Abstract
Purpose
Patients with surgically treated acetabular fractures using extensive dissection of hip muscles demonstrate an incomplete biomechanical recovery and limited joint mobility during movement. The purpose of this study was to evaluate the early biomechanical outcome in a series of patients with acetabular fractures treated using the less invasive anatomical pararectus approach.
Methods
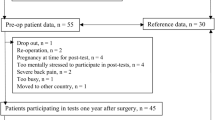
Eight patients (48 ± 14 years, BMI 25.8 ± 3 kg/m2) were investigated 3.8 ± 1.3 months after surgery and compared to matched controls (49 ± 13 years, BMI 26 ± 2.8 kg/m2). Trunk and lower extremity kinematics and kinetics during gait and stair climb were calculated. SF-12 and the Merle d’Aubigné score were used for functional evaluation. Statistical analysis was conducted using Mann–Whitney test and Student’s t test. Effect sizes were calculated using Cohen’s d.
Results
No group differences for lower extremity kinematics during walking and stair climbing were found. During walking, patients showed significant reductions (p < 0.05) of the vertical ground reaction force (8%) and knee and hip extension moments (29 and 27%). Ipsilateral trunk lean was significantly increased by 3.1° during stair descend while reductions of vertical ground reaction force were found for stair ascend (7%) and descend (20%). Hip extension moment was significantly reduced during stair descend by 37%. Patients revealed acceptable SF-12 physical and mental component outcomes and a good rating for the Merle d’Aubigné score (15.9 ± 1.7).
Conclusion
Patients showed some biomechanical restrictions that can be related to residual deficits in weight bearing capacity and strength of the hip muscles. In contrast, an immediate recovery of mobility was achieved by preserving lower extremity and pelvic movement. Therefore, the pararectus approach can serve as a viable strategy in the surgical treatment of acetabular fractures.
Clinical trial
Trial registration number DRKS00011308, 11/14/2016, prospectively registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetabular fractures demonstrate an overall incidence of about 2–8% of all fractures and may rapidly lead to long lasting physical limitations and functional disability [1]. Regarding internal fracture fixation, various surgical access strategies such as the ilioinguinal approach, the Kocher–Langenbeck approach and the Stoppa approach have proven to be effective. However, sufficient visualisation of the fracture site to achieve anatomical reduction is always a challenge in these approaches which could have a significant impact on the functional outcome [2]. In this context, the less invasive anatomical pararectus approach suggests an alternative access route to surgically stabilise displaced acetabular fractures. Its anatomical tissue-conserving shape protects important functional structures and demonstrates particular advantages in terms of visualisation compared to other approaches. This allows better possibilities for anatomical fracture reduction, achieving a step-free reduction in more than 90% of cases [3]. Radiological evaluation also showed a comparable outcome with other minimally invasive surgical procedures while achieving shorter operation time [4, 5]. In this context, a significantly improved reduction in joint space with similar complication rates was found, when the pararectus approach was compared to the ilioinguinal approach [6]. A crucial aspect in the rehabilitation process following comminute acetabular fractures is the early recovery of mobility. Current surgical interventions that require extensive dissection of major hip muscles demonstrated to have a negative impact on walking quality [7, 8]. Although the pararectus approach indicates to be a promising anatomical access to address acetabular fractures involving the quadrilateral plate, clinical studies on the early postoperative biomechanical outcome and functional mobility are still missing. Instrumented gait analysis can serve as a viable quality tool in the objective assessment of human movement in a clinical setting [9]. In so far, acetabular fractures using the anterior ilioinguinal or the posterior Kocher–Langenbeck approach demonstrated incomplete recovery of hip and pelvic biomechanics including limited mobility and an altered functional outcome after surgery [10,11,12]. However, most of these gait studies examined patients more than 12 months after surgery, and the immediate postoperative result, therefore, is only partially reflected. The pararectus approach is expected to result in less muscle damage and due to its minimally invasive character it is intended to achieve an early and fast recovery after surgery [13, 37]. Using a patient adjusted walking speed for our matched controls would have been beneficial for data comparison. Another limitation of this study is that no biomechanical long-term adaptions using the pararectus approach were investigated. However, the main study aim was to evaluate gait restoration during the early postoperative phase (up to 6 months after surgery) where full weight bearing is regained and supervised physical therapy is completed. Since no group comparisons regarding other surgical treatments were performed in this study, we also cannot directly state whether the pararectus approach provides a significant advantage to other treatment strategies. In this context, a systematic comparison might be suggested in the future.
Conclusion
Patients with isolated unilateral acetabular fractures treated using the pararectus approach showed an almost physiologic dynamic joint mobility of the lower extremities and clinically demonstrated a good hip function. However, reduced joint moments and vertical ground reaction forces during walking and stair descend indicate that deficits in weight bearing capacity and dynamic motor control are still present. In this context, a diminished self-reported physical and mental state compared to healthy controls was also observed. Nonetheless, our findings confirm that lower extremity joint mobility during walking and stair climbing can recover in a very early phase after surgery. Thus, the less invasive pararectus approach appeared to be a viable treatment strategy of acetabular fractures to achieve a promising functional baseline for the ongoing rehabilitation process.
Data availability
The datasets analysed during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Fritz T, Veith NT, Braun BJ, Pohlemann T, Herath SC. Beckenchirurgie—akutversorgungdiagnostik der beckenfrakturenapparativediagnostik. OP-J. 2018;34:26–32.
Keel MJB, et al. The Pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Jt Surg Br. 2012;94B(3):405–11. https://doi.org/10.1302/0301-620X.94B3.27801.
Keel MJB, Thannheimer A. ThePararectus approach—innovation in acetabular surgery. OrthopUnfallchirurgischePrax. 2016;5(11):616–20. https://doi.org/10.14512/oew310327.
Wenzel L, et al. The Pararectus approach in acetabular surgery: radiological and clinical outcome. J Orthop Trauma. 2020;34(2):82–8. https://doi.org/10.1097/BOT.0000000000001636.
Chui KH, Chan CCD, Ip KC, Lee KB, Li W. Three-dimensional navigation-guided percutaneous screw fixation for nondisplaced and displaced pelvi-acetabular fractures in a major trauma centre. IntOrthop. 2018;42(6):1387–95. https://doi.org/10.1007/s00264-017-3659-z.
Märdian S, Schaser KD, Hinz P, Wittenberg S, Haas NP, Schwabe P. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: a direct comparison. Bone Jt J. 2015;97B(9):1271–8. https://doi.org/10.1302/0301-620X.97B9.35403.
Mayo K. Surgical approaches to the acetabulum. Tech Orthop. 1990;4:24–35.
Mehlman C, Meiss L, Di Pasquale T. Hyphenated-history: the Kocher–Langenbeck surgical approach. J OrthopSurg Res. 2000;14(1):60–4.
Klöpfer-Krämer I, Brand A, Wackerle H, Müßig J, Kröger I, Augat P. Gait analysis—available platforms for outcome assessment. Injury. 2019. https://doi.org/10.1016/j.injury.2019.11.011.
Kubota M, et al. Changes in gait pattern and hip muscle strength after open reduction and internal fixation of acetabular fracture. Arch Phys Med Rehabil. 2012;93(11):2015–21. https://doi.org/10.1016/j.apmr.2012.01.016.
Engsberg JR, Steger-May K, Anglen JO, Borrelli J. An analysis of gait changes and functional outcome in patients surgically treated for displaced acetabular fractures. J Orthop Trauma. 2009;23(5):346–53. https://doi.org/10.1097/BOT.0b013e3181a278cc.
Borrelli J, Goldfarb C, Ricci W, Wagner JM, Engsberg JR. Functional outcome after isolated acetabular fractures. J Orthop Trauma. 2002;16(2):73–81. https://doi.org/10.1097/00005131-200202000-00001.
von Rottkay E, Rackwitz L, Rudert M, Nöth U, Reichert JC. Function and activity after minimally invasive total hip arthroplasty compared to a healthy population. IntOrthop. 2018;42(2):297–302. https://doi.org/10.1007/s00264-017-3541-z.
Zhao HY, De Kang P, **a YY, Shi XJ, Nie Y, Pei FX. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplast. 2017;32(11):3421–8. https://doi.org/10.1016/j.arth.2017.05.056.
Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. J Bone Jt Surg. 1964;46A(8):1615–75.
Ugino FK, Righetti CM, Alves DPL, Guimarães RP, Honda EK, Ono NK. Evaluation of the reliability of the modified Merle d’Aubigné and Postel method. ActaOrtop Bras. 2012;20(4):213–7. https://doi.org/10.1590/S1413-78522012000400004.
Gandek B, et al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. J ClinEpidemiol. 1998;51(11):1171–8. https://doi.org/10.1016/S0895-4356(98)00109-7.
Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8(3):383–92. https://doi.org/10.1002/jor.1100080310/full (Accessed 21 Mar 2016).
Davis RB, Ounpuu S, Tyburski D, Gage JR. A gait analysis data collection technique. Hum MovSci. 1991;10:575–87.
Perry J, Burnfield J. Gait analysis—normal and pathological function. 2nd ed. Thorofare: SLACK Incorporated; 2010.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Philadelphia: Lawrence Erlbaum Associates; 1988. p. 567.
Bennett D, Ogonda L, Elliott D, Humphreys L, Beverland DE. Comparison of gait kinematics in patients receiving minimally invasive and traditional hip replacement surgery: a prospective blinded study. Gait Posture. 2006;23(3):374–82. https://doi.org/10.1016/j.gaitpost.2005.04.008.
Madsen MS, et al. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res. 2004;22:44–50. https://doi.org/10.1016/j.jelekin.2017.11.004.
Rutherford DJ, Hubley-Kozey C. Explaining the hip adduction moment variability during gait: implications for hip abductor strengthening. ClinBiomech. 2009;24(3):267–73. https://doi.org/10.1016/j.clinbiomech.2008.12.006.
Wesseling M, et al. Gait alterations to effectively reduce hip contact forces. J Orthop Res. 2015;33(7):1094–102. https://doi.org/10.1002/jor.22852.
Stansfield BW, et al. Sagittal joint kinematics, moments, and powers are predominantly characterized by speed of progression, not age, in normal children. J PediatrOrthop. 2001;21(3):403–11. https://doi.org/10.1097/00004694-200105000-00027.
Queen RM, Newman ET, Abbey AN, Vail TP, Bolognesi MP. Stair ascending and descending in hip resurfacing and large head total hip arthroplasty patients. J Arthroplast. 2013;28(4):684–9. https://doi.org/10.1016/j.arth.2012.07.020.
Stacoff A, Diezi C, Luder G, Stüssi E, Kramers-De Quervain IA. Ground reaction forces on stairs: effects of stair inclination and age. Gait Posture. 2005;21(1):24–38. https://doi.org/10.1016/j.gaitpost.2003.11.003.
Bergmann G, et al. Hip forces and gait patterns from rountine activities. J Biomech. 2001;34:859–71.
Mündermann A, Asay JL, Mündermann L, Andriacchi TP. Implications of increased medio-lateral trunk sway for ambulatory mechanics. J Biomech. 2008;41(1):165–70. https://doi.org/10.1016/j.jbiomech.2007.07.001.
Arima Y, Tateuchi H, Mori K, Wakida M, Kim KH, Hase K. Relationship between vertical ground reaction force and muscle strength while climbing stairs after total hip arthroplasty. Clin Biomech. 2020;78:2–7. https://doi.org/10.1016/j.clinbiomech.2020.105088.
Morfeld M, Kirchberger I, Bullinger M. Fragebogenzumgesundheitszustand; Deutsche version des short form-36 health survey 2, ergänzte und überarbeiteteauflage manual. HogrefeVerlag GmbH & Co; 2011.
Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenicacetabular fractures involving the quadrilateral plate. Injury. 2011;42(10):1130–4. https://doi.org/10.1016/j.injury.2010.11.060.
Chémaly O, Hebert-Davies J, Rouleau DM, Benoit B, Laflamme GY. Heterotopic ossification following total hip replacement for acetabular fractures. J Bone Jt Surg. 2013;95-B(1):95–100. https://doi.org/10.1302/0301-620X.95B1.29721.
von Rüden C, et al. Thepararectus approach for internal fixation of acetabular fractures involving the anterior column: evaluating the functional outcome. IntOrthop. 2019;43(6):1487–93. https://doi.org/10.1007/s00264-018-4148-8.
Moed BR, Yu PH, Gruson KI. Functional outcomes of acetabular fractures. J Bone JtSurg. 2003;85(10):1879–83. https://doi.org/10.2106/00004623-200310000-00002.
Schwartz MH, Rozumalski A, Trost JP. The effect of walking speed on the gait of typically develo** children. J Biomech. 2008;41(8):1639–50. https://doi.org/10.1016/j.jbiomech.2008.03.015.
Funding
Open access funding provided by Paracelsus Medical University.
Author information
Authors and Affiliations
Contributions
Study conception and design: MP, CvR, AB, and PA. Data acquisition: CP, AB, and LW. Data analysis: AB, CP, and CvR. Data interpretation: all authors. Drafting/revision of the work for intellectual content and context: AB, CvR, PA, and MP. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was conducted in accordance to the guidelines of the Declaration of Helsinki of the World Medical Association, approved by the national ethics committee (Bavarian Medical Association, study no. 16043) and registered with the German Clinical Trials Register (DRKS00011308).
Consent to participate
Written informed consent to participate was obtained from the patients.
Consent to publication
Patients signed informed consent regarding publishing their data and photographs.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brand, A., von Rüden, C., Probst, C. et al. Early biomechanical outcome in patients with acetabular fractures treated using the pararectus approach: a gait and stair climb analysis study. Eur J Trauma Emerg Surg 48, 1307–1316 (2022). https://doi.org/10.1007/s00068-021-01655-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01655-7