Abstract
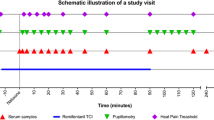
Surrogates may provide easy and quick access to information about pharmacological parameters of interest that can be directly measured only with difficulty. Surrogates have been proposed for opioid blood concentrations to replace invasive sampling, serving as a basis for target-controlled infusion systems to optimize analgesia. We aimed at identifying surrogates of remifentanil steady-state blood concentrations with relevance for its clinical, in particular, analgesic, effects. A “single ascending dose” study design assessed concentration-dependent effects of remifentanil in a double-blind randomized fashion in 16 healthy volunteers. Remifentanil was administered by means of computerized infusion aimed at steady-state effect–site concentrations of 0, 1.2, 1.8, 2.4, 3, 3.6, 4.8, and 6 ng/ml (one concentration per subject, two subjects per concentration). Arterial remifentanil blood concentrations were measured during apparent steady state. Pharmacodynamic parameters were measured at baseline and during steady-state conditions. Potential surrogate parameters included the pupil diameter, the amplitude of pupil light reflex, and the performance in a visual tracking task. Clinical parameters were analgesia to experimental pain, nausea, tiredness, and visual acuity. Remifentanil blood concentrations were well predicted by its effects on the pupil light reflex amplitude, better than by its miotic effects. However, the best prediction for both remifentanil blood concentrations and analgesic effects was obtained using a combination of three surrogate parameters (pupil diameter, light reflex amplitude, and tracking performance). This combination of pharmacodynamic parameters provided even better predictions of analgesia than could be obtained using the measured opioid blood concentrations. Develo** surrogates only for opioid blood concentrations is insufficient when opioid effects are the final goal. Combining pharmacodynamic surrogate parameters seems to provide a promising approach to obtain acceptable predictions of relevant clinical effects, with better results than obtained with measuring or estimating blood concentrations.


Similar content being viewed by others
Notes
These parameters had been obtained by a standard fit of pooled data using a classical sigmoid pharmacodynamic model. Details about goodness-of-fit are: the standard error of estimate of EC50 = 0.1, E max did not significantly differ from a value of −100 % and had therefore been fixed, and goodness-of-fit, R 2 = 0.984.
Again, these values had been obtained using a standard sigmoidal model: The standard error of the estimate of EC50 was 4; E max did not significantly differ from a value of −100 % and had therefore been fixed, and R 2 was 0.274.
References
Angst MS, Clark JD (2006) Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology 104:570–587
Bouman-Thio E, Franson K, Miller B, Getsy J, Cohen A, Bai SA, Yohrling J, Frederick B, Marciniak S, Jiao Q, Jang H, Davis H, Burggraaf J (2008) A phase I, single and fractionated, ascending-dose study evaluating the safety, pharmacokinetics, pharmacodynamics, and immunogenicity of an erythropoietin mimetic antibody fusion protein (CNTO 528) in healthy male subjects. J Clin Pharmacol 48:1197–1207
Bright E, Baines DB, French BG, Cartmill TB (1993) Upper limb amputation following radial artery cannulation. Anaesth Intensive Care 21:351–353
Buch H, Vinding T, Nielsen NV (2001) Prevalence and causes of visual impairment according to World Health Organization and United States criteria in an aged, urban Scandinavian population: the Copenhagen City Eye Study. Ophthalmology 108:2347–2357
Drummond JC, Brann CA, Perkins DE, Wolfe DE (1991) A comparison of median frequency, spectral edge frequency, a frequency band power ratio, total power, and dominance shift in the determination of depth of anesthesia. Acta Anaesthesiol Scand 35:693–699
DuMouchel WH, O'Brien FL (1989) Integrating a robust option into a multiple regression computing environment. Proceedings of the 21st Symposium on the Interface, American Statistical Association
Egan TD (1995) Remifentanil pharmacokinetics and pharmacodynamics: a preliminary appraisal. Clin Pharmacokinet 29:80–94
Egan TD, Lemmens HJ, Fiset P, Hermann DJ, Muir KT, Stanski DR, Shafer SL (1993) The pharmacokinetics of the new short-acting opioid remifentanil (GI87084B) in healthy adult male volunteers. Anesthesiology 79:881–892
Egan TD, Minto CF, Hermann DJ, Barr J, Muir KT, Shafer SL (1996) Remifentanil versus alfentanil: comparative pharmacokinetics and pharmacodynamics in healthy adult male volunteers [published erratum appears in Anesthesiology 1996 Sep;85(3):695]. Anesthesiology 84:821–833
Egan TD, Kern SE, Muir KT, White J (2004) Remifentanil by bolus injection: a safety, pharmacokinetic, pharmacodynamic, and age effect investigation in human volunteers. Br J Anaesth 92:335–343
Evans PJ, Kerr JH (1975) Arterial occlusion after cannulation. Br Med J 3:197–199
Hermann DJ, Egan TD, Muir KT (1999) Influence of arteriovenous sampling on remifentanil pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther 65:511–518
Holford NH, Sheiner LB (1982) Kinetics of pharmacologic response. Pharmacol Ther 16:143–166
Hosmer DW, Taber S, Lemeshow S (1991) The importance of assessing the fit of logistic regression models: a case study. Am J Public Health 81:1630–1635
Hummel T, Kobal G (2001) Olfactory event-related potentials. In: Simon SA, Nicolelis MAL (eds) Methods in chemosensory research. CRC Press, Boca Raton, London, New York, Washington, D.C., pp 429–464
Hummel T, Hummel C, Friedel I, Pauli E, Kobal G (1994) A comparison of the antinociceptive effects of imipramine, tramadol and anpirtoline. Br J Clin Pharmacol 37:325–333
Jiang LJ, Wang M, Or YS (2009) Pharmacokinetics of EDP-420 after ascending single oral doses in healthy adult volunteers. Antimicrob Agents Chemother 53:1786–1792
Johnson NL, Kotz S, Balakrishnan N (1994) Lognormal distributions Continuous univariate distributions, JohnWiley & Sons, New York
Kern SE, Stanski DR (2008) Pharmacokinetics and pharmacodynamics of intravenously administered anesthetic drugs: concepts and lessons for drug development. Clin Pharmacol Ther 84:153–157
Kharasch ED, Hoffer C, Walker A, Sheffels P (2003) Disposition and miotic effects of oral alfentanil: a potential noninvasive probe for first-pass cytochrome P4503A activity. Clin Pharmacol Ther 73:199–208
Kobal G (1985) Pain-related electrical potentials of the human nasal mucosa elicited by chemical stimulation. Pain 22:151–163
Koppert W, Sittl R, Scheuber K, Alsheimer M, Schmelz M, Schuttler J (2003) Differential modulation of remifentanil-induced analgesia and postinfusion hyperalgesia by S-ketamine and clonidine in humans. Anesthesiology 99:152–159
Kosek E, Jensen KB, Lonsdorf TB, Schalling M, Ingvar M (2009) Genetic variation in the serotonin transporter gene (5-HTTLPR, rs25531) influences the analgesic response to the short acting opioid Remifentanil in humans. Molecular Pain 5: 37
Lin L, Chang LW, Tsai CY, Hsu CH, Chung DT, Aronstein WS, Ajayi F, Kuzmak B, Lyon RA (2010) Dose escalation study of the safety, tolerability, and pharmacokinetics of nemonoxacin (TG-873870), a novel potent broad-spectrum nonfluorinated quinolone, in healthy volunteers. Antimicrob Agents Chemother 54:405–410
Lötsch J, Angst MS (2003) The mu-opioid agonist remifentanil attenuates hyperalgesia evoked by blunt and punctuated stimuli with different potency: a pharmacological evaluation of the freeze lesion in humans. Pain 102:151–161
Lötsch J, Darimont J, Skarke C, Zimmermann M, Hummel T, Geisslinger G (2001) Effects of the opioid remifentanil on olfactory function in healthy volunteers. Life Sci 69:2279–2285
Lötsch J, Dudziak R, Freynhagen R, Marschner J, Geisslinger G (2006) Fatal respiratory depression after multiple intravenous morphine injections. Clin Pharmacokinet 45:1051–1060
Lötsch J, Geisslinger G, Tegeder I (2009) Genetic modulation of the pharmacological treatment of pain. Pharmacol Ther 124:168–184
Lötsch J, Prüss H, Veh RW, Doehring A (2010) A KCNJ6 (Kir3.2, GIRK2) gene polymorphism modulates opioid effects on analgesia and addiction but not on pupil size. Pharmacogenet Genomics 20:291–297
Lötsch J, Doehring A, Mogil JS, Arndt T, Geisslinger G, Ultsch A (2013) Functional genomics of pain in analgesic drug development and therapy. Pharmacol Ther 139:60-70
Maher CE, Selley DE, Childers SR (2000) Relationship of mu opioid receptor binding to activation of G-proteins in specific rat brain regions. Biochem Pharmacol 59:1395–1401
Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, Billard V, Hoke JF, Moore KH, Hermann DJ, Muir KT, Mandema JW, Shafer SL (1997a) Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil I. Model development. Anesthesiology 86:10–23
Minto CF, Schnider TW, Shafer SL (1997b) Pharmacokinetics and pharmacodynamics of remifentanil II. Model application. Anesthesiology 86:24–33
Mitrovic I, Margeta-Mitrovic M, Bader S, Stoffel M, Jan LY, Basbaum AI (2003) Contribution of GIRK2-mediated postsynaptic signaling to opiate and alpha 2-adrenergic analgesia and analgesic sex differences. Proc Natl Acad Sci USA 100:271–276
Moskovitz BL, Benson CJ, Patel AA, Chow W, Mody SH, McCarberg BH, Kim MS (2011) Analgesic treatment for moderate-to-severe acute pain in the United States: patients' perspectives in the Physicians Partnering Against Pain (P3) survey. J Opioid Manag 7:277–286
Noh GJ, Kim KM, Jeong YB, Jeong SW, Yoon HS, Jeong SM, Kang SH, Linares O, Kern SE (2006) Electroencephalographic approximate entropy changes in healthy volunteers during remifentanil infusion. Anesthesiology 104:921–932
Oertel BG, Lötsch J (2013) Clinical pharmacology of analgesics assessed with human experimental pain models: bridging basic and clinical research. Br J Pharmacol 168:534–553
Oertel BG, Doehring A, Roskam B, Kettner M, Hackmann N, Ferreirós N, Schmidt PH, Lötsch J (2012a) Genetic–epigenetic interaction modulates μ-opioid receptor regulation. Hum Mol Genet 21:4751–4760
Oertel BG, Vermehren J, Zimmermann M, Huynh TT, Doehring A, Ferreiros N, Senzel S, Schmitz-Rixen T, Erbe M, Geisslinger G, Harder S, Angst MS, Lötsch J (2012b) Necessity and risks of arterial blood sampling in healthy volunteer studies. Clin Pharmacokinet 51:629–638
Padhi D, Jang G, Stouch B, Fang L, Posvar E (2011) Single-dose, placebo-controlled, randomized study of AMG 785, a sclerostin monoclonal antibody. J Bone Mineral Res Off J Am Soc Bone Mineral Res 26:19–26
Porreca F, Ossipov MH (2009) Nausea and vomiting side effects with opioid analgesics during treatment of chronic pain: mechanisms, implications, and management options. Pain Med 10:654–662
Sahinovic MM, Absalom AR, Struys MM (2010) Administration and monitoring of intravenous anesthetics. Curr Opin Anaesthesiol 23:734–740
Schwilden H, Stoeckel H (1993) Closed-loop feedback controlled administration of alfentanil during alfentanil-nitrous oxide anaesthesia. Br J Anaesth 70:389–393
Selinger K, Lanzo C, Sekut A (1994) Determination of remifentanil in human and dog blood by HPLC with UV detection. J Pharm Biomed Anal 12:243–248
Shafer SL, Varvel JR, Aziz N, Scott JC (1990) Pharmacokinetics of fentanyl administered by computer-controlled infusion pump. Anesthesiology 73:1091–1102
Sharpe LG, Pickworth WB (1985) Opposite pupillary size effects in the cat and dog after microinjections of morphine, normorphine and clonidine in the Edinger-Westphal nucleus. Brain Res Bull 15:329–333
Sim LJ, Selley DE, **ao R, Childers SR (1996) Differences in G-protein activation by mu- and delta-opioid, and cannabinoid, receptors in rat striatum. Eur J Pharmacol 307:97–105
Simone CB 2nd, Vapiwala N, Hampshire MK, Metz JM (2012) Cancer patient attitudes toward analgesic usage and pain intervention. Clin J Pain 28:157–162
Sinatra R (2010) Causes and consequences of inadequate management of acute pain. Pain Med 11:1859–1871
Skarke C, Darimont J, Schmidt H, Geisslinger G, Lotsch J (2003) Analgesic effects of morphine and morphine-6-glucuronide in a transcutaneous electrical pain model in healthy volunteers. Clin Pharmacol Ther 73:107–121
Spearman C (1987) The proof and measurement of association between two things. By C. Spearman, 1904. Am J Psychol 100:441–471
Tzabazis A, Ihmsen H, Schywalsky M, Schwilden H (2004) EEG-controlled closed-loop dosing of propofol in rats. Br J Anaesth 92:564–569
Wu CL, Raja SN (2011) Treatment of acute postoperative pain. Lancet 377:2215–2225
Acknowledgments
All the authors declare that there are no personal financial holdings that could be perceived as constituting a potential conflict of interests. All authors, except JL, further declare that no financial support or compensation has been received from any individual or corporate entity over the past 3 years for research or professional service. One author, JL, declares that he received research support from Cortex Pharmaceuticals, Irvine, California, USA, and received counselling compensation from BioMed Valley Discoveries, Inc., Kansas City, USA, and a presentation honorarium from Janssen-Cilag, all without any relation to the present analysis, which was an effort in the context of the “Landesoffensive zur Entwicklung wissenschaftlich-ökonomischer Exzellenz”: “LOEWE-Schwerpunkt: Anwendungsorientierte Arzneimittelforschung”. The study medication had been provided by Glaxo Wellcome GmbH & Co., Hamburg, Germany, who had no further involvement in the project, including planning, performance, data analysis, and writing of this report. There was no further assistance with the study. There was no further financial support or sponsorship. Data from the reported study, non-redundant with the present analysis, have been published in another context in Life Sciences 2001;69(19):2279–85 and Clin Pharmacokinet 2012;51(10):629–38.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 559 kb)
Rights and permissions
About this article
Cite this article
Lötsch, J., Skarke, C., Darimont, J. et al. Non-invasive combined surrogates of remifentanil blood concentrations with relevance to analgesia. Naunyn-Schmiedeberg's Arch Pharmacol 386, 865–873 (2013). https://doi.org/10.1007/s00210-013-0889-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-013-0889-5