Abstract
Purpose
Despite the comprehensive literature on the anatomical risk factors for patellar dislocation, knowledge on the risk factors for subsequent osteochondral fracture (OCF) remains limited.
Methods
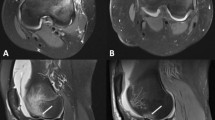
Magnetic resonance imaging was used to compare measures of patellofemoral anatomy in patients with OCF after patellar dislocation and propensity score matched patients without OCF. For differing measures, limit values showing a 50% probability for the occurrence of OCF were calculated using predictive logistic regression modelling. Proportions of abnormal measures in the groups were compared using Chi-square test. The association of anatomical measures with OCF location was examined by comparing subgroup mean values in the different OCF locations.
Results
Propensity score matching provided a total of 111 matched pairs of patients with OCF and patients without OCF. The patients with and without OCF differed in patellotrochlear index (PTI; 0.54 [95% CI 0.52–0.57] vs. 0.47 [95% CI 0.45–0.49]; p < 0.001), tibial tubercle-posterior cruciate ligament distance (TT-PCL; 21.6 mm [95% CI 21.0–22.3 mm] vs. 20.5 mm [95% CI 20.0–21.1 mm]; p = 0.013), trochlear depth (2.5 mm [95% CI 2.3–2.7 mm] vs. 3.0 mm [95% CI 2.8–3.2 mm]; p < 0.001) trochlear facet asymmetry ratio (0.54 [95% CI 0.51–0.57] vs. 0.43 [95% CI 0.42–0.45]; p < 0.001) and trochlear condyle asymmetry ratio (1.04 [95% CI 1.03–1.04] vs. 1.05 [95% CI 1.04–1.05]; 0.013. Thresholds for increased OCF risk were > 0.51 for PTI > 21.1 mm for TT-PCL < 2.8 mm for trochlear depth > 0.48 for trochlear facet asymmetry ratio and < 1.04 for trochlear condyle asymmetry ratio.
Conclusion
In patients with OCF after patellar dislocation, trochlear configuration and patella vertical location were closer to normal anatomy, whereas patella lateralization was more severe when compared to patients without OCF. These anatomical factors contribute to the risk of OCF during patellar dislocation.
Level of evidence
III.



Similar content being viewed by others
References
Arendt EA, England K, Agel J, Tompkins MA (2017) An analysis of knee anatomic imaging factors associated with primary lateral patellar dislocations. Knee Surg Sports Traumatol Arthrosc 25:3099–3107
Askenberger M, Janarv PM, Finnbogason T, Arendt EA (2016) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med 45:50–58
Dejour D, Le Coultre B (2018) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 26:8–15
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA (2020) Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med 48:2552–2562
Parikh SN, Lykissas MG, Gkiatas I (2018) Predicting risk of recurrent patellar dislocation. Curr Rev Musculoskelet Med 11:253–260
Askenberger M, Arendt EA, Ekström W, Voss U, Finnbogason T, Janarv P-M (2016) Medial patellofemoral ligament injuries in children with first-time lateral patellar dislocations: a magnetic resonance imaging and arthroscopic study. Am J Sports Med 44:152–158
Zheng L, Ding H-y, Feng Y, Sun B-s, Zhu L-l, Zhang G-y (2020) Gender-related differences in concomitant articular injuries after acute lateral patellar dislocation. Injury. https://doi.org/10.1016/j.injury.2020.10.065
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14:513–515
Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ (2018) Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health 10:146–151
Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H (2008) Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc 40:606–611
Sanders TL, Pareek A, Johnson NR, Stuart MJ, Dahm DL, Krych AJ (2017) Patellofemoral arthritis after lateral patellar dislocation: a matched population-based analysis. Am J Sports Med 45:1012–1017
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225:736–743
Seeley MA, Knesek M, Vanderhave KL (2013) Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop 33:511–518
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Statistics Finland. www.stat.fi/index_en.html
Finnish Ministry of Justice (2010) Medical research act, 488/1999. Edita Publishing Ltd.
World Health Organization (2004) ICD-10: international statistical classification of diseases and related health problems: tenth revision, 2nd edn. World Health Organization
Dvorak J, George J, Junge A, Hodler J (2007) Age determination by magnetic resonance imaging of the wrist in adolescent male football players. Br J Sports Med 41:45–52
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104
Caton J, Deschamps G, Chambat P, Lerat J, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317
Biedert RM, Albrecht S (2006) The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc 14:707–712
Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G (2014) Tibial tubercle-trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg 96:318–324
Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S (2012) Tibial tubercle–posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med 40:1119–1125
Pfirrmann CW, Zanetti M, Romero J, Hodler J (2000) Femoral trochlear dysplasia: MR findings. Radiology 216:858–864
Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA (2000) Patellar instability: assessment on MR images by measuring the lateral trochlear inclination—initial experience. Radiology 216:582–585
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Arendt EA, Askenberger M, Agel J, Tompkins MA (2018) Risk of redislocation after primary patellar dislocation: a clinical prediction model based on magnetic resonance imaging variables. Am J Sports Med 46:3385–3390
Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW (2018) High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc 26:1204–1209
Kuss O (2013) The z-difference can be used to measure covariate balance in matched propensity score analyses. J Clin Epidemiol 66:1302–1307
Brady JM, Rosencrans AS, Stein BES (2018) Use of TT-PCL versus TT-TG. Curr Rev Musculoskelet Med 11:261–265
Danova N, Colopy S, Radtke C, Kalscheur V, Markel M, Vanderby R Jr et al (2003) Degradation of bone structural properties by accumulation and coalescence of microcracks. Bone 33:197–205
Muir P, McCarthy J, Radtke C, Markel M, Santschi EM, Scollay M et al (2006) Role of endochondral ossification of articular cartilage and functional adaptation of the subchondral plate in the development of fatigue microcracking of joints. Bone 38:342–349
Nagaraja S, Couse TL, Guldberg RE (2005) Trabecular bone microdamage and microstructural stresses under uniaxial compression. J Biomech 38:707–716
Ito MM, Kida MY (2000) Morphological and biochemical re-evaluation of the process of cavitation in the rat knee joint: cellular and cell strata alterations in the interzone. J Anat 197:659–679
Miller T, Staron R, Feldman F (1996) Patellar height on sagittal MR imaging of the knee. Am J Roentgenol 167:339–341
Biedert RM, Tscholl PM (2017) Patella alta: a comprehensive review of current knowledge. Am J Orthop 46:290–300
Daynes J, Hinckel BB, Farr J (2016) Tibial tuberosity—posterior cruciate ligament distance. J Knee Surg 29:471–477
Author information
Authors and Affiliations
Contributions
Coordination of tudy conduction: MU, VP, JR, VM, JP. Study design: MU, VP, JR, JP. Data collection: MU, VP, SH, GK. Statistical analysis: MU, VP. Data interpretation: MU, VP, JR, VM, HN, JP. Clinical consultant: HN. Manuscript preparation: MU, VP. Critical review of the manuscript: JR, VM, JP, HN, GK, SH. Approval of the final draft: MU, VP, JR, VM, JP, HN, GK, SH.
Corresponding author
Ethics declarations
Conflict of interest
None.
Funding
None.
Ethical approval
Due to the retrospective study design with the data gathered only from electronic patient records without affecting the treatment of the patients, an ethical committee approval was not obtained or needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uimonen, M., Ponkilainen, V., Hirvinen, S. et al. The risk of osteochondral fracture after patellar dislocation is related to patellofemoral anatomy. Knee Surg Sports Traumatol Arthrosc 29, 4241–4250 (2021). https://doi.org/10.1007/s00167-021-06547-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06547-2