Abstract
Background
Lung CT imaging may reveal COVID-19 abnormalities earlier than RTPCR. CT may be more sensitive than RT-PCR for diagnosing COVID-19-related pneumonia.
Aim
This study assesses the accuracy of multi-slice computed tomography (MSCT) grading in predicting COVID-19 mortality.
Methods
COVID-19 RT-PCR. For severity scores, all patients’ clinical examinations, history, and chest MSCT data were collected.
Results
According to the chest MSCT score, 102 (51.5%), 70 (35%), and 28 (14%) patients had mild, moderate, and severe illness. Out of the patients, 62 (31%) died, and 69% survived. Patients with severe MSCT scores showed a considerably greater mean age than other groups (P < 0.001). Moreover, this group had a considerably higher mean BMI (P < 0.001), and a majority (57.1%) were obese (P < 0.001). Compared to the mild group, the moderate and severe groups had significantly increased rates of diabetes, hypertension, and liver disease (P < 0.001). The moderate group had a greater rate of no comorbidities (P < 0.001). A severe MSCT score was linked to increased leucocytes, C-reactive protein, ESR, ferritin, d-dimer, HbA1c, and fasting blood sugar, as well as decreased mean lymphocytes (P < 0.001). Severe MSCT scores were linked to increased ICU admissions (P < 0.001) and increased demand for advanced mechanical ventilation and oxygen assistance (P < 0.001). A severe MSCT score was associated with the highest death rate, followed by a moderate MSCT score. Low mortality rates were observed in mild MSCT-scored patients (P < 0.001).
Conclusion
MSC T score severity is a reliable and noninvasive way to predict COVID-19 mortality
Similar content being viewed by others
Background
Computed tomography (CT) has been extensively employed to identify and investigate suspected or affirmed cases of COVID-19 on a large scale [1]. Based on existing empirical evidence, it has been observed that lung CT imaging has the potential to detect abnormalities at an earlier stage compared to RT-PCR testing. Recent studies have indicated that MSCT may exhibit greater sensitivity compared to RT-PCR when diagnosing pneumonia associated with COVID-19. High-resolution computed tomography (HRCT) has become a dominant modality for initial diagnosis, screening, and assessment of disease intensity [2, 20].
According to recent studies, ground-glass opacity (GGO) is the most prevalent discovery in COVID-19-linked pneumonia. Most cases include both the lungs and peripheral subpleural distribution. The imaging findings are nonspecific; however, other radiological features have been described [3, 19].
Few studies have examined COVID-19 chest CT discoveries’ short-term prognostic value. Individuals who were seriously ill exhibited a higher prevalence of consolidation patterns, air bronchograms, crazy paving, central lung involvement (peri-bronchovascular), and pleural effusion. These data may suggest COVID-19’s severity and aggressiveness. Thus, these radiologic features may be predictive imaging indicators in COVID-19 pneumonia cases [4]. However, this research aimed to evaluate the MSCT score’s predictive accuracy in COVID-19 patients.
Methods
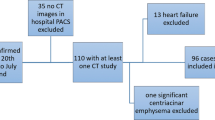
The current study is a retrospective and prospective observational investigation carried out in a university hospital and other quarantine hospitals for the duration of the study, spanning from November 2021 to May 2022. The study included a group of 200 individuals who had been diagnosed with COVID-19. The diagnosis was made by verifying the presence of COVID-19 nucleic acid using real-time reverse transcription-polymerase chain reaction (rRT-PCR) on swab specimens taken from the respiratory tract. Exclusion criteria include those without a prior CT scan, those with severe cardiac disease, or those with previous pulmonary disease.
All cases were subjected to the following:
-
I.
Complete history-taking: It includes demographic and clinical data.
-
II.
Complete clinical examination: A comprehensive clinical evaluation encompassing the assessment of overall status and vital signs, including blood pressure, pulse, temperature, and respiration rate, was performed. The medical practitioner conducted examinations of the abdomen, thorax, and heart. The researchers conducted the height and weight measurements and subsequently computed the body mass index (BMI) by dividing the weight (expressed in kilograms) by the height (expressed in M2).
-
III.
Laboratory investigations: Blood specimens were obtained from the patients and utilized to investigate the parameters listed below:
-
1.
Complete blood count (CBC): CBC includes hemoglobin concentration (Hb%), white blood cells (WBCs), red blood cells (RBC), neutrophil count, lymphocyte count, and platelet count.
-
2.
The study assessed fasting, random blood glucose levels, and HbA1c. The criteria for diagnosing diabetes included a fasting blood glucose level equal to or greater than 126 mg/dL, a glycated hemoglobin level equal to or greater than 6.5%, the use of hypoglycemic medications, or a self-reported history of diabetes.
-
3.
Renal profile: Blood urea and creatinine (Cr) were evaluated.
-
4.
Liver profile: Aspartate aminotransferase (AST), alanine transaminase (ALT), albumin, and serum total bilirubin were evaluated.
-
5.
CRP, ferritin, and D-dimer were evaluated.
-
1.
-
IV.
Radiological investigations: The radiologist reported an X-ray chest and a CT chest for all patients. During the chest examination using computed tomography (CT), all chest x-ray films and CT images were reviewed by the radiologists with more than 10 years of experience and blinded to the clinical data and laboratory indicators; a visual scoring system was employed to assess the condition of each of the five lung lobes. The scoring scale ranged from 0 to 5, with greater scores demonstrating greater severity or abnormality. The levels of involvement can be categorized as follows: 0 reveals no involvement, 1 indicates involvement of less than 5%, 2 indicates involvement of 25%, 3 indicates involvement ranging from 26 to 49%, 4 indicates involvement ranging from 50 to 75%, and 5 indicates involvement above 75%.
-
V.
MSCT severity scoring: The primary objective of this study was to evaluate various computed tomography (CT) characteristics, including the spatial distribution of lesions (peripheral, central, or both), the extent of involvement in terms of the number of influenced lobes (one, two, three, four, or five), the morphological characteristics of lesions (patchy or nodular), the visual appearance of lesions (consolidation, ground-glass opacity (GGO), or GGO with consolidation), specific signs observed within the lesions (crazy paving pattern, vascular thickening, halo sign, air bronchogram sign, and fibrosis), the size of the largest lesion (less than 1 cm, 1–3 cm, and greater than 3 cm), and any additional manifestations outside the lungs (including enlargement of mediastinal and hilar lymph nodes, pleural thickening, and pleural effusion). The COVID 19-CT severity scoring was conducted for each unique incident using the methodology outlined by Yang et al. [5]. The scoring methodology was employed to calculate the severity of disease involvement in each of the five lobes present in both lungs. A score of zero indicates the lack of lung tissue involvement, whereas a score of one indicates participation of less than five percent. The 2, 3, 4, and 5 scores indicated progressively higher degrees of participation, encompassing 5–25% (Fig. 1), 26–50% (Fig. 2), 51–75%, and above 75% parenchymal involvement (Fig. 3), respectively. The aggregate global CT score was determined by totaling the individual lobar scores, encompassing a variation from 0 to 25. Scores varying from 0 to 1 were categorized as moderate. Scores ranging from 2 to 3 were categorized as moderate. Scores of 4 or 5 were categorized as indicative of a significant condition.
-
VI.
All patients received medical treatment following Egypt’s Ministry of Health and Population guidelines.
Sample size
The sample size calculation was performed using EpI-Info 2002 software statistical package designed by World Health Organization (WHO) and by Centers for Disease Control and Prevention (CDC). The sample size was calculated based on the following considerations: 95% confidence level, and the prevalence of mortality was 30% according to a previous study [6] ± 5% confidence limit. Six cases were added to overcome dropout. Therefore, we will recruit 200 cases.
Statistical analysis
For data analysis, SPSS version 24 for Windows was utilized. Numerical data with normal distributions had means and standard deviations. The numerical variable distribution’s normality was validated with Kolmogorov-Smirnov. The chi-square test examined categorical variable associations. In cases of assumption violations, the fissure exact test was applied. An independent sample t-test was employed to compare parametric numerical variables across different groups. A P-value of less than 0.05 was deemed to be statistically significant.
Results
The current study involved a cohort of 200 cases diagnosed with a verified case of COVID-19. According to the chest MSCT grading system, the distribution of disease severity among the patients was as follows: 102 individuals (51.5%) had a mild illness, 70 individuals (35%) had a moderate disease, and 28 individuals (14%) had a severe disease. Among the patients mentioned above, 62 individuals, including 31% of the sample, suffered death from the disease, while the remaining 69% of patients survived.
Baseline characteristics of the studied cases dependent on BMI
The study revealed that the severe group had a statistically significant higher mean age (M = 63.50, SD = 11.73) when compared to the other categories. Furthermore, the group had a notably higher average BMI of 34.35 ± 13.62. Furthermore, most individuals (57.1%) within this group were classified as obese (Table 1).
The frequency of diabetes mellitus, hypertension, and liver disease was considerably greater in the moderate and severe groups compared to the mild group. In contrast, the mild group had a greater prevalence of individuals without comorbidities, amounting to 31.4% of the sample. No statistically significant differences were seen between the groups under investigation, as indicated by additional data (Table 1).
Laboratory and clinical data of studied cases dependent on MSCT severity
No significant variations were observed in various clinical data across different groups of patients categorized based on chest MSCT score activity. The study revealed that the severe group exhibited significantly elevated levels of leucocytes, erythrocyte sedimentation rate, C-reactive protein, glycosylated hemoglobin, ferritin, d-dimer, and fasting blood sugar, while the results showed lower mean lymphocyte counts. Additional data indicated no statistically significant variations (Table 2).
Nutrition index, hospital stay, and oxygen therapy in studied patients based on MSCT scoring severity
No significant differences were observed regarding hospital stay and nutrition ratio across various patient groups categorized based on MSCT score severity. However, it was found that the severe group had a much greater rate of admission to the ICU, with all patients in this group requiring ICU care (Table 2).
As illustrated in Table 3, a notable disparity was noticed among patient groups in terms of scoring activity as well as the mode of mechanical ventilation and oxygen support. The study revealed that a significant proportion of individuals in the mild group (98%) and moderate group (54.3%) had improved and were subsequently discharged. Conversely, all patients in the severe group exhibited deterioration and ultimately succumbed to the illness.
Different complications among the studied cases dependent on MSCT scoring severity
There were notable variations in the occurrence of different difficulties across numerous groups based on the severity of MSCT grading, except for neurological issues, where the difference was not statistically significant (P = 0.15). ARDS had a notably high prevalence within the severe group (64.3%) and the moderate group (22.9%) (Table 4).
Acute myocardial infarction, heart failure, atrial fibrillation, and uncontrolled hypertension were observed in 8 (11.4%), 2 (2.9%), 2 (2.9%), and 4 (5.7%) patients in the moderate group and 4 (14.3%), 2 (7.1%), 6 (21.4%), and 6 (21.4%) patients in the severe group, respectively. Six patients with modest severity experienced both heart failure and uncontrolled hypertension. Ten (35.7%), 8 (11.4%), and 6 (5.9%) patients of severe, moderate, and mild groups, respectively, developed acute hepatitis. Two patients in the mild group developed pancytopenia, and another four had thrombocytopenia. Thrombocytopenia occurred in four patients with moderate scores (Table 4).
Deep vein thrombosis (DVT) and thrombocytopenia occurred in four cases in the severe group. Two patients in the moderate group developed diabetes mellitus, while four patients in the severe group had subacute thyroiditis. Bed sores were absent in the mild group, whereas 10 (14.35) and 16 (57.1%) patients with moderate and severe illnesses, respectively, had bed sores (Table 4).
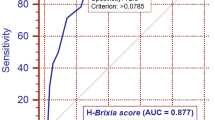
Accuracy of MSCT scoring prediction of mortality among cases with COVID-19
It was found that MSCT scoring severity had 100% accuracy in predicting mortality in patients with COVID-19 with the area under the curve of 0.726 (Table 5 and Figs. 4, 5, and 6).
Univariate and multivariate regression of different complications versus chest MSCT scoring severity
In univariate regression, respiratory complications, cardiovascular complications, acute kidney injury, acute hepatitis, hematological complications, endocrine complications, and bed sores were independent predictors of chest MSCT scoring severity (P-value < 0.05).
In multivariate regression, cardiovascular complications, acute kidney injury, acute hepatitis, endocrine complications, and bed sores were independent predictors of chest MSCT scoring severity (P-value < 0.05), while respiratory complications and hematological complications were not (Table 6).
Discussion
A targeted viral diagnostic assay utilizing RT-PCR was quickly created to ascertain the diagnosis of COVID-19. While the diagnostic test is widely regarded as the gold standard, it is vital to find that certain individuals may experience false-negative outcomes [7]. The potential cause of this issue could be a lack of adequate cellular material for detection and the nucleic acid’s unsuitable extraction from clinical specimens. The variety in the RT-PCR data emphasizes the importance of using an adjunctive diagnostic methodology [14] noted that COVID-19 cases with severe or critical disease had a higher CT severity score than patients with moderate disease in their study of 50 COVID-19 cases.
This is aligned with Hefeda’s [15] study, which revealed that most patients with consolidation had a significant mortality rate. Crazy paving and consolidation are more likely in advanced-illness patients [15].
In addition, the Parry et al. [16] study found that clinically unstable patients had a higher crazy paving and consolidation appearance.
Moreover, Francone et al. [12] reported that GGO tends to be more prevalent in early cases, in contrast to crazy paving and consolidation patterns, which are more frequently noted in later stages.
Furthermore, Feng et al. [17] noted that individuals with a progressing condition have a radiographic finding known as a “crazy paving sign,” which indicates interstitial thickness.
This study’s results demonstrated that the severity of MSCT scoring demonstrated a 100% accuracy rate in anticipating the mortality of cases diagnosed with COVID-19. The area under the curve for this prediction was calculated to be 0.726.
In line with our study, the receiver operating characteristic (ROC) curve in the Magdy et al. [10] study showed that the CT severity score highly predicts short-term clinical outcomes in COVID-19 cases. A cut-off value of ≥ 19 was found to be particularly indicative of short-term death, with a sensitivity of 100%, a specificity of 91.9%, and an accuracy of 92.56%.
Furthermore, Francone et al. [12] asserted that a CT severity score equal to or greater than 18 out of 25 exhibits a strong predictive capability for death in COVID-19 patients throughout their immediate posttreatment monitoring period. Furthermore, Zhou et al. [18] have documented that a CT severity score cut-off value of 16.5/25 points yielded a sensitivity of 69.4% and specificity of 82.3% in prognosticating unfavorable outcomes among individuals diagnosed with COVID-19.
This study has limitations. The CT-SS assumes lung opacification, which indicates COVID-19 presence. These findings were not histologically confirmed. We also selected the first chest CT scan taken upon admission. Thus, the analysis was unaffected by symptom duration, which could influence scoring system interpretation. Our data show that severe patients had a considerably longer time between symptom onset and hospital admission than moderate patients.
Conclusion
Overall, this study presents a simple yet effective way for evaluating the extent of COVID-19 severity based on the initial chest CT scans. In our sample, a CT-SS score shows 51.5% had a mild illness, 35% had a moderate disease, and 14% had a severe disease. CT-SS has the ability to accelerate the process of determining whether patients require hospital admission. We believe that this strategy could be valuable in situations where there are a large number of patients, limited healthcare resources, or restricted polymerase chain reaction testing capabilities. Moreover, it is worth noting that age can be determined as a significant risk factor for the severity of MSCT scoring in cases diagnosed with COVID-19.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- RT-PCR:
-
Reverse transcription polymerase chain reaction
- MSCT:
-
Multi-slice computed tomography
- ESR:
-
Erythrocyte sedimentation rate
- HRCT:
-
High-resolution computed tomography
- GGO:
-
Ground-glass opacity
- BMI:
-
Body mass index
- ARDS:
-
Adult respiratory distress syndrome
- DVT:
-
Deep venous thrombosis
References
Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H et al (2020) Imaging profile of the COVID-19 infection: radiologic findings and literature review. Rad Cardiothorac Imaging. 2:e200034
**ong Y, Sun D, Liu Y, Fan Y, Zhao L, Li X et al (2020) Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest Radiol. 55:332–9
Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N et al (2020) Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 295:200463
Tabatabaei SMH, Rahimi H, Moghaddas F, Rajebi H (2020) Predictive value of CT in the short-term mortality of coronavirus disease 2019 (COVID-19) pneumonia in nonelderly patients: a case-control study. Eur J Radiol. 132:109298
Yang R, Li X, Liu H, Zhen Y, Zhang X, **ong Q et al (2020) Chest CT severity score: an imaging tool for assessing severe COVID-19. Radiol Cardiothorac Imaging 2:e200047
Said AF, El-Fateh AH, Esmaeel TEZ, Mady AF (2024) 4C mortality score and CT severity score among COVID-19 patients: a single center prospective study. Egyptian J Radiol Nuclear Med 55:34
Ye Z, Zhang Y, Wang Y, Huang Z, Song B (2020) Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 30:4381–9
**e X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J (2020) Chest CT for typical coronavirus disease 2019 (COVID-19) pneumonia: relationship to negative RT-PCR testing. Radiology 296:E41-e5
Faheem MH, Gomaa A, Allam AH (2022) Prognostic significance of COVID-19 MSCT chest findings on short-term disease progression. Egyptian J Bronchol 16:34
Magdy AM, Saad MA, El Khateeb AF, Ahmed MI, Gamal El-Din DH. Comparative evaluation of semi-quantitative CT-severity scoring versus serum lactate dehydrogenase as prognostic biomarkers for disease severity and clinical outcome of COVID-19 patients: Egypt J Radiol Nucl Med. 2021;52(1):114. https://doi.org/10.1186/s43055-021-00493-2. Epub 2021 Apr 28.; 2021.
Farghaly S, Makboul M. Correlation between age, sex, and severity of coronavirus disease-19 based on chest computed tomography severity scoring system: Egypt J Radiol Nucl Med. 2021;52(1):23. doi: https://doi.org/10.1186/s43055-021-00408-1. Epub 2021 Jan 13.; 2021.
Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L et al (2020) Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol. 30:6808–17
Ioannidis JPA, Axfors C, Contopoulos-Ioannidis DG (2020) Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 188:109890
Liu N, He G, Yang X, Chen J, Wu J, Ma M et al (2020) Dynamic changes of chest CT follow-up in coronavirus disease-19 (COVID-19) pneumonia: relationship to clinical ty**. BMC Med Imaging. 20:92
Hefeda MM (2020) CT chest findings in patients infected with COVID-19: review of literature. Egyptian J Radiol Nuclear Med 51:239
Parry AH, Wani HA, Choh NA, Shah NN, Jehangir M (2021) Spectrum of chest CT manifestations of coronavirus disease (COVID-19): a pictorial essay. Indian J Radiol Imaging. 31:S170-s7
Feng Z, Yu Q, Yao S, Luo L, Zhou W, Mao X et al (2020) Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nat Commun. 11:4968
Zhou S, Chen C, Hu Y, Lv W, Ai T, **a L (2020) Chest CT imaging features and severity scores as biomarkers for prognostic prediction in patients with COVID-19. Ann Transl Med. 8:1449
Szabó M, Kardos Z, Kostyál L et al (2023) The importance of chest CT severity score and lung CT patterns in risk assessment in COVID-19-associated pneumonia: a comparative study. Front Med (Lausanne). 10:1125530
Ndabahweje DN, Mukuku O, Kahindo CK et al (2024) Prediction of mortality in adult COVID-19 patients using chest CT severity scoring systems: a comparative analysis of different scores. Adv Gen Pract Med 5(1):81–89
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
TM, MB, and ME-b contributed in data collection, image revision, and final editing. H and H, share in data collection and editing. E-B, G, and MG, revision. All authors have read and approved the research and agree for the submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was done after approval from the Al-Azhar University Hospital — Faculty of Medicine Assiut and after patient agrees verbal consent (as the patients not exposed to any type of surgical or intervention maneuver). The committee’s reference number is as follows: the number of meeting code is 237, and the number of paper code is 4.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohammed, H.A.EM., Mansour, T.M.M., Abdalla, H. et al. Evaluation of MSCT severity scoring for prediction of mortality among patients with COVID-19. Egypt J Bronchol 18, 34 (2024). https://doi.org/10.1186/s43168-024-00287-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00287-w