Abstract
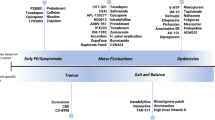
Parkinson’s disease is a chronic, neurodegenerative disease, which manifests with a mixture of motor, cognitive and behavioural symptoms. Levodopa is the most effective antiparkinsonian treatment to date, although chronic use engenders a mixture of complications in a substantial proportion of patients. Amongst these is the occurrence of episodes of worsening symptoms—‘off’ phenomena. These episodes can manifest with either motor or non-motor symptoms or a combination of these features and have been found to have profound impacts on patients’ quality of life. Although preventative measures are poorly evidenced, avoiding excessive total daily levodopa intake in selected populations that are deemed to be of a higher risk for develo** these episodes warrants further exploration. Methods to improve levodopa bioavailability and delivery to the brain are currently available and are of value in addressing these episodes once they have become established. These include modifications to levodopa formulations as well as the use of complimentary agents that improve levodopa bioavailability. The deployment of device-assisted approaches is a further dimension that can be considered in addressing these debilitating episodes. This review summarises the clinical manifestations of ‘off’ phenomena and the current approaches to treat them. Although we briefly discuss clinical advances on the horizon, the predominant focus is on existing, established treatments.




Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Mayeux R, et al. The frequency of idiopathic Parkinson’s disease by age, ethnic group, and sex in northern Manhattan, 1988–1993. Am J Epidemiol. 1996;143(5):528 (Am. J. Epidemiol: 1995).
Hughes AJ, Daniel SE, Blankson S, Lees AJ. A clinicopathologic study of 100 cases of parkinson’s disease. Arch Neurol. 1993;50(2):140–8.
Poewe W. Non-motor symptoms in Parkinson’s disease. Eur J Neurol. 2008. https://doi.org/10.1111/j.1468-1331.2008.02056.x.
Poewe W, et al. Parkinson disease. Nat Rev Dis Prim. 2017. https://doi.org/10.1038/nrdp.2017.13.
Cotzias GC, Papavasiliou PS, Gellene R. Modification of Parkinsonism—chronic treatment with L-dopa. N Engl J Med. 1969. https://doi.org/10.1056/NEJM196902132800701.
Cotzias GC, Van Woert MH, Schiffer LM. “Aromatic amino acids and modification of parkinsonism. N Engl J Med. 1967. https://doi.org/10.1056/NEJM196702162760703.
Fahn S. The history of dopamine and levodopa in the treatment of Parkinson’s disease. Mov Disord. 2008. https://doi.org/10.1002/mds.22028.
Obeso JA, Rodriguez-Oroz MC, Chana P, Lera G, Rodriguez M, Olanow CW. The evolution and origin of motor complications in Parkinson’s disease. Neurology. 2000;55(11 Suppl 4):S13–20.
Jankovic J. Motor fluctuations and dyskinesias in Parkinson’s disease: clinical manifestations. Mov Disord. 2005. https://doi.org/10.1002/mds.20458.
Martinez-Martin P, et al. Prevalence of nonmotor symptoms in Parkinson’s disease in an international setting; study using nonmotor symptoms questionnaire in 545 patients. Mov Disord. 2007. https://doi.org/10.1002/mds.21586.
Shulman LM, Taback RL, Bean J, Weiner WJ. Comorbity of the nonmotor symptoms of Parkinson’s disease. Mov Disord. 2001. https://doi.org/10.1002/mds.1099.
Marsden CD, Parkes JD. Success and problems of long-term levodopa therapy in Parkinson’s disease. Lancet. 1977. https://doi.org/10.1016/S0140-6736(77)91146-1.
Merello M, Lees AJ. Beginning-of-dose motor deterioration following the acute administration of levodopa and apomorphine in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1992. https://doi.org/10.1136/jnnp.55.11.1024.
Melamed E, Bitton V, Zelig O. Delayed onset of responses to single doses of L-Dopa in Parkinsonian fluctuators on long-term L-Dopa therapy. Clin Neuropharmacol. 1986. https://doi.org/10.1097/00002826-198604000-00009.
Witjas T, et al. Nonmotor fluctuations in Parkinson’s disease: frequent and disabling. Neurology. 2002. https://doi.org/10.1212/WNL.59.3.408.
Stacy M. The wearing-off phenomenon and the use of questionnaires to facilitate its recognition in Parkinson’s disease. J Neural Transm. 2010. https://doi.org/10.1007/s00702-010-0424-5.
Chaudhuri KR, et al. The nondeclaration of nonmotor symptoms of Parkinson’s disease to health care professionals: an international study using the nonmotor symptoms questionnaire. Mov Disord. 2010. https://doi.org/10.1002/mds.22868.
Martínez-Fernández R, Schmitt E, Martinez-Martin P, Krack P. The hidden sister of motor fluctuations in Parkinson’s disease: a review on nonmotor fluctuations. Mov Disord. 2016. https://doi.org/10.1002/mds.26731.
Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord. 2001. https://doi.org/10.1002/mds.1090.
Katzenschlager R, Head J, Schrag A, Ben-Shlomo Y, Evans A, Lees AJ. Fourteen-year final report of the randomized PDRG-UK trial comparing three initial treatments in PD. Neurology. 2008. https://doi.org/10.1212/01.wnl.0000310812.43352.66.
Hauser RA, et al. Ten-year follow-up of Parkinson’s disease patients randomized to initial therapy with ropinirole or levodopa. Mov Disord. 2007. https://doi.org/10.1002/mds.21743.
Hely MA, Reid WGJ, Adena MA, Halliday GM, Morris JGL. The Sydney Multicenter Study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord. 2008. https://doi.org/10.1002/mds.21956.
Rizos A, et al. Characterizing motor and non-motor aspects of early-morning off periods in Parkinson’s disease: an international multicenter study. Parkinsonism Relat Disord. 2014. https://doi.org/10.1016/j.parkreldis.2014.09.013.
Merims D, Djaldetti R, Melamed E. Waiting for ON: a major problem in patients with Parkinson disease and ON/OFF motor fluctuations. Clin Neuropharmacol. 2003. https://doi.org/10.1097/00002826-200307000-00009.
Hauser RA, et al. Sublingual apomorphine (APL-130277) for the acute conversion of OFF to ON in Parkinson’s disease. Mov Disord. 2016. https://doi.org/10.1002/mds.26697.
Van Lunen B, Anthony J, Spears J. Implications of motor fluctuations in Parkinson’s disease patients on chronic therapy (IMPACT): results from an observational registry. Mov Disord. 2005;20:S146.
Storch A, et al. Nonmotor fluctuations in Parkinson disease: severity and correlation with motor complications. Neurology. 2013. https://doi.org/10.1212/WNL.0b013e318285c0ed.
Brown RG, et al. Depression and anxiety related subtypes in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2011. https://doi.org/10.1136/jnnp.2010.213652.
Marras C, Chaudhuri KR. Nonmotor features of Parkinson’s disease subtypes. Mov Disord. 2016. https://doi.org/10.1002/mds.26510.
Chaudhuri KR, Poewe W, Brooks D. Motor and nonmotor complications of levodopa: phenomenology, risk factors, and imaging features. Mov Disord. 2018. https://doi.org/10.1002/mds.27386.
Hillen ME, Sage JI. Nonmotor fluctuations in patients with Parkinson’s disease. Neurology. 1996. https://doi.org/10.1212/WNL.47.5.1180.
Picillo M, et al. Gender and non motor fluctuations in Parkinson’s disease: a prospective study. Parkinsonism Relat Disord. 2016. https://doi.org/10.1016/j.parkreldis.2016.04.001.
Fahn S, et al. Levodopa and the progression of Parkinson’s disease. N Engl J Med. 2004. https://doi.org/10.1056/NEJMoa033447.
Stocchi F, Rascol O, Kieburtz K, Poewe W, Jankovic J, et al. Initiating levodopa/carbidopa therapy with and without entacapone in early Parkinson disease: the STRIDE-PD study. Ann Neurol. 2010;68(1):18–27.
Olanow CW, et al. Factors predictive of the development of Levodopa-induced dyskinesia and wearing-off in Parkinson’s disease. Mov Disord. 2013. https://doi.org/10.1002/mds.25364.
Schrag A, Quinn N. Dyskinesias and motor fluctuations in Parkinson’s disease: a community-based study. Brain. 2000. https://doi.org/10.1093/brain/123.11.2297.
Foltynie T, et al. BDNF val66met influences time to onset of levodopa induced dyskinesia in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2009. https://doi.org/10.1136/jnnp.2008.154294.
De Lau LML, Verbaan D, Marinus J, Heutink P, Van Hilten JJ. Catechol-O-methyltransferase Val158Met and the risk of dyskinesias in Parkinson’s disease. Mov Disord. 2012. https://doi.org/10.1002/mds.23805.
Lee JY, Cho J, Lee EK, Park SS, Jeon BS. Differential genetic susceptibility in diphasic and peak-dose dyskinesias in Parkinson’s disease. Mov Disord. 2011. https://doi.org/10.1002/mds.23400.
Schumacher-Schuh AF, et al. Association of common genetic variants of HOMER1 gene with levodopa adverse effects in Parkinson’s disease patients. Pharmacogenom J. 2014. https://doi.org/10.1038/tpj.2013.37.
Politis M, Wu K, Molloy S, Bain PG, Chaudhuri KR, Piccini P. Parkinson’s disease symptoms: the patient’s perspective. Mov Disord. 2010. https://doi.org/10.1002/mds.23135.
Chapuis S, Ouchchane L, Metz O, Gerbaud L, Durif F. Impact of the motor complications of Parkinson’s disease on the quality of life. Mov Disord. 2005. https://doi.org/10.1002/mds.20279.
Hung SW, Adeli GM, Arenovich T, Fox SH, Lang AE. Patient perception of dyskinesia in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2010. https://doi.org/10.1136/jnnp.2009.173286.
Storch A, et al. Quantitative assessment of non-motor fluctuations in Parkinson’s disease using the Non-Motor Symptoms Scale (NMSS). J Neural Transm. 2015. https://doi.org/10.1007/s00702-015-1437-x.
Nutt JG, Woodward WR, Carter JH, Gancher ST. Effect of long-term therapy on the pharmacodynamics of levodopa: relation to on-off phenomenon. Arch Neurol. 1992. https://doi.org/10.1001/archneur.1992.00530350037016.
Nutt JG, Holford NHG. The response to levodopa in Parkinson’s disease: imposing pharmacological law and order. Ann Neurol. 1996. https://doi.org/10.1002/ana.410390504.
Nutt JG, Carter JH, Lea ES, Sexton GJ. Evolution of the response to levodopa during the first 4 years of therapy. Ann Neurol. 2002. https://doi.org/10.1002/ana.10189.
Zappia M, et al. Loss of long-duration response to levodopa over time in PD: implications for wearing-off. Neurology. 1999. https://doi.org/10.1212/wnl.52.4.763.
Stocchi F. The hypothesis of the genesis of motor complications and continuous dopaminergic stimulation in the treatment of Parkinson’s disease. Parkinsonism Relat Disord. 2009. https://doi.org/10.1016/S1353-8020(09)70005-7.
Nutt JG, Woodward WR, Hammerstad JP, Carter JH, Anderson JL. The On–Off phenomenon in Parkinson’s disease: relation to levodopa absorption and transport. N Engl J Med. 1984. https://doi.org/10.1056/NEJM198402233100802.
Edwards LL, Quigley EMM, Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease: frequency and pathophysiology. Neurology. 1992. https://doi.org/10.1212/wnl.42.4.726.
Baruzzi A, et al. Infuence of meal ingestion time on pharmacokinetics of orally administered levodopa in parkinsonian patients. Clin Neuropharmacol. 1987. https://doi.org/10.1097/00002826-198712000-00004.
Leon AS, Spiegel HE. The effect of antacid administration on the absorption and metabolism of levodopa. J Clin Pharmacol New Drugs. 1972. https://doi.org/10.1002/j.1552-4604.1972.tb00053.x.
Valenzuela JE. Dopamine as a possible neurotransmitter in gastric relaxation. Gastroenterology. 1976. https://doi.org/10.1016/S0016-5085(76)80051-0.
Frackowiak RS, Leenders KL, Poewe WH, Palmer AJ, Brenton DP. Inhibition of L-18Ffluorodopa uptake into human brain by amino acids demonstrated by positron emission tomography. Ann Neurol. 1986;20(2):258–62.
Çamcı G, Oğuz S. Association between Parkinson’s disease and Helicobacter pylori. J Clin Neurol (Korea). 2016. https://doi.org/10.3988/jcn.2016.12.2.147.
van Kessel SP, El Aidy S. Contributions of gut bacteria and diet to drug pharmacokinetics in the treatment of Parkinson’s disease. Front Neurol. 2019. https://doi.org/10.3389/fneur.2019.01087.
Fabbnni G, Mouradian MM, Junecos JL, Schlegel J, Mohr E, Chase TN. Motor fluctuations in Parkinson’s disease: central pathophysiological mechanisms, Part I. Ann Neurol. 1988. https://doi.org/10.1002/ana.410240303.
Mouradian MM, Junecos JL, Fabbrini G, Schlegel J, Bartko JJ, Chase TN. Motor fluctuations in Parkinson’s disease: central pathophysiological mechanisms, part II. Ann Neurol. 1988. https://doi.org/10.1002/ana.410240304.
Bravi D, Mouradian MM, Roberts JW, Davis TL, Sohn YH, Chase TN. Wearing-off fluctuations in Parkinson’s disease: contribution of postsynaptic mechanisms. Ann Neurol. 1994. https://doi.org/10.1002/ana.410360108.
Barbato L, et al. The long-duration action of levodopa may be due to a postsynaptic effect. Clin Neuropharmacol. 1997. https://doi.org/10.1097/00002826-199710000-00003.
Stocchi F, Vacca L, Berardelli A, De Pandis F, Ruggieri S. Long-duration effect and the postsynaptic compartment: study using a dopamine agonist a short half-life. Mov Disord. 2001. https://doi.org/10.1002/mds.1070.
Bergstrom BP, Garris PA. ‘Passive stabilization’ of striatal extracellular dopamine across the lesion spectrum encompassing the presymptomatic phase of Parkinson’s disease: a voltammetric study in the 6-OHDA-lesioned rat. J Neurochem. 2003. https://doi.org/10.1046/j.1471-4159.2003.02104.x.
Abercrombie ED, Bonatz AE, Zigmond MJ. Effects of l-DOPA on extracellular dopamine in striatum of normal and 6-hydroxydopamine-treated rats. Brain Res. 1990. https://doi.org/10.1016/0006-8993(90)91318-B.
Chase TN, Baronti F, Fabbrini G, Heuser IJ, Juncos JL, Mouradian MM. Rationale for continuous dopaminomimetic therapy of Parkinson’s disease. Neurology. 1989;39(11 Suppl 2):7–10.
De La Fuente-Fernndez R, et al. Biochemical variations in the synaptic level of dopamine precede motor fluctuations in Parkinson’s disease: PET evidence of increased dopamine turnover. Ann Neurol. 2001. https://doi.org/10.1002/ana.65.
Obeso JA, et al. The origin of motor fluctuations in Parkinson’s disease: importance of dopaminergic innervation and basal ganglia circuits. Neurology. 2004. https://doi.org/10.1212/wnl.62.1_suppl_1.s17.
Chaudhuri KR, Rizos A, Sethi KD. Motor and nonmotor complications in Parkinson’s disease: an argument for continuous drug delivery? J Neural Transm. 2013. https://doi.org/10.1007/s00702-013-0981-5.
Brown P, Marsden CD. What do the basal ganglia do? Lancet. 1998. https://doi.org/10.1016/S0140-6736(97)11225-9.
Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson’s disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain. 2005. https://doi.org/10.1093/brain/awh445.
Halliday GM, Leverenz JB, Schneider JS, Adler CH. The neurobiological basis of cognitive impairment in Parkinson’s disease. Mov Disord. 2014. https://doi.org/10.1002/mds.25857.
Lim SY, Fox SH, Lang AE. Overview of the extranigral aspects of Parkinson disease. Arch Neurol. 2009. https://doi.org/10.1001/archneurol.2008.561.
Verschuur CVM, et al. Randomized delayed-start trial of levodopa in Parkinson’s disease. N Engl J Med. 2019. https://doi.org/10.1056/NEJMoa1809983.
Hsu A, Yao HM, Gupta S, Modi NB. Comparison of the pharmacokinetics of an oral extended-release capsule formulation of carbidopa-levodopa (IPX066) with immediate-release carbidopa-levodopa (Sinemet®), sustained-release carbidopa-levodopa (Sinemet® CR), and carbidopa–levodopa–entacapone (Stalevo®). J Clin Pharmacol. 2015. https://doi.org/10.1002/jcph.514.
Goetze O, Wieczorek J, Mueller T, Przuntek H, Schmidt WE, Woitalla D. Impaired gastric emptying of a solid test meal in patients with Parkinson’s disease using 13C-sodium octanoate breath test. Neurosci Lett. 2005. https://doi.org/10.1016/j.neulet.2004.11.007.
Destée A, Rérat K, Bourdeix I. Is there a difference between levodopa/dopa-decarboxylase inhibitor and entacapone and levodopa/dopa-decarboxylase inhibitor dose fractionation strategies in Parkinson’s disease patients experiencing symptom re-emergence due to wearing-off? The honeymoon study. Eur Neurol. 2009. https://doi.org/10.1159/000177938.
Carter JH, Nutt JG, Woodward WR, Hatcher LF, Trotman TL. Amount and distribution of dietary protein affects clinical response to levodopa in Parkinson’s disease. Neurology. 1989. https://doi.org/10.1212/wnl.39.4.552.
Cereda E, Barichella M, Pedrolli C, Pezzoli G. Low-protein and protein-redistribution diets for Parkinson’s disease patients with motor fluctuations: a systematic review. Mov Disord. 2010. https://doi.org/10.1002/mds.23226.
Burn DJ, et al. Decreased ‘OFF’ time and improved Parkinson’s disease symptoms with the gastroprokinetic camicinal as an adjunct to L-DOPA based treatment; a pilot study. Mov Disord. 2015. https://doi.org/10.1002/mds.26295.
Cotzias GC, Papavasiliou PS, Gellene R. Experimental treatment of parkinsonism with L-Dopa. Neurology. 1968;18(3):276–7.
LeWitt PA, et al. Pharmacokinetic–pharmacodynamic crossover comparison of two levodopa extension strategies. Mov Disord. 2009. https://doi.org/10.1002/mds.22587.
Dupont E, et al. Sustained-release Madopar HBS® compared with standard Madopar® in the long-term treatment of de novo parkinsonian patients. Acta Neurol Scand. 2009. https://doi.org/10.1111/j.1600-0404.1996.tb00163.x.
Block G, Liss C, Reines S, Irr J, Nibbelink D. Comparison of immediate-release and controlled release carbidopa/levodopa in Parkinson’s disease. A multicenter 5-year study. The CR First Study Group. Eur Neurol. 1997;37(1):23–7.
Mittur A, Gupta S, Modi NB. Pharmacokinetics of Rytary®, an extended-release capsule formulation of carbidopa–levodopa. Clin Pharmacokinet. 2017. https://doi.org/10.1007/s40262-017-0511-y.
Yao HM, Hsu A, Gupta S, Modi NB. Clinical pharmacokinetics of IPX066: evaluation of dose proportionality and effect of food in healthy volunteers. Clin Neuropharmacol. 2016. https://doi.org/10.1097/WNF.0000000000000126.
Morgan JC, Dhall R, Rubens R, Khanna S, Gupta S. Dosing patterns during conversion to IPX066, extended-release carbidopa–levodopa (ER CD-LD), in Parkinson’s disease with motor fluctuations. Parkinsons Dis. 2018. https://doi.org/10.1155/2018/9763057.
Hauser RA, et al. Extended-release carbidopa–levodopa (IPX066) compared with immediate-release carbidopa-levodopa in patients with Parkinson’s disease and motor fluctuations: a phase 3 randomised, double-blind trial. Lancet Neurol. 2013. https://doi.org/10.1016/S1474-4422(13)70025-5.
Pahwa R, et al. Randomized trial of IPX066, carbidopa/levodopa extended release, inearly Parkinson’s disease. Parkinsonism Relat Disord. 2014. https://doi.org/10.1016/j.parkreldis.2013.08.017.
Metman LV, Stover N, Chen C, Cowles VE, Sweeney M. Gastroretentive carbidopa/levodopa, DM-1992, for the treatment of advanced Parkinson’s disease. Mov Disord. 2015. https://doi.org/10.1002/mds.26219.
LeWitt PA. New levodopa therapeutic strategies. Parkinsonism Relat Disord. 2016. https://doi.org/10.1016/j.parkreldis.2015.09.021.
LeWitt PA, et al. Accordion pill carbidopa/levodopa (AP-CD/LD) for treatment of advanced PD. Mov Disord. 2014. https://doi.org/10.1002/mds.25914.
Navon N, Gendreau R, Meckler J. Gastric retention of the accordion Pill™: results from MRI studies with Parkinson’s disease patients and healthy volunteers [abstract]. Mov Disord. 2018;33(suppl 2).
LeWitt PA, Giladi N, Navon N. Pharmacokinetics and efficacy of a novel formulation of carbidopa-levodopa (Accordion Pill®) in Parkinson’s disease. Parkinsonism Relat Disord. 2019. https://doi.org/10.1016/j.parkreldis.2019.05.032.
LeWitt P, Gendreau R, Meckler J, Navon N. Design of a phase 3 efficacy and safety trial of accordion Pill™ carbidopa/levodopa for Parkinson’s disease (PD) patients experiencing motor fluctuations [abstract]. Mov Disord. 2018;33(suppl 2).
Kuoppamäki M, Leinonen M, Poewe W. Efficacy and safety of entacapone in levodopa/carbidopa versus levodopa/benserazide treated Parkinson’s disease patients with wearing-off. J Neural Transm. 2015. https://doi.org/10.1007/s00702-015-1449-6.
Rinne UK, Larsen JP, Siden Å, Worm-Petersen J. Entacapone enhances the response to levodopa in parkinsonian patients with motor fluctuations. Neurology. 1998. https://doi.org/10.1212/WNL.51.5.1309.
Poewe WH, Deuschl G, Gordin A, Kultalahti ER, Leinonen M. Efficacy and safety of entacapone in Parkinson’s disease patients with suboptimal levodopa response: a 6-month randomized placebo controlled double blind study in Germany and Austria (Celomen study). Acta Neurol Scand. 2002. https://doi.org/10.1034/j.1600-0404.2002.1o174.x.
Brooks DJ, Sagar H. Entacapone is beneficial in both fluctuating and non-fluctuating patients with Parkinson’s disease: a randomised, placebo controlled, double blind, six month study. J Neurol Neurosurg Psychiatry. 2003. https://doi.org/10.1136/jnnp.74.8.1071.
Ceravolo R, Piccini P, Bailey DL, Jorga KM, Bryson H, Brooks DJ. 18F-dopa PET evidence that tolcapone acts as a central COMT inhibitor in Parkinson’s disease. Synapse. 2002. https://doi.org/10.1002/syn.10034.
Adler CH, et al. Randomized, placebo-controlled study of tolcapone in patients with fluctuating Parkinson disease treated with levodopa–carbidopa. Arch Neurol. 1998. https://doi.org/10.1001/archneur.55.8.1089.
Assal F, Spahr L, Hadengue A, Rubbici-Brandt L, Burkhard PR. Tolcapone and fulminant hepatitis. Lancet. 1998. https://doi.org/10.1016/S0140-6736(05)61511-5.
Ferreira JJ, et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson’s disease. Eur J Neurol. 2013. https://doi.org/10.1111/j.1468-1331.2012.03866.x.
Ferreira JJ, et al. Effect of opicapone on levodopa pharmacokinetics, catechol-O-methyltransferase activity and motor fluctuations in patients with Parkinson’s disease. Eur J Neurol. 2015. https://doi.org/10.1111/ene.12666.
Rocha JF, et al. Effect of opicapone and entacapone upon levodopa pharmacokinetics during three daily levodopa administrations. Eur J Clin Pharmacol. 2014. https://doi.org/10.1007/s00228-014-1701-2.
Lees AJ, et al. Opicapone as adjunct to levodopa therapy in patients with Parkinson disease and motor fluctuations a randomized clinical trial. JAMA Neurol. 2017. https://doi.org/10.1001/jamaneurol.2016.4703.
Ferreira JJ, Lees A, Rocha JF, Poewe W, Rascol O, Soares-da-Silva P. Opicapone as an adjunct to levodopa in patients with Parkinson’s disease and end-of-dose motor fluctuations: a randomised, double-blind, controlled trial. Lancet Neurol. 2016. https://doi.org/10.1016/S1474-4422(15)00336-1.
Elmer LW. Rasagiline adjunct therapy in patients with Parkinson’s disease: Posthoc analyses of the PRESTO and LARGO trials. Parkinsonism Relat Disord. 2013. https://doi.org/10.1016/j.parkreldis.2013.06.001.
Schwid SR. A randomized placebo-controlled trial of rasagiline in levodopa-treated patients with Parkinson disease and motor fluctuations: the PRESTO study. Arch Neurol. 2005. https://doi.org/10.1001/archneur.62.2.241.
Rascol O, et al. Rasagiline as an adjunct to levodopa in patients with Parkinson’s disease and motor fluctuations (LARGO, Lasting effect in Adjunct therapy with Rasagiline Given Once daily, study): a randomised, double-blind, parallel-group trial. Lancet. 2005. https://doi.org/10.1016/S0140-6736(05)71083-7.
Fox SH, et al. International Parkinson and movement disorder society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2018. https://doi.org/10.1002/mds.27372.
Heinonen EH, Myllylä V. Safety of selegiline (Deprenyl) in the treatment of Parkinson’s disease. Drug Saf. 1998. https://doi.org/10.2165/00002018-199819010-00002.
Richard IH, Kurlan R, Tanner C, Factor S, Hubble J, Suchowersky O, Waters C. Serotonin syndrome and the combined use of deprenyl and an antidepressant in Parkinson's disease. Neurology. 1997;48(4):1070–7.
Panisset M, Chen JJ, Rhyee SH, Conner J, Mathena J. Serotonin toxicity association with concomitant antidepressants and rasagiline treatment: retrospective study (STACCATO). Pharmacotherapy. 2014. https://doi.org/10.1002/phar.1500.
Caccia C, et al. Safinamide: From molecular targets to a new anti-Parkinson drug. Neurology. 2006. https://doi.org/10.1212/wnl.67.7_suppl_2.s18.
Borgohain R, et al. Randomized trial of safinamide add-on to levodopa in Parkinson’s disease with motor fluctuations. Mov Disord. 2014. https://doi.org/10.1002/mds.25751.
Schapira AHV, et al. Assessment of safety and efficacy of safinamide as a levodopa adjunct in patients with Parkinson disease and motor fluctuations a randomized clinical trial. JAMA Neurol. 2017. https://doi.org/10.1001/jamaneurol.2016.4467.
Borgohain R, et al. Two-year, randomized, controlled study of safinamide as add-on to levodopa in mid to late Parkinson’s disease. Mov Disord. 2014. https://doi.org/10.1002/mds.25961.
Binde CD, Tvete IF, Gåsemyr J, Natvig B, Klemp M. A multiple treatment comparison meta-analysis of monoamine oxidase type B inhibitors for Parkinson’s disease. Br J Clin Pharmacol. 2018. https://doi.org/10.1111/bcp.13651.
Kvernmo T, Härtter S, Burger E. A review of the receptor-binding and pharmacokinetic properties of dopamine agonists. Clin Ther. 2006. https://doi.org/10.1016/j.clinthera.2006.08.004.
Jenner P. Pharmacology of dopamine agonists in the treatment of Parkinson’s disease. Neurology. 2002. https://doi.org/10.1212/wnl.58.suppl_1.s1.
Piercey MF. Pharmacology of pramipexole, a dopamine D3-preferring agonist useful in treating Parkinson’s disease. Clin Neuropharmacol. 1998;21(3):141–51.
Hoehn MMM, Elton RL. Low dosages of bromocriptine added to levodopa in Parkinson’s disease. Neurology. 1985. https://doi.org/10.1212/wnl.35.2.199.
Stocchi F, et al. Ropinirole 24-hour prolonged release and ropinirole immediate release in early Parkinson’s disease: a randomized, double-blind, non-inferiority crossover study. Curr Med Res Opin. 2008. https://doi.org/10.1185/03007990802387130.
Pahwa R, et al. Ropinirole 24-hour prolonged release: randomized, controlled study in advanced Parkinson disease. Neurology. 2007. https://doi.org/10.1212/01.wnl.0000258660.74391.c1.
Poewe W, et al. Extended-release pramipexole in early Parkinson disease A 33-week randomized controlled trial. Neurology. 2011. https://doi.org/10.1212/WNL.0b013e31822affb0.
Schapira AHV, et al. Extended-release pramipexole in advanced Parkinson disease: a randomized controlled trial. Neurology. 2011. https://doi.org/10.1212/WNL.0b013e31822affdb.
Elshoff JP, Cawello W, Andreas JO, Mathy FX, Braun M. An update on pharmacological, pharmacokinetic properties and drug-drug interactions of rotigotine transdermal system in Parkinson’s disease and restless legs syndrome. Drugs. 2015. https://doi.org/10.1007/s40265-015-0377-y.
Trenkwalder C, et al. Rotigotine effects on early morning motor function and sleep in Parkinson’s disease: a double-blind, randomized, placebo-controlled study (RECOVER). Mov Disord. 2011. https://doi.org/10.1002/mds.23441.
Kassubek J, et al. Rotigotine transdermal system and evaluation of pain in patients with Parkinson’s disease: a post hoc analysis of the RECOVER study. BMC Neurol. 2014. https://doi.org/10.1186/1471-2377-14-42.
Hirano M, Isono C, Sakamoto H, Ueno S, Kusunoki S, Nakamura Y. Rotigotine transdermal patch improves swallowing in dysphagic patients with Parkinson’s disease. Dysphagia. 2015. https://doi.org/10.1007/s00455-015-9622-5.
Tateno H, et al. Transdermal dopamine agonist ameliorates gastric emptying in Parkinson’s disease. J Am Geriatr Soc. 2015. https://doi.org/10.1111/jgs.13800.
Lee JY, et al. Association between the dose of dopaminergic medication and the behavioral disturbances in Parkinson disease. Parkinsonism Relat Disord. 2010. https://doi.org/10.1016/j.parkreldis.2009.12.002.
Rabinak CA, Nirenberg MJ. Dopamine agonist withdrawal syndrome in parkinson disease. Arch Neurol. 2010. https://doi.org/10.1001/archneurol.2009.294.
Nirenberg MJ. Dopamine agonist withdrawal syndrome: implications for patient care. Drugs Aging. 2013. https://doi.org/10.1007/s40266-013-0090-z.
Antonini A, Poewe W. Fibrotic heart-valve reactions to dopamine-agonist treatment in Parkinson’s disease. Lancet Neurol. 2007. https://doi.org/10.1016/S1474-4422(07)70218-1.
Rizos A, et al. A European multicentre survey of impulse control behaviours in Parkinson’s disease patients treated with short- and long-acting dopamine agonists. Eur J Neurol. 2016. https://doi.org/10.1111/ene.13034.
Garcia-Ruiz PJ, et al. Impulse control disorder in patients with Parkinson’s disease under dopamine agonist therapy: a multicentre study. J Neurol Neurosurg Psychiatry. 2014. https://doi.org/10.1136/jnnp-2013-306787.
Shulman LM, Minagar A, Rabinstein A, Weiner WJ. The use of dopamine agonists in very elderly patients with Parkinson’s disease. Mov Disord. 2000. https://doi.org/10.1002/1531-8257(200007)15:4%3c664:AID-MDS1010%3e3.0.CO;2-D.
Saint-Cyr JA, Trépanier LL. Beneficial effects of amantodine on L-dopa-induced dyskinesias in Parkinson’s disease. Mov Disord. 2000. https://doi.org/10.1002/1531-8257(200009)15:5%3c873:AID-MDS1017%3e3.0.CO;2-I.
Metman LV, Del Dotto P, Van Den Munckhof P, Fang J, Mouradian MM, Chase TN. Amantadine as treatment for dyskinesias and motor fluctuations in Parkinson’s disease. Neurology. 1998. https://doi.org/10.1212/wnl.50.5.1323.
Malkani R, Zadikoff C, Melen O, Videnovic A, Borushko E, Simuni T. Amantadine for freezing of gait in patients with parkinson disease. Clin Neuropharmacol. 2012. https://doi.org/10.1097/WNF.0b013e31826e3406.
Thomas A, Iacono D, Luciano AL, Armellino K, Di Iorio A, Onofrj M. Duration of amantadine benefit on dyskinesia of severe Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2004;75(1):141–3.
Ory-Magne F, et al. Withdrawing amantadine in dyskinetic patients with Parkinson disease: the AMANDYSK trial. Neurology. 2014. https://doi.org/10.1212/WNL.0000000000000050.
Hauser RA, et al. Pharmacokinetics of ADS-5102 (Amantadine) extended release capsules administered once daily at bedtime for the treatment of dyskinesia. Clin Pharmacokinet. 2019. https://doi.org/10.1007/s40262-018-0663-4.
Pahwa R, et al. ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson disease (EASE LID study): a randomized clinical trial. JAMA Neurol. 2017. https://doi.org/10.1001/jamaneurol.2017.0943.
Oertel W, et al. Randomized, placebo-controlled trial of ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson’s disease (EASE LID 3). Mov Disord. 2017. https://doi.org/10.1002/mds.27131.
Pahwa R, et al. Amantadine extended release for levodopa-induced dyskinesia in Parkinson’s disease (EASED Study). Mov Disord. 2015. https://doi.org/10.1002/mds.26159.
Kase H. Industry forum: progress in pursuit of therapeutic A2A antagonists—the adenosine A2A receptor selective antagonist KW6002: research and development toward a novel nondopaminergic therapy for Parkinson’s disease. Neurology. 2003. https://doi.org/10.1212/01.wnl.0000095219.22086.31.
Hauser RA, et al. Study of istradefylline in patients with Parkinson’s disease on levodopa with motor fluctuations. Mov Disord. 2008. https://doi.org/10.1002/mds.22095.
Mizuno Y, Kondo T. Adenosine A2A receptor antagonist istradefylline reduces daily OFF time in Parkinson’s disease. Mov Disord. 2013. https://doi.org/10.1002/mds.25418.
Takahashi M, Fujita M, Asai N, Saki M, Mori A. Safety and effectiveness of istradefylline in patients with Parkinson’s disease: interim analysis of a post-marketing surveillance study in Japan. Expert Opin Pharmacother. 2018. https://doi.org/10.1080/14656566.2018.1518433.
Kondo T, Mizuno Y. A long-term study of istradefylline safety and efficacy in patients with parkinson disease. Clin Neuropharmacol. 2015. https://doi.org/10.1097/WNF.0000000000000073.
Murata M, et al. Zonisamide improves wearing-off in Parkinson’s disease: a randomized, double-blind study. Mov Disord. 2015. https://doi.org/10.1002/mds.26286.
Fornadi F, Milani F, Werner M. Madopar dispersible in the treatment of advanced Parkinson’s disease. Clin Neuropharmacol. 1995. https://doi.org/10.1097/00002826-199417003-00003.
Jansson Y, Eriksson B, Johnels B. Dispersible levodopa has a fast and more reproducible onset of action than the conventional preparation in Parkinson’s disease. A study with optoelectronic movement analysis. Parkinsonism Relat Disord. 1998. https://doi.org/10.1016/s1353-8020(98)00036-4.
Auffret M, Drapier S, Vérin M. Pharmacological insights into the use of apomorphine in Parkinson’s disease: clinical relevance. Clin Drug Investig. 2018. https://doi.org/10.1007/s40261-018-0619-3.
Millan MJ, Maiofiss L, Cussac D, Audinot V, Boutin JA, Newman-Tancredi A. Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes. J Pharmacol Exp Ther. 2002. https://doi.org/10.1124/jpet.102.039867.
Jenner P, Katzenschlager R. Apomorphine—pharmacological properties and clinical trials in Parkinson’s disease. Parkinsonism Relat Disord. 2016. https://doi.org/10.1016/j.parkreldis.2016.12.003.
Gancher ST, Nutt JG, Woodward WR. Absorption of apomorphine by various routes in parkinsonism. Mov Disord. 1991. https://doi.org/10.1002/mds.870060304.
Nicolle E, et al. Pharmacokinetics of apomorphine in parkinsonian patients. Fundam Clin Pharmacol. 1993. https://doi.org/10.1111/j.1472-8206.1993.tb00238.x.
Gancher ST, Woodward WR, Boucher B, Nutt JG. Peripheral pharmacokinetics of apomorphine in humans. Ann Neurol. 1989. https://doi.org/10.1002/ana.410260209.
Corboy DL, Wagner ML, Sage JI. Apomorphine for motor fluctuations and freezing in Parkinson’s disease. Ann Pharmacother. 1995. https://doi.org/10.1177/106002809502900310.
LeWitt PA. Subcutaneously administered apomorphine: pharmacokinetics and metabolism. Neurology. 2004. https://doi.org/10.1212/wnl.62.6_suppl_4.s8.
Dewey RB, Hutton JT, LeWitt PA, Factor SA. A randomized, double-blind, placebo-controlled trial of subcutaneously injected apomorphine for parkinsonian off-state events. Arch Neurol. 2001. https://doi.org/10.1001/archneur.58.9.1385.
Gunzler SA, Koudelka C, Carlson NE, Pavel M, Nutt JG. Effect of low concentrations of apomorphine on parkinsonism in a randomized, placebo-controlled, crossover study. Arch Neurol. 2008. https://doi.org/10.1001/archneurol.2007.58.
Pahwa R, Koller WC, Trosch RM, Sherry JH. Subcutaneous apomorphine in patients with advanced Parkinson’s disease: a dose-escalation study with randomized, double-blind, placebo-controlled crossover evaluation of a single dose. J Neurol Sci. 2007. https://doi.org/10.1016/j.jns.2007.03.013.
Merello M, Pikielny R, Cammarota A, Leiguarda R. Comparison of subcutaneous apomorphine versus dispersible madopar latency and effect duration in Parkinson’s disease patients: a double-blind single-dose study. Clin Neuropharmacol. 1997. https://doi.org/10.1097/00002826-199704000-00008.
Isaacson S, Lew M, Ondo W, Hubble J, Clinch T, Pagan F. Apomorphine subcutaneous injection for the management of morning akinesia in Parkinson’s disease. Mov Disord Clin Pract. 2017. https://doi.org/10.1002/mdc3.12350.
Stibe CMH, Kempster PA, Lees AJ, Stern GM. Subcutaneous apomorphine in parkinsonian on–off oscillations. Lancet. 1988. https://doi.org/10.1016/S0140-6736(88)91193-2.
Stibe C, Lees A, Stern G. Subcutaneous infusion of apomorphine and lisuride in the treatment of parkinsonian on-off fluctuations. Lancet. 1987. https://doi.org/10.1016/S0140-6736(87)91660-6.
Frankel JP, Lees AJ, Kempster PA, Stern GM. Subcutaneous apomorphine in the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1990. https://doi.org/10.1136/jnnp.53.2.96.
LeWitt PA, Ondo WG, Van Lunen B, Bottini PB. Open-label study assessment of safety and adverse effects of subcutaneous apomorphine injections in treating ‘off’ episodes in advanced Parkinson disease. Clin Neuropharmacol. 2009. https://doi.org/10.1097/WNF.0b013e31816d91f9.
Lees A. Dopamine agonists in Parkinson’s disease: a look at apomorphine. Fundam Clin Pharmacol. 1993. https://doi.org/10.1111/j.1472-8206.1993.tb00226.x.
Martinez-Martin P, et al. Chronic subcutaneous infusion therapy with apomorphine in advanced Parkinson’s disease compared to conventional therapy: a real life study of non motor effect. J Parkinsons Dis. 2011. https://doi.org/10.3233/JPD-2011-11037.
Grosset KA, Malek N, Morgan F, Grosset DG. Phase IIa randomized double-blind, placebo-controlled study of inhaled apomorphine as acute challenge for rescuing ‘off’ periods in patients with established Parkinson’s disease. Eur J Neurol. 2013. https://doi.org/10.1111/ene.12091.
Grosset KA, Malek N, Morgan F, Grosset DG. Inhaled dry powder apomorphine (VR040) for ’off ’ periods in Parkinson’s disease: an in-clinic double-blind dose ranging study. Acta Neurol Scand. 2013. https://doi.org/10.1111/ane.12107.
Grosset KA, Malek N, Morgan F, Grosset DG. Inhaled apomorphine in patients with ‘on-off’ fluctuations: a randomized, double-blind, placebo-controlled, clinic and home based, parallel-group study. J Parkinsons Dis. 2013. https://doi.org/10.3233/JPD-120142.
Olanow CW, et al. Apomorphine sublingual film for off episodes in Parkinson’s disease: a randomised, double-blind, placebo-controlled phase 3 study. Lancet Neurol. 2020. https://doi.org/10.1016/S1474-4422(19)30396-5.
Tambasco N, Romoli M, Calabresi P. Levodopa in Parkinson’s disease: current status and future developments. Curr Neuropharmacol. 2017. https://doi.org/10.2174/1570159x15666170510143821.
Taddei RN, Spinnato F, Jenner P. New symptomatic treatments for the management of motor and nonmotor symptoms of Parkinson’s disease. Int Rev Neurobiol. 2017;132:407–52.
LeWitt PA, et al. A randomized trial of inhaled levodopa (CVT-301) for motor fluctuations in Parkinson’s disease. Mov Disord. 2016. https://doi.org/10.1002/mds.26611.
Grosset D, et al. Long-term pulmonary safety of inhaled levodopa in Parkinson’s disease subjects with motor fluctuations: interim results of a phase 3 study. Parkinsonism Relat Disord. 2018. https://doi.org/10.1016/j.parkreldis.2017.11.287.
Antonini A, et al. Develo** consensus among movement disorder specialists on clinical indicators for identification and management of advanced Parkinson’s disease: a multi-country Delphi-panel approach. Curr Med Res Opin. 2018. https://doi.org/10.1080/03007995.2018.1502165.
Bredberg E, et al. Intraduodenal infusion of a water-based levodopa dispersion for optimisation of the therapeutic effect in severe Parkinson’s disease. Eur J Clin Pharmacol. 1993. https://doi.org/10.1007/BF00315491.
Nyholm D, et al. Optimizing levodopa pharmacokinetics: intestinal infusion versus oral sustained-release tablets. Clin Neuropharmacol. 2003. https://doi.org/10.1097/00002826-200305000-00010.
Nyholm D, et al. Pharmacokinetics of levodopa, carbidopa, and 3-O-methyldopa following 16-hour jejunal infusion of levodopa-carbidopa intestinal gel in advanced Parkinson’s disease patients. AAPS J. 2013. https://doi.org/10.1208/s12248-012-9439-1.
Vijiaratnam N, et al. Levodopa–carbidopa intestinal gel: is the naso-jejunal phase a redundant convention? Intern Med J. 2018. https://doi.org/10.1111/imj.13754.
Zibetti M, et al. Sleep improvement with levodopa/carbidopa intestinal gel infusion in Parkinson disease. Acta Neurol Scand. 2013. https://doi.org/10.1111/ane.12075.
Chang FCF, et al. 24h Levodopa–carbidopa intestinal gel may reduce falls and ‘unresponsive’ freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord. 2015. https://doi.org/10.1016/j.parkreldis.2014.12.019.
Olanow CW, et al. Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson’s disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. 2014. https://doi.org/10.1016/S1474-4422(13)70293-X.
Standaert DG, et al. Effect of levodopa–carbidopa intestinal gel on non-motor symptoms in patients with advanced Parkinson’s disease. Mov Disord Clin Pract. 2017. https://doi.org/10.1002/mdc3.12526.
Fernandez HH, et al. Levodopa-carbidopa intestinal gel in advanced Parkinson’s disease: final 12-month, open-label results. Mov Disord. 2015. https://doi.org/10.1002/mds.26123.
Vijiaratnam N, Sue CM. Levodopa-carbidopa intestinal gel: ‘dismantling the road blocks of a journey’. Intern Med J. 2018. https://doi.org/10.1111/imj.13757.
Vijiaratnam N, Sue CM. How do i manage patients with the levodopa/carbidopa intestinal gel? Mov Disord Clin Pract. 2019. https://doi.org/10.1002/mdc3.12701.
Vijiaratnam N, Sue CM. Maximizing benefits of the levodopa/carbidopa intestinal gel: systematic considerations, challenging convention and individualizing approaches. Basal Ganglia. 2018. https://doi.org/10.1016/j.baga.2018.12.002.
Merola A, Romagnolo A, Zibetti M, Bernardini A, Cocito D, Lopiano L. Peripheral neuropathy associated with levodopa–carbidopa intestinal infusion: a long-term prospective assessment. Eur J Neurol. 2016. https://doi.org/10.1111/ene.12846.
Rispoli V, et al. Peripheral neuropathy in 30 duodopa patients with vitamins B supplementation. Acta Neurol Scand. 2017. https://doi.org/10.1111/ane.12783.
Rogers G, Davies D, Pink J, Cooper P. Parkinson’s disease: summary of updated NICE guidance. BMJ. 2017. https://doi.org/10.1136/bmj.j1951.
Bhidayasiri R, Sringean J, Anan C, Boonpang K, Thanawattano C, Chaudhuri KR. Quantitative demonstration of the efficacy of night-time apomorphine infusion to treat nocturnal hypokinesia in Parkinson’s disease using wearable sensors. Parkinsonism Relat Disord. 2016. https://doi.org/10.1016/j.parkreldis.2016.11.016.
Trenkwalder C, et al. Expert Consensus Group report on the use of apomorphine in the treatment of Parkinson’s disease—clinical practice recommendations. Parkinsonism Relat Disord. 2015. https://doi.org/10.1016/j.parkreldis.2015.06.012.
Renoux C, et al. Ventricular tachyarrhythmia and sudden cardiac death with domperidone use in Parkinson’s disease. Br J Clin Pharmacol. 2016. https://doi.org/10.1111/bcp.12964.
Kempster PA, Frankel JP, Stern GM, Lees AJ. Comparison of motor response to apomorphine and levodopa in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1990. https://doi.org/10.1136/jnnp.53.11.1004.
Gervason CL, Pollak PR, Limousin P, Perret JE. Reproducibility of motor effects induced by successive subcutaneous apomorphine injections in Parkinson’s disease. Clin Neuropharmacol. 1993. https://doi.org/10.1097/00002826-199304000-00003.
Katzenschlager R, et al. Apomorphine subcutaneous infusion in patients with Parkinson’s disease with persistent motor fluctuations (TOLEDO): a multicentre, double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2018. https://doi.org/10.1016/S1474-4422(18)30239-4.
Martinez-Martin P, et al. EuroInf: a multicenter comparative observational study of apomorphine and levodopa infusion in Parkinson’s disease. Mov Disord. 2015. https://doi.org/10.1002/mds.26067.
Deleu D, Hanssens Y, Northway MG. Subcutaneous apomorphine: an evidence-based review of its use in Parkinson’s disease. Drugs Aging. 2004. https://doi.org/10.2165/00002512-200421110-00001.
Acland KM, Churchyard A, Fletcher CL, Turner K, Lees A, Dowd PM. Panniculitis in association with apomorphine infusion. Br J Dermatol. 1998. https://doi.org/10.1046/j.1365-2133.1998.02128.x.
Skorvanek M, Bhatia KP. The skin and Parkinson’s disease: review of clinical, diagnostic, and therapeutic issues. Mov Disord Clin Pract. 2017. https://doi.org/10.1002/mdc3.12425.
Pietz K, Hagell P, Odin P. Subcutaneous apomorphine in late stage Parkinson’s disease: a long term follow up. J Neurol Neurosurg Psychiatry. 1998. https://doi.org/10.1136/jnnp.65.5.709.
Rosa-Grilo M, Qamar MA, Evans A, Chaudhuri KR. The efficacy of apomorphine—a non-motor perspective. Parkinsonism Relat Disord. 2016. https://doi.org/10.1016/j.parkreldis.2016.11.020.
Barbosa P, Lees AJ, Magee C, Djamshidian A, Warner TT. A retrospective evaluation of the frequency of impulsive compulsive behaviors in Parkinson’s disease patients treated with continuous waking day apomorphine pumps. Mov Disord Clin Pract. 2017. https://doi.org/10.1002/mdc3.12416.
Todorova A, Samuel M, Brown RG, Chaudhuri KR. Infusion therapies and development of impulse control disorders in advanced Parkinson disease: clinical experience after 3 years’ follow-up. Clin Neuropharmacol. 2015. https://doi.org/10.1097/WNF.0000000000000091.
Borgemeester RWK, Lees AJ, van Laar T. Parkinson’s disease, visual hallucinations and apomorphine: a review of the available evidence. Parkinsonism Relat Disord. 2016. https://doi.org/10.1016/j.parkreldis.2016.04.023.
Ellis C, et al. Use of apomorphine in Parkinsonian patients with neuropsychiatric complications to oral treatment. Parkinsonism Relat Disord. 1997. https://doi.org/10.1016/S1353-8020(97)00009-6.
Moore TJ, Glenmullen J, Mattison DR. Reports of pathological gambling, hypersexuality, and compulsive shop** associated with dopamine receptor agonist drugs. JAMA Intern Med. 2014. https://doi.org/10.1001/jamainternmed.2014.5262.
Samuel M, et al. Impulse control disorders in Parkinson’s disease:management, controversies, and potential approaches HHS public access. Mov Disord. 2015. https://doi.org/10.1002/mds.26099.Impulse.
Giladi N, Caraco Y, Gurevich T, Djaldetti R, Adar L, Rachmilewitz Minei T, Oren S. ND0612 (levodopa/carbidopa for subcutaneous infusion) achieves stable levodopa plasma levels when administered in low and high doses in patients with PD [abstract]. Mov Disord. 2017;32(suppl:2).
Giladi N, et al. Pharmacokinetic profile of ND0612 (levodopa/carbidopa for subcutaneous infusion) in Parkinson’s disease (PD) patients with motor fluctuations: results of a phase IIa dose finding study. Eur J Neurol. 2015. https://doi.org/10.1111/ene.12805.
Adar L, Minei TR, Cohen Y. Pharmacokinetic profile of continuous levodopa/carbidopa delivery when administered subcutaneously (ND0612) versus duodenal infusion (levodopa/carbidopa intestinal gel). Mov Disord. 2017. https://doi.org/10.1002/mds.27087.
Adar L, Rachmilewitz Minei T, Cohen Y, Oren S. Pharmacokinetic profile of continuous levodopa/carbidopa delivery when administered subcutaneously (ND0612) versus duodenal infusion (levodopa/carbidopa intestinal gel) [abstract]. Mov Disord. 2017;32(suppl:2).
Oren S, Kieburtz K, Olanow CW, Cohen Y. A randomized controlled clinical study to evaluate the efficacy and safety of subcutaneous levodopa/carbidopa (ND0612H) in patients with advanced Parkinson’s disease. J Parkinsons Dis. 2016. https://doi.org/10.3233/JPD-169900.
Adar L, Minei TR. Identification of the optimal carbidopa concentration in subcutaneously administered ND0612. Mov Disord. 2017. https://doi.org/10.1002/mds.27087.
L. P. et al. Indigo: a multicenter, randomized, double-blind, placebocontrolled, study of continuous ND0612 infusion with adjunct oral levodopa in fluctuating Parkinson’s disease. Mov Disord. 2018. http://dx.doi.org/10.1002/mds.27434.
Okun MS. Deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2012. https://doi.org/10.1056/NEJMct1208070.
Herrington TM, Cheng JJ, Eskandar EN. Mechanisms of deep brain stimulation. J Neurophysiol. 2016. https://doi.org/10.1152/jn.00281.2015.
Eusebio A, et al. Deep brain stimulation can suppress pathological synchronisation in parkinsonian patients. J Neurol Neurosurg Psychiatry. 2011. https://doi.org/10.1136/jnnp.2010.217489.
Okun MS, et al. Subthalamic deep brain stimulation with a constant-current device in Parkinson’s disease: an open-label randomised controlled trial. Lancet Neurol. 2012. https://doi.org/10.1016/S1474-4422(11)70308-8.
Deuschl G, et al. A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2006. https://doi.org/10.1056/NEJMoa060281.
Lachenmayer ML, et al. Stimulation of the globus pallidus internus in the treatment of Parkinson’s disease: long-term results of a monocentric cohort. Parkinsonism Relat Disord. 2019. https://doi.org/10.1016/j.parkreldis.2019.03.009.
Limousin P, Foltynie T. Long-term outcomes of deep brain stimulation in Parkinson disease. Nat Rev Neurol. 2019. https://doi.org/10.1038/s41582-019-0145-9.
Schuepbach WMM, et al. Neurostimulation for Parkinson’s disease with early motor complications. N Engl J Med. 2013. https://doi.org/10.1056/NEJMoa1205158.
Obeso JA, Olanow CW, Rodriguez-Oroz MC, Krack P, Kumar R, Lang AE. Deep-brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson’s disease. N Engl J Med. 2001. https://doi.org/10.1056/NEJMoa000827.
Bronstein JM, et al. Deep brain stimulation for Parkinson disease an expert consensus and review of key issues. Arch Neurol. 2011. https://doi.org/10.1001/archneurol.2010.260.
Anderson VC, Burchiel KJ, Hogarth P, Favre J, Hammerstad JP. Pallidal vs subthalamic nucleus deep brain stimulation in Parkinson disease. Arch Neurol. 2005. https://doi.org/10.1001/archneur.62.4.554.
Odekerken VJJ, et al. Subthalamic nucleus versus globus pallidus bilateral deep brain stimulation for advanced Parkinson’s disease (NSTAPS study): a randomised controlled trial. Lancet Neurol. 2013. https://doi.org/10.1016/S1474-4422(12)70264-8.
Ramirez-Zamora A, Ostrem JL. Globus pallidus interna or subthalamic nucleus deep brain stimulation for Parkinson disease a review. JAMA Neurol. 2018. https://doi.org/10.1001/jamaneurol.2017.4321.
Lyons KE, Wilkinson SB, Overman J, Pahwa R. Surgical and hardware complications of subthalamic stimulation: a series of 160 procedures. Neurology. 2004. https://doi.org/10.1212/01.WNL.0000134650.91974.1A.
Oh MY, et al. Long-term hardware-related complications of deep brain stimulation. Neurosurgery. 2002. https://doi.org/10.1097/00006123-200206000-00017.
Fenoy AJ, Simpson RK. Risks of common complications in deep brain stimulation surgery: Management and avoidance—clinical article. J Neurosurg. 2014. https://doi.org/10.3171/2013.10.JNS131225.
Constantinescu R, et al. Key clinical milestones 15 years and onwards after DBS-STN surgery—a retrospective analysis of patients that underwent surgery between 1993 and 2001. Clin Neurol Neurosurg. 2017. https://doi.org/10.1016/j.clineuro.2017.01.010.
Fasano A, et al. Motor and cognitive outcome in patients with Parkinson’s disease 8 years after subthalamic implants. Brain. 2010. https://doi.org/10.1093/brain/awq221.
Dayal V, Limousin P, Foltynie T. Subthalamic nucleus deep brain stimulation in Parkinson’s disease: the effect of varying stimulation parameters. J Parkinson’s Dis. 2017. https://doi.org/10.3233/JPD-171077.
Dafsari HS, et al. EuroInf 2: subthalamic stimulation, apomorphine, and levodopa infusion in Parkinson’s disease. Mov Disord. 2019. https://doi.org/10.1002/mds.27626.
Habets JGV, Heijmans M, Kuijf ML, Janssen MLF, Temel Y, Kubben PL. An update on adaptive deep brain stimulation in Parkinson’s disease. Mov Disord. 2018. https://doi.org/10.1002/mds.115.
Contarino MF, et al. Directional steering: a novel approach to deep brain stimulation. Neurology. 2014. https://doi.org/10.1212/WNL.0000000000000823.
Seppi K, et al. Update on treatments for nonmotor symptoms of Parkinson’s disease—an evidence-based medicine review. Mov Disord. 2019. https://doi.org/10.1002/mds.27602.
Schrag A, Sauerbier A, Chaudhuri KR. New clinical trials for nonmotor manifestations of Parkinson’s disease. Mov Disord. 2015. https://doi.org/10.1002/mds.26415.
Zesiewicz TA, et al. Practice parameter: Treatment of nonmotor symptoms of Parkinson disease: report of the quality standards subcommittee of the American academy of neurology. Neurology. 2010. https://doi.org/10.1212/WNL.0b013e3181d55f24.
Evans AH, Farrell MJ, Gibson SJ, Helme RD, Lim SY. Dyskinetic patients show rebound worsening of affect after an acute L-dopa challenge. Parkinsonism Relat Disord. 2012. https://doi.org/10.1016/j.parkreldis.2012.01.020.
Antonini A, et al. COMT inhibition with tolcapone in the treatment algorithm of patients with Parkinson’s disease (PD): Relevance for motor and non-motor features. Neuropsychiatr Dis Treat. 2008. https://doi.org/10.2147/ndt.s2404.
Ebersbach G, Hahn K, Lorrain M, Storch A. Tolcapone improves sleep in patients with advanced Parkinson’s disease (PD). Arch Gerontol Geriatr. 2010. https://doi.org/10.1016/j.archger.2010.03.008.
Muller T. Tolcapone addition improves Parkinson’s disease associated nonmotor symptoms. Ther Adv Neurol Disord. 2014. https://doi.org/10.1177/1756285613512392.
Wolz M, Hauschild J, Koy J, Fauser M, Klingelhöfer L, Schackert G, Reichmann H, Storch A. Immediate effects of deep brain stimulation of the subthalamic nucleus on nonmotor symptoms in Parkinson's disease. Parkinsonism Relat Disord. 2012;18(8):994–7.
Witjas T, et al. Effects of chronic subthalamic stimulation on nonmotor fluctuations in Parkinson’s disease. Mov Disord. 2007. https://doi.org/10.1002/mds.21602.
Odin P, et al. Collective physician perspectives on non-oral medication approaches for the management of clinically relevant unresolved issues in Parkinson’s disease: consensus from an international survey and discussion program. Parkinsonism Relat Disord. 2015. https://doi.org/10.1016/j.parkreldis.2015.07.020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
NV’s research time and position is funded by the Janet Owens charitable foundation. No funding was received specifically for this review.
Conflict of interest
NV has received educational support from Abbvie, Stada, Ipsen and Merc, speaker’s honorarium from Abbvie & Stada and served on advisory boards for Abbvie & Britannia Pharmaceuticals. TF has received grant support form Cure Parkinson’s trust, Michael J Fox Foundation, John Black Charitable Foundation, Van Andel Institute, Defeat MSA, Innovate UK, National Institute for Health Research. He has received honoraria for speaking at meetings sponsored by Bial, Profile Pharma, Britannia and Boston Scientific. He has served on advisory boards for Living Cell Technologies, Voyager Therapeutics and Oxford Biomedica.
Rights and permissions
About this article
Cite this article
Vijiaratnam, N., Foltynie, T. Therapeutic Strategies to Treat or Prevent Off Episodes in Adults with Parkinson’s Disease. Drugs 80, 775–796 (2020). https://doi.org/10.1007/s40265-020-01310-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-020-01310-2