Abstract
Background
Patient-reported outcomes (PROs) are getting widely implemented, but little is known of the impact of applying PROs in specific cancer diagnoses. We report the results of a randomized controlled trial (RCT) of the active use of PROs in patients with locally advanced or metastatic bladder cancer (BC) undergoing medical oncological treatment (MOT) with focus on determining the clinical effects of using PROs during chemo- or immunotherapy compared to standard of care.
Methods
We recruited patients from four departments of oncology from 2019 to 2021. Inclusion criteria were locally advanced or metastatic BC, initiating chemo- or immunotherapy. Patients were randomized 1:1 between answering selected PRO-CTCAE questions electronically once weekly with a built-in alert-algorithm instructing patients of how to handle reported symptoms as a supplement to standard of care for handling of side effects (intervention arm (IA)) vs standard procedure for handling of side effects (control arm (CA)). No real-time alerts were sent to the clinic when PROs exceeded threshold values. Clinicians were prompted to view the completed PROs in the IA at each clinical visit. The co-primary clinical endpoints were hospital admissions and treatment completion rate. Secondary endpoints were overall survival (OS), quality of life (EORTC’s QLQ-C30 and QLQ-BLM30) and dose reductions.
Results
228 patients with BC were included, 76% were male. 141 (62%) of the patients had metastatic disease. 51% of patients in the IA completed treatment vs. 56% of patients in the CA, OR 0.83 (95% CI 0.47–1.44, p = 0.51). 41% of patients in the IA experienced hospitalization vs. 32% in the CA, OR 1.48 (95% CI 0.83–2.65, p = 0.17). OS was comparable between the two arms (IA: median 22.3mo (95% CI 17.0-NR) vs. CA: median 23.1mo (95% CI 17.7-NR). Patient and clinician compliance was high throughout the study period (80% vs 94%).
Conclusions
This RCT did not show an effect of PRO on completion of treatment, hospitalizations or OS for BC patients during MOT despite a high level of patient and clinician compliance. The lack of real-time response to alerts remains the greatest limitation to this study.
Similar content being viewed by others
Introduction
Bladder cancer (BC) patients with advanced stages of disease have a poor prognosis [1, 2]. Only few oncological treatment possibilities exist and due to comorbidities, many patients are unfit for one or more of these treatment options [3,4,5]. From previous studies we have shown a high rate of hospital admissions and low rate of treatment completion for this patient group [6]. These poor clinical outcomes may to some extent be preventable, with the right intervention. One such intervention has over the past years been proposed to be the use of symptom questionnaires, patient-reported outcomes (PROs). The effect of real-time use of PROs to ensure timely handling of severe symptoms while in active oncological treatment has been tested in many settings with real-time responses and handling of symptoms either by the patients themselves or through added supportive care provided by study personnel [7,8,9]. For these purposes electronic PROs (ePROs) have been introduced to ensure completion of symptom questionnaires from home. Two studies by Denis and Basch testing the effect of the active use of PROs in different cancer populations on overall survival have shown an improved overall survival (OS) of 5–7 months compared to standard of care handling of symptoms and side-effects [10,11,12]. These data are of special interest to the BC population as a survival benefit of 5–7 months would markedly surpass the improvement in overall survival of 2–3 months seen for previously introduced 2nd line treatments [13]. However, PROs themselves have little or no clinical implications if not handled upon. Sole collection of PROs provides no direct benefit to the patient him- or herself [14]. Thus, the PROs must be used actively and generate a handling from either the patient herself or study personnel in order to secure the enhanced supported care. Also, the chosen PROs must be appropriate for the population and context to which they are applied [15,16,17,18]. We previously performed item selection specific to this group with the present study and endpoint in mind and found 15 appropriate symptoms explored by 30 items relevant for the present study [19]. Also, we tested the feasibility of ePRO use in the BC population and found a high questionnaire completion rate, even in this elderly and comorbid patient population [20].
In this study we report the effect of weekly ePROs as an intervention compared to standard of care for BC patients receiving chemo- or immunotherapy with the aim of reducing rate of hospital admissions during treatment and prevent early treatment cessation.
Methods
Patients
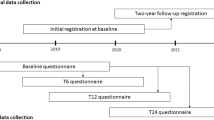
From 15th of January 2019 all patients with urothelial carcinoma of the bladder initiating chemo- or immunotherapy (cisplatin/gemcitabine, carboplatin/gemcitabine, pembrolizumab or vinflunin) as neoadjuvant treatment for muscle-invasive or locally advanced BC (from here on referred to as locally advanced BC) or palliative treatment for metastatic BC at the oncological department of four university hospitals (Copenhagen University Hospitals Rigshospitalet and Herlev Hospital, Aalborg University Hospital and Odense University Hospital) were asked to participate, please see Fig. 1. Further inclusion criteria were access to electronic communication with authorities through e-Boks™ as described in detail in a previous publication [20] and able to read Danish. Recruitment continued until 230 patients were enrolled.
Study overview. Abbreviations: PRO-CTCAE: Patient Reported Outcomes version of the Common Terminology Criteria for Adverse Events. QLQ-C30: European Organisation for Research and Treatment of Cancers global quality of life core questionnaire. QLQ-BLM30: European Organisation for Research and Treatment of Cancers questionnaire for muscle-invasive bladder cancer. Randomization allocation was provided by the Ambuflex software
Treatments (chemo- or immunotherapy) were for all patients given every three weeks in an out-patient setting. As part of enrollment into the study patients were asked to complete questionnaires (see below) for a maximum of six cycles of treatment [18 weeks]. Irrespective of allocated arm of randomization all patients could at any time contact their treatment department from home with troublesome symptoms.
The co-primary clinical endpoints were hospital admissions and treatment completion rate. Secondary endpoints were OS, quality of life (QoL) (EORTC’s QLQ-C30 and QLQ-BLM30) and dose reductions.
The intervention arm
If allocated to the intervention arm (IA) patients received the first questionnaire the same day as initiating treatment by receiving an email in Denmark’s electronic platform for communication with authorities, e-Boks™. Ambuflex, a generic web-based PRO software developed in 2004 in Denmark, sends questionnaires to a patient through e-Boks™, with a link for the patient with the specific questionnaire [20, 21]. The frequency of questionnaires and interval between treatment cycles and accompanying clinical visits follows a fixed interval, as shown in Table 1.
If patients failed to complete the questionnaires a reminder was sent after two days.
During completion of the 15 PRO-CTCAE symptoms the patient was guided on-screen of how to handle the given symptom if the severity exceeded a predefined level of severity. The alert appeared as shown below in a blue box next to the question:
Symptoms were selected specifically for patients in chemo- or immunotherapy for urothelial cancer. The comprehensive process of selection is described in detail in a previous publication [19].
For all PRO-CTCAE items, alerts were prompted to the patient at a level of severity at which the study group (GT, HL, HP) agreed that the symptom in question should be handled, either by the patients themselves or by the treating department, Table 2. A predefined level of severity was defined to colour the ‘bars’ in the clinician view of the Ambuflex system reflecting the severity of the response, Table 2.
For patients in the IA the treating clinician were at all following clinical visits reminded of responses in the Ambuflex system (Fig. 2) and could use this information in the conversation and treatment of the patient. As such, while the patients in the intervention arm completed questionnaires weekly, the clinicians were only prompted to view the development of the symptoms in Fig. 2 at clinical visits planned for every third week according to treatment cycles. No real-time alerts were sent to the clinic when PROs exceeded threshold values. Patients were thus expected to act upon the on-screen alerts, as illustrated in Fig. 3 and Table 2.
In response to the PROs, the clinician was not given a predefined course of action depending on the symptom and severity thereof. It was at the discretion of the clinician to use these data as he or she saw fit.
In order to evaluate the use of the above-described intervention in the daily clinic, we aimed to estimate the percentage of clinical visits in which the questionnaire was viewed by a clinician. We reviewed all clinician logs into Ambuflex coinciding with a completed questionnaire and divided the number by number of completed cycles of treatment for the IA.
The control arm
Patients assigned to the control arm (CA) followed standard procedure for handling of side effects and symptoms as informed by the treating department. The patients completed QoL questionnaires once every three weeks, as shown in Table 3. No on-screen alerts in response to these questionnaires were given and the clinicians were not, as in the IA, made aware of responses in Ambuflex when the patient came for clinical visits at the hospital. The completed questionnaires, although present in Ambuflex, were not presented to the clinician with coloured bars as in the IA.
Statistical analysis
On the basis of rates of treatment completion from a previous study and literature review, the current study was planned to include 230 patients. Prior data indicated that the rate of treatment cessation among controls was 50% [22,23,24] and data from our previous study indicated a treatment cessation rate of 54% [6]. If the true rate of treatment cessation for experimental subjects was 30% we would need 103 experimental subjects and 103 control subjects to be able to reject the null hypothesis that the failure rates for experimental and control subjects were equal with probability (power) 0.8. Allowing for expected attrition, 230 patients were planned for inclusion, 115 patients in each group. The type I error probability associated with this test of this null hypothesis was 0.05.
The proportion of patients experiencing early treatment cessation, hospitalization or dose reduction was compared between arms using Fisher’s exact test. OS was defined as time from inclusion in the study to death from any cause. The survival curves were calculated using the Kaplan–Meier estimator and compared between arms using the log-rank test. Median OS (mOS) was computed based on the estimated survival curves. The Cox proportional hazards model was used to estimate hazard ratios and corresponding 95% CIs. Variables with possible effect on survival were included in the analyses. Differences between arms in QoL was assessed using linear mixed effects models with time and group as fixed effects allowing for interaction, and patient as a random effect. Minimal important differences (MID) for interpreting EORTC QLQ-C30 were applied according to Musoro et al. and a MID of 10 point was applied in the interpretation of the results [25] The statistical analysis was carried out using R version 4.2.1 [26].
Ethical considerations
The study was approved by the Danish Data Protection Agency (suite nb: RH-2017–348), registered at www.clinicaltrials.gov with NCT03584659 and all patients completed written informed consent before entry into the study and randomisation. According to Danish law concerning sole questionnaire intervention studies at the time of study conduction, the study was exempt from approval from the National Committee on Health Research Ethics. The study was checked against the CONSORT Statement list of recommendations for randomized controlled trials with patient reported outcomes and the PRO extension, please see (Additional file 1: Table 1) [27].
Results
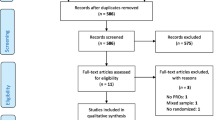
From 22nd January 2019 to 19th March 2021, we enrolled a total of 230 patients. Two patients were later excluded due to final pathology report requiring a different treatment than that of our inclusion criteria and another did not initiate treatment. The analysis therefore included 228 patients, Fig. 4.
The clinical data of the 228 patients are shown Table 4. The clinical characteristics of the patients were in concordance with other published studies of the bladder cancer cohorts and evenly dispersed between the two groups, with no significant differences [5, 28, 29]. Similar, no differences between groups are seen regarding stage of disease or systemic treatment modality. Median follow-up time from randomization to registration of death vs alive was 14.1 months.
We observed no difference in rate of hospital admissions (OR 1.48, 95% CI 0.83–2.65, p = 0.17) or completion of treatment (OR 0.83, 95% CI 0.47–1.44, p = 0.51) between the two groups, Table 5. Likewise, no difference in OS was found (mOS intervention arm: 22.3 months (95% CI 17.0-NA) vs. mOS control arm: 22.1 months (95% CI 17.7-NA)), p = 0.8, Table 5 and Fig. 5. Upper level of the confidence interval could not be computed due to too few deaths in the study period. When looking at OS with the clinical characteristics as covariates in a Cox proportional hazards model, only disease stage was found significant for survival (HR 4.91 (95% CI 2.62–19, p < 0.0001), Table 6. No difference in rate of dose reductions was observed between the two study arms; 19% vs 17%, OR 1.21 (95% CI 0.58–2.55, p = 0.61).
Global QoL for all patients was stable over time (Mean Global QoL 61–63 (SD: 22–26)). At the end of the study period global QoL increased for the intervention arm while the control arm experienced a decrease in QoL, although this difference was not statistically significant, Table 7 and Fig. 6. When looking at the subscales of QoL the data showed a highly significant and clinically meaningful difference in emotional functioning between the intervention and control arm favouring the intervention arm (Point estimate at week 18 = 13.6, p = 0.0001) [25]. No differences between arms were found for the remaining QoL subscales, Fig. 7.
Completion rate of electronic questionnaire for all patients was 69–88% through the course of 0–18 weeks with the highest completion rate (88.6%) at week 0. The completion differed between the two groups, as illustrated by Fig. 8. Completion rate declined steadily over time for patients in the control arm whereas completion for patients in the intervention arm remained at a stable level throughout treatment but repeatedly declined every third week coinciding with the longer questionnaire (EORTC QLQ-C30, QLQ-BLM30 and PRO-CTCAE) whereas completion remained above 80% for the short questionnaires (PRO-CTCAE).
The level of clinician compliance was determined by number of logs into the Ambuflex system coinciding with a completed questionnaire and compared with number of planned visits (as expected according to number of completed cycles of treatment). We found that the intervention group had a total of 495 completed cycles of treatment. The number of clinician logs into Ambuflex for the intervention group was 466, equaling a clinician compliance of 94%. However, against the intention of the study, we also found a clinician log into Ambuflex for the control group of 240. The control group had a total of 467 completed cycles equaling an unintended clinician log into Ambuflex (which did not show any listing of EORTC or PRO-CTCAE data) of 51%.
Discussion
In this multicenter randomized trial testing the active use of PROs during systemic oncological treatment for BC patients, we found a high rate of completed questionnaires and a high rate of clinician viewing of the patient-reported symptoms. For the primary endpoints, no statistically significant differences were found, although a higher rate of hospital admissions and lower rate of treatment completion was found in the IA. During the study period, global QoL increased for the IA and decreased for the CA, however these finding were not statistically significant. Emotional functioning was significantly higher for the IA. No differences were found in OS between the two study arms.
Unlike previously reported PRO trials testing the impact of systematic symptom reporting and enhanced handling of side effects, our study was unable to demonstrate differences in the chosen endpoints. Many explanations for this may exist. A major difference between ours and previous studies testing the use of PRO for cancer patients in treatment is that previously reported studies have implemented study staff to, on a daily basis, react upon alarming symptoms reported from home and then contacting the patient to initiate the appropriate supported care [11, 22, 30, 31]. Specifically, in a study by Maguire et al., alarming symptoms required study personnel attention within 30 min to 8 h. Hospital clinicians received these alerts on dedicated handsets and a predefined algorithm of how to handle a given symptom guided the clinical staff of how to handle the symptom in collaboration with the patient at home [30]. In the present study we relied on the patient following the on-screen instructions when exceeding a certain limit, as defined in Table 2. This patient-led strategy has been described effective for enhancing physical well-being and self-efficacy in the eRAPID study conducted in a health care system similar to the Danish health care system [32]. Low health literacy and/or unclear instructions for engaging the patients in the self-efficacy needed to act upon guidance shown on-screen may cause low impact of the tested intervention [33, 34], although health literacy in Denmark generally is perceived high compared to other European countries [35]. Insufficient training of the patients prior to PRO completion from home may also have affected our results. Recently, a study by Mooney et al. showed the importance of multicomponent interventions highlighting the importance of all components of PRO handling and interventions, thus showing lower effect on symptom relief with fewer interventional components [36]. Therefore, we may have missed opportunities to show significant effects in the chosen endpoints by solely relying on the patient to act upon alerts presented while PRO reporting from home.
In this study we found a mean questionnaire completion rate of 80% through the study period which is at level with previously conducted PRO studies [37–39]. This high compliance would along with the improved emotional functioning seen for the intervention group be assumed sufficient to enable engagement with the treating clinician at every clinical visit and support the self-efficacy needed to act upon on-screen guidance when prompted to do so as a result of a given symptom exceeding the predefined threshold [7, 30, 40]. The negative findings could therefore pinpoint the necessity of daily study personnel to support the intervention.
Clinician reluctance to the use of PROs and the importance of clinician endorsement to achieve effects of PRO have been described in several previous publications [41–43]. We found very high clinician compliance (94%) for the IA which explains the continuously high completion rate for the patients as seen for the IA in Fig. 8. However, we also saw clinician logs into the Ambuflex system for the CA of 51%, although no PRO data could be found as seen in Fig. 2 for the IA. Our inability to demonstrate a difference between the two study arms may therefore be a so-called spillover effect of the intervention to the control group [44]. Thus, the enhanced awareness on symptoms during treatment for both groups may have clouded for the actual impact in the intervention group by bringing enhanced symptom handling to both groups, unintentionally.
Although not statistically significant, we found a higher rate of hospitalizations and lower rate of treatment completion in the intervention group when compared with the control group. Though unintentional to the initial hypothesis and aim of the study, the enhanced focus on symptom handling and toxicity may have led to an increase in hospitalizations and earlier treatment cessations. In a previous study in the breast cancer population increased awareness to toxicity was previously described to lead to early treatment cessation [45]. However, in the study by Basch et al. from 2017, fewer hospitalizations were seen for the patients in the intervention arm, although this population of patients only comprised patients in treatment with chemotherapy [22]. The introduction of immunotherapy has led to the introduction of worldwide toxicity algorithms guiding clinicians to handle toxicities to treatments alike despite different hospital settings [46]. These pre-defined algorithms for toxicity handling may over time and during our study period have enhanced attention to side effects thus minimizing the potential benefit aimed for according to our power calculations performed with data from the pre-immunotherapy era. The PRO-TECT study by Basch et al. from 2022 included patients receiving immunotherapy and demonstrated a significant effect on symptom control and HRQOL with similar effect sizes as our study but did not report the impact on hospitalizations or treatment adherence. The PRO-TECT study was in addition to patient self-management advice planned with alerts to clinical staff on a daily basis and may explain the differences in our findings [31, 36].
Despite a small increase in global quality of life was observed for the intervention group compared to the control group we did not find a statistically significant difference between the two groups. However, a randomized study with an ePRO intervention in a population of metastatic melanoma patients showed that quality of life between the two arms did not separate until months after the applied ePRO intervention [47]. In the present study, we did not measure quality of life after patients had ended treatment, mainly of ethical reasons as patients who ceased treatment often did so due to troublesome symptoms, hospitalization or progressive disease and death. Had the patients who completed 6 cycles of treatment continued QoL reporting we may have found a clinically meaningful and statistically significant difference post-intervention.
Strengths of the study include the randomized trial design conducted at four university hospitals across Denmark. Also, the extensive pilot studies leading to this design, in terms of choice of endpoints and item selection process involving patients, nurses, physicians and review of literature is a major strength of this study. The conduction of the pilot studies spread over 1½ year allowing for familiarity with PROs as a part of daily clinic was in this study reflected in the high level of clinician compliance.
The lack of multicomponent handling of PROs exceeding threshold values to clinicians to allow for real-time handling of symptoms remains the greatest limitation in terms of not reaching the specified endpoints. Also, a limitation of the study may have been that no standard procedures were given to clinicians of how to handle a given side effect as reported by the patient in the ePROs. The study was planned as such to allow for individual physician-led treatment of a given side effect. However, there may at one or more sites have been a high clinical standard of handling of side effects before study initiation, thereby diminishing the impact of the intervention. The lack of this guidance specific to this study may across four study sites have led to vast differences in the handling of side effects for both arms in the study. In a study by Maguire et al. from 2021 they achieved improvements in anxiety, health related quality of life, self-efficacy and supportive care needs in the intervention group despite the multinational setup and may be explained by their extensive symptom management flow charts [30]. We did not track clinician response to troublesome PROs as a result of the clinical visit and viewing of PROs and thus we do not know whether this component of our intervention had the intended effect on symptom handling.
Conclusions
Conclusively, we did not find ePROs effective for the bladder cancer patients in relation to the chosen endpoints. We observed a high level of clinician engagement in using the ePROs and a positive impact on patients’ emotional functioning. Our study demonstrates the caveats in applying PROs across patient groups as a result of the increased awareness to PROs over the past years. For the bladder cancer patients with limited resources this approach may be unnecessarily time consuming in what sparse time left. The study group continues to evaluate the collected PRO data in order to find subsets of symptoms indicative for one or more of the chosen endpoints. Thus, further analyses will be made with the overall aim of improving the clinical courses of patients with bladder cancer.
Availability of data and materials
The data that support the findings of this study are available from Gry Assam Taarnhøj but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Gry Assam Taarnhøj.
Abbreviations
- BC:
-
Bladder cancer
- CA:
-
Control arm
- CI:
-
Confidence interval
- EORTC:
-
European Organisation for Research and Treatment of Cancer
- ePRO:
-
Electronic patient-reported outcomes
- HR:
-
Hazard ratio
- IA:
-
Intervention arm
- MOT:
-
Medical oncological treatment
- mOS:
-
Median overall survival
- OS:
-
Overall survival
- PRO:
-
Patient-reported outcome
- PRO-CTCAE:
-
Patient-reported outcomes version of the common terminology criteria for adverse events
- QLQ-BLM30:
-
EORTCs quality of life module for invasive bladder cancer
- QLQ-C30:
-
EORTCs general core quality of life module
- QoL:
-
Quality of life
- RCT:
-
Randomized controlled trial
- SD:
-
Standard deviation
References
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM et al (2019) Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 69(5):363–385. https://doi.org/10.3322/caac.21565
von der Maase H, Hansen SW, Roberts JT, Dogliotti L, Oliver T, Moore MJ et al (2000) Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicentre, Phase III Study. J Clin Oncol 18(17):3068–3077. https://doi.org/10.1200/jco.2000.18.17.3068
Laurent M, Brureau L, El Demery M, Fléchon A, Le Thuaut A, Carvahlo-Verlinde M et al (2017) Early chemotherapy discontinuation and mortality in older patients with metastatic bladder cancer: the AGEVIM multicenter cohort study. Urol Oncol Semin Orig Investig 35(1):34.e9-34.e16. https://doi.org/10.1016/j.urolonc.2016.08.003
Guancial EA, Roussel B, Bergsma DP, Bylund KC, Sahasrabudhe D, Messing E et al (2015) Bladder cancer in the elderly patient: challenges and solutions. Clin Interv Aging 10:939–949
Galsky MD, Hahn NM, Rosenberg J, Sonpavde G, Hutson T, Oh WK et al (2011) A consensus definition of patients with metastatic urothelial carcinoma who are unfit for cisplatin-based chemotherapy. Lancet Oncol 12(3):211–214. https://doi.org/10.1016/s1470-2045(10)70275-8
Taarnhøj GA, Lindberg H, Johansen C, Pappot H (2021) Patient-reported outcomes, health-related quality of life, and clinical outcomes for urothelial cancer patients receiving chemo- or immunotherapy: a real-life experience. J Clin Med 10(9):1852
Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM et al (2004) Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol 22(4):714–724. https://doi.org/10.1200/jco.2004.06.078
Mooney KH, Beck SL, Wong B, Dunson W, Wujcik D, Whisenant M et al (2017) Automated home monitoring and management of patient-reported symptoms during chemotherapy: results of the symptom care at home RCT. Cancer Med 6(3):537–546
Absolom K, Holch P, Warrington L, Samy F, Hulme C, Hewison J et al (2017) Electronic patient self-reporting of adverse-events: patient information and aDvice (eRAPID): a randomised controlled trial in systemic cancer treatment. BMC Cancer 17(1):318
Basch E, Deal AM, Dueck AC, Scher HI, Kris MG, Hudis C et al (2017) Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 318(2):197–198
Denis F, Yossi S, Septans AL, Charron A, Voog E, Dupuis O et al (2017) Improving survival in patients treated for a lung cancer using self-evaluated symptoms reported through a web application. Am J Clin Oncol 40(5):464–469. https://doi.org/10.1097/coc.0000000000000189
Denis F, Basch E, Septans AL, Bennouna J, Urban T, Dueck AC et al (2019) Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer. JAMA 321(3):306–307
Bellmunt J, Théodore C, Demkov T, Komyakov B, Sengelov L, Daugaard G et al (2009) Phase III trial of vinflunine plus best supportive care compared with best supportive care alone after a platinum-containing regimen in patients with advanced transitional cell carcinoma of the urothelial tract. J Clin Oncol 27(27):4454–4461. https://doi.org/10.1200/jco.2008.20.5534
Mooney K, Berry DL, Whisenant M, Sjoberg D (2017) Improving cancer care through the patient experience: how to use patient-reported outcomes in clinical practice. Am Soc Clin Oncol Educ Book 37:695–704. https://doi.org/10.1200/edbk_175418
Basch E, Abernethy AP, Mullins CD, Reeve BB, Lou SM, Coons SJ et al (2012) Recommendations for incorporating patient-reported outcomes into clinical comparative effectiveness research in adult oncology. J Clin Oncol 30(34):4249–4255. https://doi.org/10.1200/jco.2012.42.5967
Nissen A, Bager L, Pappot H (2019) The use of PRO in adverse event identification during cancer therapy—choosing the right questions to ask. Acta Oncol (Madr) 58(5):596–602. https://doi.org/10.1080/0284186x.2018.1560496
Lohr KN, Zebrack BJ (2008) Using patient-reported outcomes in clinical practice: challenges and opportunities. Qual Life Res 18(1):99–107. https://doi.org/10.1007/s11136-008-9413-7
Snyder CF, Aaronson NK, Choucair AK, Elliott TE, Greenhalgh J, Halyard MY et al (2011) Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual Life Res 21(8):1305–1314. https://doi.org/10.1007/s11136-011-0054-x
Taarnhøj GA, Lindberg H, Johansen C, Pappot H (2019) Patient-reported outcomes item selection for bladder cancer patients in chemo- or immunotherapy. J Patient Rep Outcomes 3(1):56
Taarnhøj GA, Lindberg H, Dohn LH, Omland LH, Hjøllund NH, Johansen C et al (2020) Electronic reporting of patient-reported outcomes in a fragile and comorbid population during cancer therapy—a feasibility study. Health Qual Life Outcomes 18(1):225
Hjollund NHI (2019) Fifteen years’ use of patient-reported outcome measures at the group and patient levels: trend analysis. J Med Internet Res 21(9):e15856–e15856
Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P et al (2016) Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol 34(6):557–565
Zauderer MG, Sima CS, Korc-Grodzicki B, Kris MG, Krug LM (2013) Toxicity of initial chemotherapy in older patients with lung cancers. J Geriatr Oncol 4(1):64–70
Maggiore RJ, Dale W, Gross CP, Feng T, Tew WP, Mohile SG et al (2014) Polypharmacy and potentially inappropriate medication use in older adults with cancer undergoing chemotherapy: effect on chemotherapy-related toxicity and hospitalization during treatment. J Am Geriatr Soc 62(8):1505–1512
Musoro JZ, Coens C, Sprangers MAG, Brandberg Y, Groenvold M, Flechtner HH et al (2023) Minimally important differences for interpreting EORTC QLQ-C30 change scores over time: A synthesis across 21 clinical trials involving nine different cancer types. Eur J Cancer 188:171–182
Team RC. A language and environment for statistical computing. Availabe online: https://www.R-project.org/ (accessed on
Calvert M, Blazeby J, Altman DG et al (2013) Reporting of patient-reported outcomes in randomized trials: The CONSORT PRO extension. JAMA 309(8):814–822. https://doi.org/10.1001/jama.2013.879
Bellmunt J, von der Maase H, Mead GM, Skoneczna I, De Santis M, Daugaard G et al (2012) Randomized phase III study comparing paclitaxel/cisplatin/gemcitabine and gemcitabine/cisplatin in patients with locally advanced or metastatic urothelial cancer without prior systemic therapy: EORTC Intergroup Study 30987. J Clin Oncol 30(10):1107–1113
Rosenberg JE, Hoffman-Censits J, Powles T, van der Heijden MS, Balar AV, Necchi A et al (2016) Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387(10031):1909–1920
Maguire R, McCann L, Kotronoulas G, Kearney N, Ream E, Armes J et al (2021) Real time remote symptom monitoring during chemotherapy for cancer: European multicentre randomised controlled trial (eSMART). BMJ 374:n1647–n1647
Basch E, Schrag D, Henson S, Jansen J, Ginos B, Stover AM et al (2022) Effect of electronic symptom monitoring on patient-reported outcomes among patients with metastatic cancer: a randomized clinical trial. JAMA 327(24):2413–2422
Absolom K, Warrington L, Hudson E, Hewison J, Morris C, Holch P et al (2021) Phase III randomized controlled trial of eRAPID: eHealth intervention during chemotherapy. J Clin Oncol 39(7):734–747. https://doi.org/10.1200/jco.20.02015
Sheeran P, Maki A, Montanaro E, Avishai-Yitshak A, Bryan A, Klein WMP et al (2016) The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol 35(11):1178–1188. https://doi.org/10.1037/hea0000387
Mackey LM, Doody C, Werner EL, Fullen B (2016) Self-management skills in chronic disease management. Med Decis Making 36(6):741–759. https://doi.org/10.1177/0272989x16638330
Tang Svendsen M, Kronborg Bak C, Sørensen K, Pelikan J, Juul Riddersholm S, Kuhr Skals R et al (2023) Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. https://doi.org/10.1186/s12889-020-08498-8
Mooney K, Gullatte M, Iacob E, Echeverria C, Brown K, Donaldson G (2022) A randomized control trial to determine necessary intervention elements to achieve optimal symptom outcomes for a remote symptom management system. J Clin Oncol 40(16_suppl):12008. https://doi.org/10.1200/JCO.2022.40.16_suppl.12008
Judson TJ, Bennett AV, Rogak LJ, Sit L, Barz A, Kris MG et al (2013) Feasibility of long-term patient self-reporting of toxicities from home via the Internet during routine chemotherapy. J Clin Oncol 31(20):2580–2585
Basch E, Artz D, Iasonos A, Speakman J, Shannon K, Lin K et al (2007) Evaluation of an online platform for cancer patient self-reporting of chemotherapy toxicities. J Am Med Inform Assoc 14(3):264–268
Benze G, Nauck F, Alt-Ep** B, Gianni G, Bauknecht T, Ettl J et al (2019) PROutine: a feasibility study assessing surveillance of electronic patient reported outcomes and adherence via smartphone app in advanced cancer. Ann Palliat Med 8(2):104–111. https://doi.org/10.21037/apm.2017.07.05
Ruland CM, Andersen T, Jeneson A, Moore S, Grimsbø GH, Børøsund E et al (2013) Effects of an internet support system to assist cancer patients in reducing symptom distress. Cancer Nurs 36(1):6–17. https://doi.org/10.1097/ncc.0b013e31824d90d4
Nordan L, Blanchfield L, Niazi S, Sattar J, Coakes CE, Uitti R et al (2018) Implementing electronic patient-reported outcomes measurements: challenges and success factors. BMJ Qual Saf 27(10):852–856. https://doi.org/10.1136/bmjqs-2018-008426
Yang LY, Manhas DS, Howard AF, Olson RA (2017) Patient-reported outcome use in oncology: a systematic review of the impact on patient-clinician communication. Support Care Cancer 26(1):41–60. https://doi.org/10.1007/s00520-017-3865-7
Calvert M, Kyte D, Price G, Valderas JM, Hjollund NH (2019) Maximising the impact of patient reported outcome assessment for patients and society. BMJ. https://doi.org/10.1136/bmj.k5267
Crawford FW, Morozova O, Buchanan AL, Spiegelman D (2019) Interpretation of the individual effect under treatment spillover. Am J Epidemiol 188(8):1407–1409
Baeksted CW, Nissen A, Knoop A, Christiansen M, Pappot H (2019) Handling of symptomatic adverse events in breast cancer patients receiving adjuvant chemotherapy in a cluster randomized trial with electronic patient-reported outcomes as intervention. Breast J 25(6):1295–1296. https://doi.org/10.1111/tbj.13477
Puzanov I, Diab A, Abdallah K, Bingham CO 3rd, Brogdon C, Dadu R et al (2017) Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer 5(1):95
Tolstrup LK, Pappot H, Bastholt L, Möller S, Dieperink KB (2022) Impact of patient-reported outcomes on symptom monitoring during treatment with checkpoint inhibitors: health-related quality of life among melanoma patients in a randomized controlled trial. J Patient Rep Outcomes 6(1):8
Acknowledgements
A special thanks to all the patients participating in this randomized study and all prior studies leading up to the current. Also, endless appreciation to the clinical and study staff at all four hospital sites throughout the study period.
Funding
Open access funding provided by Royal Library, Copenhagen University Library Danish Cancer Society, Dagmar Marshalls Fond, Einar Willumsens Mindelegat, A.P. Møller Lægefonden, Christian Larsen og Dommer Ellen Larsens Legat, Rigshospitalets Fond til støtte for onkologiske formal, Onkologisk Forskningsfond and Rigshospitalets Jubilæumsfond. None of the funding sources played a role in the planning, conduction of the study, analyses of the data or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
GAT: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Validation; Visualization; Roles/Writing – original draft; Writing – review & editing. CJ: Conceptualization; Funding acquisition; Methodology; Resources; Supervision; Writing – review & editing. AC: Data curation; Investigation; Project administration; Writing – review & editing. RHD: Data curation; Investigation; Project administration; Writing – review & editing. L.H. Dohn Data curation; Investigation; Writing – review & editing. NHH: Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Software; Writing – review & editing. MBK: Data curation; Formal analysis; Methodology; Validation; Visualization; Roles/Writing – original draft; Writing – review & editing. AT: Data curation; Formal analysis; Methodology; Validation; Visualization; Roles/Writing – original draft; Writing – review & editing. HL: Conceptualization; Data curation; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Writing – review & editing. HP: Conceptualization; Data curation; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Roles/Writing – original draft; Writing – review & editing. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Danish Data Protection Agency (suite nb: RH-2017–348), registered at www.clinicaltrials.gov with NCT03584659 and all patients completed written informed consent before entry into the study and randomisation. According to Danish law concerning sole questionnaire intervention studies at the time of study conduction, the study was exempt from approval from the National Committee on Health Research Ethics.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Information for reporting randomized controlled trials with patient reported outcomes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Taarnhøj, G.A., Johansen, C., Carus, A. et al. The iBLAD study: patient-reported outcomes in bladder cancer during oncological treatment: a multicenter national randomized controlled trial. J Patient Rep Outcomes 7, 99 (2023). https://doi.org/10.1186/s41687-023-00640-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-023-00640-5