Abstract
Objective
Indirect bypass surgery, which induces spontaneous neoangiogenesis in ischemic brain tissue and improves cerebral blood flow, is an effective treatment for moyamoya disease (MMD). The time course of neoangiogenesis development has not yet been investigated. This study aimed to determine the critical period of neovascularization after indirect bypass in MMD patients.
Methods
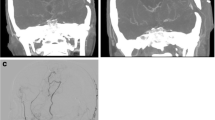
Patients with MMD who underwent indirect bypass surgery at Peking University International Hospital between January 2015 and October 2017 were retrospectively reviewed. Surgically treated hemispheres with short-term (3–6 months) and long-term (1 year) follow-up digital subtraction angiography (DSA) were included. The effects of revascularization were evaluated on lateral and anteroposterior views using angiography and compared between two follow-ups of the same hemisphere.
Results
This study included 25 hemispheres from 24 MMD patients (mean age: 22.48 ± 14.83 years), among whom 13 were pediatric patients and 12 were adults. Qualitative measurements including the Matsushima scale and coverage of neoangiogenesis on anteroposterior views were not significantly different between the short term and long term (P = 0.083 and P = 0.157, respectively). Quantitative measurements including the greatest width and height of the area covered by neovascularization on lateral views of DSA and the greatest depth of neovascularization penetration on anteroposterior views (P = 0.488, 0.298 and 0.527, respectively) were also not significantly different. The mean count of newly formed veins was more at long-term than short-term follow-up (5.5 ± 2.5 vs. 5.1 ± 2.4, P = 0.005). Subgroup analysis of pediatric patients and adults yielded the same results as in the whole series.
Conclusion
After indirect bypass surgery, the major time window of arterial neoangiogenesis development was within 6 months after surgery. The general effect of revascularization was very similar in the short and long term; therefore, a follow-up angiography scheduled at 6 months after surgery is recommended. Growth of veins might continue after 6 months.






Similar content being viewed by others
References
Fukui M, Kono S, Sueishi K, Ikezaki K. Moyamoya disease. Neuropathology. 2000;20 Suppl:S61-4.
Smith ER. Moyamoya arteriopathy. Curr Treat Options Neurol. 2012;14:549–56.
Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226–37.
Sun H, Wilson C, Ozpinar A, Safavi-Abbasi S, Zhao Y, Nakaji P, Wanebo JE, Spetzler RF. Perioperative complications and long-term outcomes after bypasses in adults with moyamoya disease: a systematic review and meta-analysis. World Neurosurg. 2016;92:179–88.
Macyszyn L, Attiah M, Ma TS, Ali Z, Faught R, Hossain A, Man K, Patel H, Sobota R, Zager EL, Stein SC. Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg. 2017;126:1523–9.
Zhao M, Deng X, Zhang D, Wang S, Zhang Y, Wang R, Zhao J. Risk factors for and outcomes of postoperative complications in adult patients with moyamoya disease. J Neurosurg. 2018;30:1-12.
Ogiwara H, Morota N. Bifrontal encephalogaleosynangiosis for children with moyamoya disease. J Neurosurg Pediatr. 2012;10:246–51.
Kawamoto H, Kiya K, Mizoue T, Ohbayashi N. A modified burr-hole method ‘galeoduroencephalosynangiosis’ in a young child with moyamoya disease. A preliminary report and surgical technique. Pediatr Neurosurg. 2000;32:272–5.
Kim SK, Wang KC, Kim IO, Lee DS, Cho BK. Combined encephaloduroarteriosynangiosis and bifrontal encephalogaleo (periosteal) synangiosis in pediatric moyamoya disease. Neurosurgery. 2008;62(6 Suppl 3):1456-64.
Patel NN, Mangano FT, Klimo P Jr.. Indirect revascularization techniques for treating moyamoya disease. Neurosurg Clin N Am. 2010;21:553–63.
Acker G, Fekonja L, Vajkoczy P. Surgical management of moyamoya disease. Stroke. 2018;49:476–82.
Adelson PD, Scott RM. Pial synangiosis for moyamoya syndrome in children. Pediatr Neurosurg. 1995;23:26–33.
Ishii Y, Tanaka Y, Momose T, Yamashina M, Sato A, Wakabayashi S, Maehara T, Nariai T. Chronologic evaluation of cerebral hemodynamics by dynamic susceptibility contrast magnetic resonance imaging after indirect bypass surgery for moyamoya disease. World Neurosurg. 2017;108:427–35.
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases. Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo). 2012;52:245-66.
Matsushima T, Inoue T, Suzuki SO, Fujii K, Fukui M, Hasuo K. Surgical treatment of moyamoya disease in pediatric patients—comparison between the results of indirect and direct revascularization procedures. Neurosurgery. 1992;31:401–5.
Nakashima H, Meguro T, Kawada S, Hirotsune N, Ohmoto T. Long-term results of surgically treated moyamoya disease. Clin Neurol Neurosurg. 1997;99 Suppl 2:S156-61.
Park SE, Kim JS, Park EK, Shim KW, Kim DS. Direct versus indirect revascularization in the treatment of moyamoya disease. J Neurosurg. 2018;129:480-9.
Kim T, Oh CW, Bang JS, Kim JE, Cho WS. Moyamoya disease: treatment and outcomes. J Stroke. 2016;18:21–30.
Goda M, Isono M, Ishii K, Kamida T, Abe T, Kobayashi H. Long-term effects of indirect bypass surgery on collateral vessel formation in pediatric moyamoya disease. J Neurosurg. 2004;100(2 Suppl Pediatrics):156-62.
Dai DW, Zhao WY, Zhang YW, Yang ZG, Li Q, Xu B, Ma XL, Tian B, Liu JM. Role of CT perfusion imaging in evaluating the effects of multiple burr hole surgery on adult ischemic moyamoya disease. Neuroradiology. 2013;55:1431–8.
Liu JJ, Steinberg GK. Direct versus indirect bypass for moyamoya disease. Neurosurg Clin N Am. 2017;28:361–74.
Kashiwagi S, Yamashita T, Katoh S, Kitahara T, Nakashima K, Yasuhara S, Ito H. Regression of moyamoya vessels and hemodynamic changes after successful revascularization in childhood moyamoya disease. Acta Neurol Scand Suppl. 1996;166:85–8.
Houkin K, Kamiyama H, Abe H, Takahashi A, Kuroda S. Surgical therapy for adult moyamoya disease. Can surgical revascularization prevent the recurrence of intracerebral hemorrhage? Stroke. 1996;27:1342–6.
Wang MY, Steinberg GK. Rapid and near-complete resolution of moyamoya vessels in a patient with moyamoya disease treated with superficial temporal artery-middle cerebral artery bypass. Pediatr Neurosurg. 1996;24:145–50.
Acknowledgements
We thank Chunxue Wu and **g Yuan for their contribution in assessment of radiological images.
Funding
This study was funded by the Ministry of Science and Technology of China, National Key Technology Research and Development Program (2015BAI12B04), by the National Natural Science Foundation of China (H0906 81571110 to Y.L. Zhao) and by the Training Plan of High-Level Technical Talents in the Bei**g Municipal Bureau of Health (2015-3-041).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Zhao, J. Lu, Q. Zhang, Y. Zhang, D. Zhang, R. Wang and Y. Zhao declare that they have no competing interests.
Additional information
Note
The authors declare that this manuscript had not been published or under consideration for publication elsewhere, in whole or in part.
Rights and permissions
About this article
Cite this article
Zhao, Y., Lu, J., Zhang, Q. et al. Time Course of Neoangiogenesis After Indirect Bypass Surgery for Moyamoya Disease. Clin Neuroradiol 30, 91–99 (2020). https://doi.org/10.1007/s00062-018-0748-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-018-0748-3