary venous connection. Circulation 115:1591–1598
Kanter KR (2006) Surgical repair of total anomalous pulmonary venous connection. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 9:40–44
Yong MS, d’Udekem Y, Robertson T et al (2011) Outcomes of surgery for simple total anomalous pulmonary venous drainage in neonates. Ann Thorac Surg 91:1921–1927
Hancock Friesen CL, Zurakowski D, Thiagarajan RR et al (2005) Total anomalous pulmonary venous connection: an analysis of current management strategies in a single institution. Ann Thorac Surg. 79:596–606
Lacour-Gayet F, Zoghbi J, Serraf AE et al (1999) Surgical management of progressive pulmonary venous obstruction after repair of total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg. 117:679–687
Caldarone CA, Najm HK, Kadletz M, Freedom RM, Williams WG, Coles JG (1998) Relentless pulmonary vein stenosis after repair of total anomalous pulmonary venous drainage. Ann Thorac Surg 66:1514–1520
Rito Lo M, Gazzaz T, Wilder T et al (2015) Repair type influences mode of pulmonary vein stenosis in total anomalous pulmonary venous drainage. Ann Thorac Surg. 100:654–662
Shi G, Zhu Z, Chen J et al (2017) Total anomalous pulmonary venous connection: the current management strategies in a pediatric cohort of 768 patients. Circulation 135:48–58
Ou-Yang WB, Zhang H, Yang KM, Li SJ (2012) Modified anastomosis for repair of supracardiac total anomalous pulmonary venous connection in infants. J Card Surg 27:387–389
St Louis JD, Harvey BA, Menk JS et al (2012) Repair of “simple” total anomalous pulmonary venous connection: a review from the pediatric cardiac care consortium. Ann Thorac Surg 94:133–138
van de Wal HJ, Hamilton DI, Godman MJ, Harinck E, Lacquet LK, van Oort A (1992) Pulmonary venous obstruction following correction for total anomalous pulmonary venous drainage: a challenge. Eur J Cardiothorac Surg 6:545–549
Lahiri S, Wang Y, Caldarone CA, Morris SA (2020) Trends in infant mortality after TAPVR repair over 18 years in Texas and impact of hospital surgical volume. Pediatr Cardiol 41:77–87
Harada T, Nakano T, Oda S, Kado H (2019) Surgical results of total anomalous pulmonary venous connection repair in 256 patients. Interact Cardiovasc Thorac Surg 28:421–426
Hörer J, Neuray C, Vogt M et al (2013) What to expect after repair of total anomalous pulmonary venous connection: data from 193 patients and 2902 patient years. Eur J Cardiothorac Surg 44:800–807
Wilson WR Jr, Ilbawi MN, DeLeon SY et al (1992) Technical modifications for improved results in total anomalous pulmonary venous drainage. J Thorac Cardiovasc Surg. 103:861–870
Acknowledgements
We gratefully acknowledge the role of all our colleagues, perfusionists, nurses and others involved in the care of these babies.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of the Second Affiliated Hospital and Yuying Children's Hospital and individual consent for this retrospective analysis was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
**a, J., Ma, K., Ge, H. et al. Outcomes of Surgical Repair of Total Anomalous Pulmonary Venous Drainage: Role of Primary Sutureless Technique. Pediatr Cardiol 42, 1316–1323 (2021). https://doi.org/10.1007/s00246-021-02614-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02614-0