Abstract
Background
Takayasu’s arteritis is a chronic vasculitis of unknown etiology affecting large vessels. Coronary involvement is rare and myocardial infarction as a presenting symptom has only been described in case reports.
Case
We report a case of a 19 year old female diagnosed with Takayasu’s arteritis 2 years prior who came in due to chest pain and heart failure symptoms. ECG showed diffuse ischemia with ST elevation of the inferior wall. Coronary angiogram showed 3 vessel disease with left main involvement. Patient was started on high dose steroids. She then developed an acute stroke in the right posterior cerebral artery territory. She improved with Methylprednisolone pulse therapy and oral methotrexate. She was discharged on Prednisone, Methotrexate and cardiac medications and is stable on follow up.
Diagnostics
Coronary angiogram showed ostioproximal stenosis of the distal left main segment, the proximal left anterior descending artery and the proximal left circumflex artery, with the right coronary artery being totally occluded. Two dimensional echocardiogram showed an ejection fraction of 38 percent with multisegmental wall motion abnormalities. CT aortogram showed segmental narrowing of the infrarenal abdominal aorta with multiple ostioproximal stenosis of several aortic branches with extensive collateral formation. MRI showed acute infarction in the right thalamus,right medial temporal and occipital lobes and right cerebellar hemisphere and vermis
Conclusion
Takayasu’s arteritis can present with a myriad of vascular complications. The reported incidence of coronary involvement is low. This case highlights the progressive and unpredictable nature of this disease. A high index of clinical suspicion, as well as a meticulous search for the extent of disease severity allows the clinician to individualize treatment options for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
I. Introduction
Takayasu’s arteritis is a granulomatous inflammation of the large vessels that mainly affects the aorta and its major branches. It was named after Dr. Mikito Takayasu, a Japanese ophthalmologist who described it in 1908 as a clinical syndrome characterized by eye complications[1] and accentuated pulse weakness, hence it is also referred to classically as pulseless disease. Although its etiology and pathogenesis are unknown, an autoimmune mechanism is postulated2. Its presentation may vary depending on the extent of vascular involvement. Cases presenting as acute myocardial infarction are rare. We report a patient with Takayasu’s arteritis who presented with acute coronary syndrome. Workup revealed the extent of her disease and she developed an acute ischemic stroke during her hospital stay.
II. Case presentation
A 19 year old female came into our institution with a chief complaint of severe sudden onset chest pain of a few hours duration. She has likewise been experiencing exertional dyspnea,orthopnea and paroxysmal nocturnal dyspnea since 3 months prior. She was reportedly diagnosed with Takayasu’s arteritis 2 years prior but was lost to follow up.
On physical examination the patient was conscious and coherent. Blood pressure at the right upper extremity was 100/70 mmHg, 110/70 at the left upper extremity and 130/90 on both lower extremities derived via Doppler measurements. Heart rate was regular at 72, respiratory rate was 22 cycles per minute and she was afebrile. She had a body mass index of 18.7 kg/m2. There was note of bilateral carotid bruits. Cardiovascular examination revealed a soft s1 with a 2/6 holosystolic murmur at the apex. Pulses were not appreciated on the right upper extremity and weak on the left upper extremity.
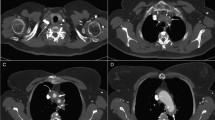
On admission, ECG showed inferior wall ST elevation myocardial infarction and Troponin I was positive at 0.461ng/ml. C reactive protein was elevated slightly at 20.2mg/L. Creatinine and electrolytes were normal. Chest radiograph showed cardiomegaly with pulmonary congestion. She then had an episode of ventricular fibrillation and was defibrillated. Referral to Invasive Cardiology was done. Coronary angiogram showed 3 vessel disease with left main involvement (Figure 1). She was started on Heparin drip and referred to Thoracic and Cardiovascular Surgery, Rheumatology and Vascular Services. Hydrocortisone 100mg/IV every 12 hours was started. Two dimensional echocardiogram showed an ejection fraction of 38% with concentric left ventricular hypertrophy with multisegmental wall motion abnormality indicative of coronary artery disease with depressed systolic function and grade III diastolic dysfunction with severe mitral regurgitation. Carotid Duplex Scan showed >50% stenosis of the left internal carotid artery(ICA) and total occlusion of the right common carotid artery. Vertebral arteries were totally occluded bilaterally. (Figure 2) CT Aortogram showed segmental narrowing of the infrarenal abdominal aorta and multiple ostioproximal stenosis, with almost total occlusion of the proximal left subclavian artery, and total occlusion of the proximal superior mesenteric artery. There was also a 70-80% stenosis of the proximal right renal artery and almost total occlusion of the ostium of the left renal artery. (Figure 3) The patient improved clinically with resolution of the previously noted ST segment elevation. The plan was to do Off pump coronary artery bypass (OPCAB). However she developed left sided weakness, dizziness and slurring of speech on her 7th hospital day. Cranial magnetic resonance imaging (Figure 4) showed acute infarction of the right thalamus, right medial temporal and occipital lobes and right cerebellar hemisphere and vermis. Patient was then brought to the Medical ICU for closer monitoring. She was started on Methylprednisolone pulse therapy for three days. There was noted improvement of the patient’s neurologic symptoms. Medications were continued including Prednisone 40mg/day and Methotrexate 10mg once a week. She was cleared for discharge and was stable on follow up.
III. Diagnostics

Figure 1

Figure 2

Figure 3

Figure 4
IV. Discussion
Takayasu’s arteritis is a chronic inflammatory disease of unknown cause. It has worldwide distribution but is more common in Asia most notably Japan, India and China [2]. It has an estimated incidence of 2.6/100,000,0/year with a female to male ratio of 2-3:1. [3] The disease onset is insidious, presenting initially with nonspecific and constitutional signs and symptoms (pre vasculitic phase) and progressing to involve branches of the aorta. This phase (vasculitic or pulseless phase) is characterized by diminished or absent pulses, hypertension, claudication and neurological involvement as well as other forms of vascular insufficiency. This may or may not be accompanied by flares. Aortic insufficiency, heart failure and stroke as well as renal artery stenosis have been described in literature. [4] The third stage is the burned-out stage, when fibrosis sets in, and generally is associated with remission.
The first classification and natural history of Takayasu's arteritis was reported by Ishikawa in 1985, which he based on the severity of involvement and the presence of complications.[5] In 1990 the American College of Rheumatology established the criteria for classification of disease based on age of diagnosis of <40 years old and the presence of the following: presence of claudication, decreased brachial artery pulse, blood pressure difference >10mmHg, bruit over subclavian arteries and arteriogram abnormality. [6] This classification was then revised by Sharma et al[7] removing the age of onset of <40 years old, including characteristic signs and symptoms and coronary artery involvement.
After recognition of specific signs and symptoms, elevation of acute phase reactants have been proposed to determine the presence of active disease. While widely used, these are non specific measures and had low sensitivity and specificity in reflecting disease flares. Our patient only had a modest elevation of C reactive protein (CRP) which eventually normalized. Based on the NIH criteria, the presence of symptoms and elevation of acute phase reactants as well as evidence of findings on imaging are indicative of active disease. [8] Other measures to determine disease activity such as Matrix Metalloproteinases or Pentraxin have been studied and were found superior to both erythrocyte sedimentation rate and CRP. [9]
Imaging studies complement the clinical and laboratory evaluation. While arteriography is classically considered the gold standard to visualize the extent of arterial involvement, other imaging modalities may be used. Doppler ultrasound is non invasive and can identify occlusive changes and measure post stenotic velocity. CT angiography and magnetic resonance imaging and angiography can identify occlusive lesions with very good specificity and sensitivity. Imaging studies facilitate early diagnosis and provide assessment of disease extent, inflammatory activity and response to treatment. [10] Mason reported a comparison of different imaging modalities and concluded that no single modality provides all the information required and that each may have complimentary roles. [11]
The incidence of coronary artery involvement has been reported to be 9% to 10%, and is observed mainly in autopsy cases. Coronary artery disease is usually not evident until the occurrence of angina pectoris or myocardial infarction, or after the onset of congestive heart failure. Based on the report by Masubara et al, [12] the following three types of coronary artery lesions can be distinguished: type 1, stenosis or occlusion of the coronary ostia and the proximal segments of the coronary arteries.Type 2, diffuse or focal coronary arteritis, which may extend diffusely to all epicardial branches or may involve focal segments, so-called skip lesions; and type 3, coronary aneurysm. Type 1 occurs in 2/3 of patients as was the case in our patient Nasu reported a 10.5% rate of coronary lesions that complicated Takayasu's arteritis.[13] Patients have predisposition to inflammation and atherosclerosis. Coronary ostial stenosis occurs as a result of the extension of inflammation, which induces intimal proliferation and fibrous contraction in the ascending aorta around the coronary ostia.[14] Inflammation may involve the entire epicardial tree. Our patient presented with angina pectoris which is an unusual presentation, reported in about 6-16% of cases. Myocarditis, pericarditis and cardiomyopathy have also been reported.[15]
Interventional treatment for our patient is problematic. There have been reports of successful stent placement for renal artery stenosis and subclavian stenosis, the results of which require additional follow up. [16;17] Percutaneous catheter intervention of the coronary arteries have been done but was associated with a high frequency of re-stenosis [18]. Drug eluting stents may have potential benefit. [19]
Surgical options are coronary artery bypass graft, surgical angioplasty of the left main coronary artery, and transaortic coronary ostial endarterectomy [20]. The timing of the operation is important, and surgical treatment should generally be avoided during the active inflammatory stage of disease. With the patient being a high risk patient our initial plan for the patient was to undergo off pump coronary artery bypass graft (OPCAB). It was initially postulated that the use of saphenous vein grafts may be more beneficial in these patients due to a high restenosis rate for arterial grafts.[21] However Kwon Joong et al reported very good outcomes with OPCAB as well as use of in situ arterial grafts[22].
Both medical and surgical modalities play an important role in the management of Takayasu’s arteritis. Our patient experienced a stroke during her hospital stay prior to the planned surgery. Patient also has bilateral renal artery stenosis. Renal function and urine output were maintained due to the extensive collateralization. With all these high risk features we decided to treat our patient with optimal medical management. While steroids are the mainstay of treatment, newer immunosuppressant medications have shown promise such as immunosuppressants and cytotoxic agents. Prednisone is usually prescribed followed by a slow taper. This therapy allows for 67% remission, but up to 50% treated individuals will relapse. Relapses are treated with either increasing corticosteroid dose or the addition of a corticosteroid sparing immunosuppressant such as methotrexate as well as other immunosuppressive drugs. [23]
The prognosis for our patient is generally poor. According to the Ishikawa classification, the presence of major complications such as heart failure, acute MI and a progressive course showed the worst prognosis of only 43% survival at 15 years [24]. Another study by Park et al showed a 10 year survival rate of 87.2 %, with the presence of more than two complications rendering a 66.9% survival at 5 years and a 36.7% at 10 years respectively. Independent prognostic factors were low ESR, treatment with steroids and stable disease activity.[25]
There have been reports of Takayasu arteritis with global arterial involvement involving the coronary arteries. [26] To our knowledge this is the first report of a patient presenting with myocardial infarction and complicated by stroke. Wheeler et al reported a case of a vasculitis presenting with myocardial infarction, stroke and aortitis[27]. It was not specified whether the patient had Takayasu’s arteritis or giant cell arteritis. In our patient this was also accompanied by bilateral renal artery stenosis and heart failure attributable to left ventricular dysfunction. There was no aortic insufficiency noted. The presence of many vascular complications and active disease flare precluded us from pushing through with our surgical plans. There have been reports of successful angiographic regression of atherosclerosis in patients with maximal medical therapy alone[28;29;30].This patient warrants close and continuous monitoring with imaging studies at least every 3-6 months as well as compliance to medications. [31].
V. Conclusion
Takayasu’s arteritis is a chronic and granulomatous vasculitis of the large elastic arteries that presents as a combination of vaso-occlusive disease and systemic inflammation. While coronary involvement is rare its inflammatory pathophysiology implies that any vascular complication is possible. It still remains both a diagnostic and therapeutic challenge. This case highlights the enigmatic and progressive nature of Takayasu’s arteritis and the need for vigilance in its diagnosis and monitoring. Treatment is individualized incorporating both effective immunosuppressive therapy and timely surgical management.
References
Takayasu M. A case with peculiar changes of the central retinal vessels. Acta Soc Opthalmol Jpn. 1908; 12: 554-555
Kimura A, Kitamura H, Date Y, Numano F. Comprehensive analysis of HLA genes in Takayasu arteritis in Japan. Int J Cardiol 1996; 54 Suppl:S61.
Dabague J, Reyes PA. Takayasu arteritis in Mexico: a 38-year clinical perspective through literature review. Int J Cardiol 1996; 54 Suppl:S103.
Hall S, Barr W, Lie JT, Stanson AW, Kazmier FJ, Hunder GG. Takayasu arteritis. A study of 32 North American patients. Medicine (Baltimore) 1985;64:89-99.
Ishikawa K, Maetani S. Long-term outcome for 120 Japanese patients with Takayasu disease: clinical and statistical analyses of related prognostic factors. Circulation. 1994;90:1855-1860.
Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 1990, 33:1129-34. http://doi.org/dh2dz8
Sharma BK, Jain S, Suri S, Numano F. Diagnostic criteria for Takayasu arteritis. Int J Cardiol 1996; 54 : S141-S147
Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS. Takayasu arteritis. Ann Intern Med. 1994;120:919-929.
Ishihara T, Haraguchi G, Tezuka D, Kamiishi T, Inagaki H, Isobe M. Diagnosis and assessment of Takayasu arteritis by multiple biomarkers. Circ J. 2013;14:477-83. doi: 10.1253/circj.CJ-12-0131
Pipitone N, Versari A, Salvarani C. Role of imaging studies in the diagnosis and follow-up of large-vessel vasculitis: an update. Rheumatology (Oxford) 2008;14:403-8.
Mason J. Takayasu arteritis—advances in diagnosis and management. Nat Rev Rheumatol 2010;6:406-15
Matsubara O, Kuwata T, Nemoto T, Kasuga T, Numano F. Coronary artery lesions in Takayasu arteritis: pathological considerations. Heart Vessels Suppl 1992;7:26-31.
Noma M, Sugihara M, Kikuchi Y. Isolated coronary ostial stenosis in Takayasu’s arteritis: case report and review of the literature. Angiology 1993;44:839-44.
G. Venkata Ramana Kumar et al, Takayasu's Arteritis with Ostial and Left Main Coronary Artery Stenosis, Tex Heart Inst J. 2007; 34(4): 470-474.
S Malik et al, Takayasu's arteritis: management of left main stem stenosis, Heart. Mar 2003; 89(3): e-9.
Sharma, et al, A follow-up study of balloon angioplasty and de-novo stenting in Takayasu arteritis, Int J Cardiol. 2000 Aug 31;75 Suppl 1:S147-52.
Liang P, Tan-Ong M, Hoffman GS. Takayasu’s arteritis: vascular interventions and outcomes. J Rheumatol. 2004;31:102-6.
Yokota, et al A case of Takayasu arteritis with repeated coronary artery restenosis after drug-eluting stent implantation successfully treated with a combination of steroids, Intern Med. 2012;51(7):739-43. Epub 2012 Apr 1.
Furukawa, et al, Sirolimus-eluting stent for in-stent restenosis of left main coronary artery in takayasu arteritis, Circ J. 2005 Jun;69(6):752-5.
Endo M, Tomizawa Y, Nishida H, Aomi S, Nakazawa M, Tsurumi Y, et al. Angiographic findings and surgical treatments of coronary artery involvement in Takayasu arteritis. J Thorac Cardiovasc Surg 2003;125:570-7
Cipriano PR, Silverman JF, Perlroth MG, Griepp RB, Wexler L. Coronary arterial narrowing in Takayasu's aortitis. Am J Cardiol 1977;39:744-50
Kwon Joong Na, et al, Anaortic Off-pump Coronary Artery Bypass Grafting in Patients with Takayasu's Arteritis, Korean J Thorac Cardiovasc Surg. Aug 2013; 46(4): 274-278.
Vishnumurthy Shushrutha Hedna, et al Takayasu's arteritis: Is it a reversible disease? Case Report and Literature Review, Surg Neurol Int. 2012; 3: 13-2.
Subramanyan R, Joy J, Balakrishnan KG, et al. SCT. Natural history of aortoarteritis (Takayasu’s arteritis). Circulation 1989; 80: 429-37.
Park MC1, Lee SW, Park YB, Chung NS, Lee SK. Clinical characteristics and outcomes of Takayasu's arteritis: analysis of 108 patients using standardized criteria for diagnosis, activity assessment, and angiographic classification. Scand J Rheumatol. 2005 Jul-Aug;34(4):284-92
Ahmed W, Ahmad Z. Takayasu’s Arteritis: A Case Report with Global Arterial Involvement. RMJ. 2005;30(1):43-45
Wheeler et al, Vasculitis Presenting with Myocardial Infarction, Stroke, and Aortitis in a Middle-aged Man, St. Luke’s Hospital and Health Network, Bethlehem, Pennsylvania
Ishikawa K, Yonekawa Y, Regression of carotid stenosis after corticosteroid therapy in occlusive thromboaortopathy (Takayasu’s disease), Stroke, 1987 May-Jun.18(3)677-9
Iga, K et al, Regression of the left main trunk lesion by steroid administration in Takayasu’s aortitis, Chest, 1991 Feb;99(2):508-10
Dela Cueva, J, et al, A Case of Takayasu’s Disease Presenting as Severe Secondary Hypertension With Angiographic Improvement Following Medical Treatment, Rev Esp Cardio 2010,63.365-7 Vol 63 NUm .03
Mukhtyar, C. et al. EULAR recommendations for the management of large vessel vasculitis. Ann. Rheum. Dis. 68, 318-323 (2009).
Author information
Authors and Affiliations
Additional information
Authors’ Profile





This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cuenza, L., Grayda, J., Natividad, T. et al. Three Vessel Disease with Left Main Involvement: A Rare Manifestation of Takayasu’s Arteritis. GSTF J Adv Med Res 1, 20 (2014). https://doi.org/10.7603/s40782-014-0020-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.7603/s40782-014-0020-y