Abstract
Background
Obstructive Sleep Apnea (OSA) is one of the diseases related to diabetes. Considering the varying prevalence of OSA in patients with type 2 diabetes in different parts of the world, in order to aggregate the results and come to a general review about the topic mentioned, the current study performed a systematic review and meta-analysis of OSA in patients with type 2 diabetes.
Methods
In this study, the international databases (PubMed, Scopus, Web of science, and Cochran library) were searched without time limit using keywords diabetes, obstructive sleep apnea, and prevalence or epidemiology. Homogeneity was investigated among studies using Cochran Q test and I2 index. Given the heterogeneity of studies, random effect model was used to estimate the prevalence of OSA. Meta-regression was used to investigate the effect of quantitative variables on the prevalence of OSA. Comprehensive Meta-analysis (CMA) software was used for data analysis.
Results
Twenty studies were included in the meta-analysis. In these 19 studies, the total number of patients with type 2 diabetes was 10,754, with a mean age of 58.6 ± 4.1 years. Final estimation of OSA prevalence was calculated to be 56.0%. The results of meta-regression showed the prevalence of OSA increased with a rise in the mean age, the percentage of male sex, body mass index, and sample size.
Conclusion
Given the high prevalence of OSA in patients with type 2 diabetes, weight control can partly mitigate their problems and possibly reduce OSA prevalence.
Similar content being viewed by others
Introduction
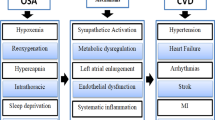
Type 2 diabetes is a chronic disease in which the body is unable to use and store glucose and instead of being converted into energy, glucose returns to the bloodstream and causes various symptoms (Srinivasan et al. 2018a). The prevalence of diabetes worldwide is estimated to be 4.6%, having a significantly increasing trend over the past two decades (Shaw et al. 2010). Moreover, the prevalence of type 2 diabetes in Iran has been reported to be 24%, indicating 4% annual increase over the past 20 years (Aamir et al. 2019). It is necessary to try to understand the factors associated with diabetes in order to prevent the increasing problems of these patients (Botros et al. 2009). Identification of potentially changeable risk factors for diabetes is still a clinical and public health priority (Nagayoshi et al. 2016). Obstructive Sleep Apnea (OSA) is one of the diseases related to diabetes; the two diseases are too common and both have common risk factors like obesity (Nannapaneni et al. 2013; Altaf et al. 2016; Mok et al. 2017).
There is a two-way relationship between OSA and diabetes; diabetes is one of the risk factor for OSA and OSA is a risk factor for diabetes (Jehan et al. 2018). The prevalence of OSA is different in independent studies. A study in China estimated the prevalence of type 2 diabetes to be 38.0% (Srinivasan et al. 2018b). This rate has been reported to be 86.0% in another study in the U.S (Foster et al. 2009). Further, in two independent studies in Iran, the prevalence rates of OSA in patients with type 2 diabetes has been reported to be 74.0 and 54.0% (Nasseri et al. 2015; Sadeghniiat-Haghighi et al. 2015). To the best of our knowledge, a meta-analysis study has not yet examined the prevalence of OSA in type 2 diabetic patients. So, due to differences in the prevalence of OSA in patients with type 2 diabetes, in order to summarize the results and gain an overview of the topic, the present study was aimed to carry out a systematic review and meta-analysis of the prevalence of OSA in patients with type 2 diabetes. The results of this study are hoped to be used by the healthcare policymakers.
Materials and methods
The present systematic review and meta-analysis investigated the prevalence of OSA in patients with diabetes based on the articles published in English journals without time limitation. In this study, the articles published in journals available in the international databases, including PubMed, Scopus, Web of Science, and Cochran library were used. The articles were searched using the keywords diabetes, obstructive sleep apnea, and prevalence or epidemiology. Searching strategies were as follows:
-
((diabetes [Title/Abstract]) AND “obstructive sleep apnea”[Title/Abstract] AND prevalence [Title/Abstract])
-
((diabetes [Title/Abstract]) AND “obstructive sleep apnea”[Title/Abstract] AND epidemiology [Title/ Abstract])
In order to reduce bias, the articles were searched independently by two researchers (the first and second authors), and in case of disagreement over a study, that article was judged by the supervisor of the research team (the fifth author). At first, all extracted articles were fed into the Endnote software and then the duplicate articles were deleted using the duplicate command. In the next step, the titles and abstracts of all papers were reviewed by the researchers and unrelated articles were removed. The remaining articles were evaluated based on the inclusion criteria using the STROBE checklist. The inclusion criteria were articles published until 27.9.2018 and being written in English and existence of title and keywords in the abstract. In these articles, the criteria for diagnosing OSA was apnea–hypopnea index ≥5 or a positive score in more than two categories of the Berlin questionnaire. Type 2 diabetic patients included those whose diagnosis had been confirmed and were treated with hypoglycemic drugs. The exclusion criteria were topics irrelevant to the subject matter, case reports, duplicate studies, uncertain method and sampling method, and lack of access to the full text of the studies. Data of the selected articles, such as title, first author’s name, year of publication, place of study, participants’ mean age, participants’ sex percentage, sample size, and number and percentage of patients with type 2 diabetes who had OSA were extracted and recorded. In addition, since a questionnaire was used in some studies to diagnose OSA and sleep monitoring devices were used in others, in order to investigate the effect of diagnostic method on the prevalence of OSA in patients with type 2 diabetes, the information about the diagnostic method was extracted and used to analyze the results in each study.
Article selection
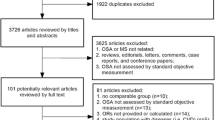
Searching the databases started on October 27, 2018 without time limitation. A total of 961 articles were extracted from the databases, 406, 89, 454, and 12 articles from PubMed, Cochran library, Scopus and Web of science, respectively. Of these, 341 articles were duplicate and were excluded. Of 620 articles, 569 articles were excluded because they were irrelevant to the research subject, so 51 articles remained for analysis (full text). Of these 51 full text articles, 9 articles were in non-English language. In 13 studies, target populations were diabetic patients at high risk and in 5 articles, patients with type 1 diabetes were examined. The content of one of the articles was repetitive and 2 articles examined the prevalence of diabetes in patients with OSA, so they were excluded from the study. Two other articles were also excluded because they used reading medical document method and the OSA diagnostic tool was not explained. The full text of all the studies included in the final stage was available. The Joanna Briggs Institute Prevalence Critical Appraisal Tool was used to evaluate the quality of these articles. This tool has 10 items and each item has four options including “yes, no, unspecified, and not applicable”. The yes option is awarded one point and the other options are awarded zero points. The rating range is between zero and 10 (Munn et al. 2014). Studies that scored equal to or higher than 5 were included in the current study. Eventually, 18 articles were included in the meta-analysis. Since two groups of Asian and European subjects were separately examined in one of the articles, the data were separately fed into the software; in fact, the data of 19 studies were fed into the software (Fig. 1).
Statistical analysis
Comprehensive Meta-analysis (CMA) software was used to analyze the data. The prevalence of OSA was extracted from the articles. Then, the variance of each study was determined by binomial distribution. Weighted mean was used to combine the prevalence of various studies. Each study was weighted proportional to its variance inverse. Heterogeneity between studies was reviewed using the heterogeneity test Cochran Q and I2 index. According to the heterogeneity of the studies, random effects model was used to estimate the prevalence. The impact of omission of each study was assessed by sensitivity analysis. To investigate the publication bias, the funnel plot and Begg and Mazumdar’s rank correlation test were used. To examine the effect of OSA evaluation tool on the prevalence, two groups of questionnaires and devices were compared. Meta-regression was also used to study the effect of quantitative variables, including age, year of study, sample size, body mass index, and gender percentage. All tests were performed with 95% confidence.
Results
Eighteen articles were included in the meta-analysis. According to the STROBE checklist, the articles included in the meta-analysis had good quality. Since one of the articles had been conducted on the Asian and European patients, its data were recorded in two separate studies; hence, 19 studies were analyzed. The total number of patients with type 2 diabetes in these 19 studies was 10,754, with a mean age of 58.6 ± 4.1 years. The highest and lowest prevalence rates of OSA were belonged to Israel (90.3%) and Saudi Arabia (15.2%), respectively (Donovan et al. 2017; Kalakattawi et al. 2017).
The OSA diagnostic tool was a questionnaire in eight studies, while it was a sleep monitoring device in 12 studies (Table 1). After initial calculations, the heterogeneity of the studies was significant based on the heterogeneity indices (Q = 1922.946 and I2 = 99.012) (P < 0.001). For this reason, the random effects model was used in all subsequent stages. The results of funnel plot and Begg and Mazumdar’s rank correlation test showed no publication bias (Fig. 2). The final estimate of the prevalence of OSA was calculated to be 56.0% (Fig. 3). In order to analyze the sensitivity, each study was excluded from the analysis and the final estimate of OSA prevalence was calculated, which had no significant effect.
Regarding the heterogeneity of the results of the studies, meta-regression models were used to find the influential factors (heterogeneity). The results showed the prevalence of OSA elevated significantly with an increase in the mean age in studies (p < 0.001). The results of meta-regression showed a statistically significant relationship between the prevalence of OSA and sample size, and that the prevalence of OSA increased with an increase in the sample size (p < 0.001). However, the year of study did not have a significant effect on the prevalence of OSA. Meta-regression was also used to examine the effect of sex percentage on the prevalence of OSA. The results showed the prevalence of OSA increased with a rise in the male percentage (p < 0.001). The results also revealed that with increasing BMI, the prevalence of OSA increased (P < 0.001). The graphs for meta-regression are shown in Fig. 4. The results showed that the prevalence of OSA in the studies using questionnaire was not significantly different from that of the sleep monitoring devices (Fig. 5).
Discussion
This systematic review and meta-analysis was aimed to determine the prevalence of OSA in patients with type 2 diabetes. The results showed that the total number of patients with type 2 diabetes in this study was 10,754, with a mean age of 58.6 ± 4.1 years. In our study, the final estimate of the prevalence of OSA was calculated to be 56.0%. The prevalence of OSA in patients with type 2 diabetes varied from country to country, ranging from 15.2 to 90.3% (Lam et al. 2010; Ozol et al. 2011; Shim et al. 2011; Tahrani et al. 2012; Burgess et al. 2013; Lecomte et al. 2013; Obaseki et al. 2014; Nasseri et al. 2015; Sadeghniiat-Haghighi et al. 2015; Vale et al. 2015; Zhang et al. 2015, 2016; Westlake et al. 2016; Amin et al. 2017; Donovan et al. 2017; Kalakattawi et al. 2017; Sokwalla et al. 2017; Viswanathan et al. 2017). The highest and lowest prevalence of OSA were related to Israel (90.3%) and Saudi Arabia (15.2%), respectively (Donovan et al. 2017; Kalakattawi et al. 2017). The prevalence of OSA in adults is estimated at 1 billion people worldwide, with a prevalence of more than 50.0% in some countries (Benjafield et al. 2019), which is much lower than the results of our study. In fact, our findings show that OSA is more common in people with type 2 diabetes than in non-diabetic group people.
The variables sample size, age, and gender were introduced as factors causing heterogeneity in the meta-regression analysis. Studies with a larger sample size were more prevalent. The prevalence of OSA also increased as the number of men rose in the studies. This relationship was also observed for age so that the prevalence of OSA increased significantly with an increase in mean age. Evidence suggests that age and male gender are the factors that increase the vulnerability of patients with OSA (Durán et al. 2001; Punjabi 2008). The results of a study in Saudi Arabia (2017) indicated that the risk of prevalence of OSA increased with an increase in the age of the diabetic patients (Kalakattawi et al. 2017). Another study in China (2015) showed that the chance of OSA prevalence elevated with an increase in the age of the diabetic patients (Zhang et al. 2015).
In our study, the results showed that with increasing BMI, the prevalence of OSA increases. This finding is consistent with previous studies (Schwab et al. 2003, JP, J 2014; Basoglu et al. 2015; Dong et al. 2020). Evidence suggests that obesity is a common cause of OSA and diabetes (Nannapaneni et al. 2013; Altaf et al. 2016). Lifestyle modification and weight control are vital factors, especially in the male patients with diabetes (Kline et al. 2011). Changing the lifestyle and performing routine exercises can help to prevent obesity and decrease the risk of OSA in patients with type 2 diabetes (Kline et al. 2011; Hargens et al. 2013; Miller et al. 2015).
In order to diagnose OSA, some studies used questionnaires, including STOP-BANG, The Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and BERLIN questionnaire and some other studies used devices such as Alice PDX, PSG, Apnealink, and night sleep monitors. The results showed no significant difference in the prevalence of OSA between studies using the questionnaire and those using sleep monitoring devices. According to Gantner et al. (2010), the accuracy of the BERLIN questionnaire was lower in OSA diagnosis than in PSG and Apnealink devices. Given the high prevalence of OSA in patients with type 2 diabetes and the cost-effectiveness of the questionnaire, diabetics can be tracked using a screening questionnaire and polysomnography in the first and second steps, respectively. With the early diagnosis of the diabetic patients’ problems, solutions and treatments for these patients can be considered (Gantner et al. 2010). Regarding the high prevalence of OSA in patients with type 2 diabetes and the presence of risk factors such as old age and male gender, it is important to take health and medical planning into account to decrease the prevalence of OSA.
This study faced three limitations. The first limitation was the lack of uniform distribution of studies in different parts of the world. Lack of information, such as the OSA report by gender, was the second limitation. The third limitation was the lack of search for gray resources due to lack of access.
Conclusion
The prevalence of OSA was estimated to be 56.0%. The results of meta-regression showed that the prevalence of OSA increased with an increase in the mean age, male gender percentage, BMI, and sample size. Since screening diabetic patients with OSA has not been performed in many parts of the world and there is no accurate information on the prevalence of OSA in patients with type 2 diabetes, it seems that more precise national planning is needed to screen the prevalence of OSA in the country and other parts of the world.
Availability of data and materials
The identified datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ESS:
-
Epworth Sleepiness Scale
- OSA:
-
Obstructive sleep apnea
- PSQI:
-
Pittsburgh Sleep Quality Index
References
Aamir AH, Ul-Haq Z, Mahar SA, Qureshi FM, Ahmad I, Jawa A, et al. Diabetes Prevalence Survey of Pakistan (DPS-PAK): prevalence of type 2 diabetes mellitus and prediabetes using HbA1c: a population-based survey from Pakistan. BMJ Open. 2019;9(2):e025300.
Altaf QA, Ali A, Piya MK, Raymond NT, Tahrani AA. The relationship between obstructive sleep apnea and intra-epidermal nerve fiber density, PARP activation and foot ulceration in patients with type 2 diabetes. J Diabetes Complicat. 2016;30(7):1315–20.
Amin A, Ali A, Altaf QA, Piya MK, Barnett AH, Raymond NT, et al. Prevalence and associations of obstructive sleep apnea in south Asians and white Europeans with type 2 diabetes: a cross-sectional study. J Clin Sleep Med. 2017;13(4):583–9.
Basoglu OK, Vardar R, Tasbakan MS, Ucar ZZ, Ayik S, Kose T, et al. Obstructive sleep apnea syndrome and gastroesophageal reflux disease: the importance of obesity and gender. Sleep Breath. 2015;19(2):585–92.
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–98.
Botros N, Concato J, Mohsenin V, Selim B, Doctor K, Yaggi HK. Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med. 2009;122(12):1122–7.
Burgess KR, Havryk A, Newton S, Tsai WH, Whitelaw WA. Targeted case finding for OSA within the primary care setting. J Clin Sleep Med. 2013;9(7):681–6.
Dong Z, Xu X, Wang C, Cartledge S, Maddison R, Islam SMS. Association of overweight and obesity with obstructive sleep apnoea: a systematic review and meta-analysis. Obes Med. 2020;17:100185.
Donovan LM, Rueschman M, Weng J, Basu N, Dudley KA, Bakker JP, et al. The effectiveness of an obstructive sleep apnea screening and treatment program in patients with type 2 diabetes. Diabetes Res Clin Pract. 2017;134:145–52.
Durán J, Esnaola S, Rubio R, Iztueta Á. Obstructive sleep apnea–hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163(3):685–9.
Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, et al. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009;32(6):1017–9.
Gantner D, Ge JY, Li LH, Antic N, Windler S, Wong K, et al. Diagnostic accuracy of a questionnaire and simple home monitoring device in detecting obstructive sleep apnoea in a Chinese population at high cardiovascular risk. Respirology. 2010;15(6):952–60.
Hargens TA, Kaleth AS, Edwards ES, Butner KL. Association between sleep disorders, obesity, and exercise: a review. Nat Sci Sleep. 2013;5:27.
Jehan S, Myers A, Zizi F. Obesity, obstructive sleep apnea, and type 2 diabetes mellitus: epidemiology and pathophysiologic insights. Sleep Med Dis Int J. 2018;2(3):54–60.
Kalakattawi RMN, Kalakattawi AMN, Alsuqati FA, Alzhrani SA, Alhamyani AH, Alhamyani AH, et al. Risk of obstructive sleep apnea assessment among patients with type 2 diabetes in Taif, Saudi Arabia. J Clin Med Res. 2017;9(12):1002–6.
Kline CE, Crowley EP, Ewing GB, Burch JB, Blair SN, Durstine JL, et al. The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep. 2011;34(12):1631–40.
Lam DCL, Lui MMS, Lam JCM, Ong LHY, Lam KSL, Ip MSM. Prevalence and recognition of obstructive sleep apnea in Chinese patients with type 2 diabetes mellitus. Chest. 2010;138(5):1101–7.
Lecomte P, Criniere L, Fagot-Campagna A, Druet C, Fuhrman C. Underdiagnosis of obstructive sleep apnoea syndrome in patients with type 2 diabetes in France: ENTRED 2007. Diabetes Metab. 2013;39(2):139–47.
Miller JD, Aronis KN, Chrispin J, Patil KD, Marine JE, Martin SS, et al. Obesity, exercise, obstructive sleep apnea, and modifiable atherosclerotic cardiovascular disease risk factors in atrial fibrillation. J Am Coll Cardiol. 2015;66(25):2899–906.
Mok Y, Tan CW, Wong HS, How CH, Tan KLA, Hsu PP. Obstructive sleep apnoea and type 2 diabetes mellitus: are they connected? Singap Med J. 2017;58(4):179.
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123.
Nagayoshi M, Punjabi NM, Selvin E, Pankow JS, Shahar E, Iso H, et al. Obstructive sleep apnea and incident type 2 diabetes. Sleep Med. 2016;25:156–61.
Nannapaneni S, Ramar K, Surani S. Effect of obstructive sleep apnea on type 2 diabetes mellitus: a comprehensive literature review. World J Diabetes. 2013;4(6):238.
Nasseri R, Malek M, Aghili R, Valojerdi AE, Khamseh ME. Disturbed sleep in type 2 diabetes mellitus independent of chronic complications, pain, and nocturia. Int J Diabetes Dev Ctries. 2015;35(4):454–9.
Obaseki DO, Kolawole BA, Gomerep SS, Obaseki JE, Abidoye IA, Ikem RT, et al. Prevalence and predictors of obstructive sleep apnea syndrome in a sample of patients with type 2 diabetes mellitus in Nigeria. Niger Med J. 2014;55(1):24–8.
Ozol D, CarlIoǧlu A, KaramanlI H, Akgedik R, Karakurt F, YildIrIm Z. Influence of snoring on microalbuminuria in diabetic patients. Sleep Breathing. 2011;15(3):295–300.
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–43.
Sadeghniiat-Haghighi K, Mohajeri-Tehrani MR, Khajeh-Mehrizi A, Fathi F, Saremi-Rasouli F, Ghajarzadeh M, et al. Obstructive sleep apnea and excessive daytime sleepiness among patients with type 2 diabetes mellitus: a single-center study from Iran. Int J Diabetes Dev Ctries. 2015;35:189–93.
Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R, et al. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med. 2003;168(5):522–30.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14.
Shim U, Lee H, Oh JY, Sung YA. Sleep disorder and cardiovascular risk factors among patients with type 2 diabetes mellitus. Korean J Intern Med. 2011;26(3):277–84.
Tahrani AA, Ali A, Raymond NT, Begum S, Dubb K, Mughal S, et al. Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med. 2012;186(5):434–41.
Vale J, Manuel P, Oliveira E, Oliveira AR, Silva E, Melo V, et al. Obstructive sleep apnea and diabetes mellitus. Rev Port Pneumol (2006). 2015;21(2):55–60.
Viswanathan V, Ramalingam IP, Ramakrishnan N. High prevalence of obstructive sleep apnea among people with type 2 diabetes mellitus in a tertiary care center. J Assoc Physicians India. 2017;65(11):38–42.
Westlake K, Plihalova A, Pretl M, Lattova Z, Polak J. Screening for obstructive sleep apnea syndrome in patients with type 2 diabetes mellitus: a prospective study on sensitivity of Berlin and STOP-Bang questionnaires. Sleep Med. 2016;26:71–6.
Zhang R, Guo X, Guo L, Lu J, Zhou X, Ji L. Prevalence and associated factors of obstructive sleep apnea in hospitalized patients with type 2 diabetes in Bei**g, China 2. J Diabetes. 2015;7(1):16–23.
Zhang P, Zhang R, Zhao F, Heeley E, Chai-Coetzer CL, Liu J, et al. The prevalence and characteristics of obstructive sleep apnea in hospitalized patients with type 2 diabetes in China. J Sleep Res. 2016;25(1):39–46.
JP J. The effect on plasma inflammatory markers of obstructive sleep apnea hypopnea syndrome in obese. Chin J Gen Pract. 2014;12(8):1341–3.
Sokwalla SMR, Joshi MD, Amayo EO, Acharya K, Mecha JO, Mutai KK. Quality of sleep and risk for obstructive sleep apnoea in ambulant individuals with type 2 diabetes mellitus at a tertiary referral hospital in Kenya: a cross-sectional, comparative study. BMC Endocr Disord. 2017;17(1):1–8.
Srinivasan K, Vaishnavi R, Sudhakar SS. Prevalence of obstructive sleep apnea in diabetes mellitus type 2. Int J Sci Res. 2018a;7(20).
Srinivasan K, Vaishnavi R, Sudhakar SS. Prevalence of obstructive sleep apnea in diabetes mellitus type 2. Int J Sci Res. 2018b;7(2).
Acknowledgements
We highly appreciate the Clinical Research Development Center of Imam Reza Hospital for kindly advices.
Funding
The study was funded by Kermanshah University of Medical Sciences (Grant No. 98454).
Author information
Authors and Affiliations
Contributions
BA, MJ, AK, AS, MJ and SMA contributed in designing the study, BA, SMA, and AK collected the data, and analyzed by BA. The final report and manuscript were written by BA, AK, AS, MJ and SMA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by research ethics committee of Kermanshah University of Medical Sciences.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Andayeshgar, B., Janatolmakan, M., Soroush, A. et al. The prevalence of obstructive sleep apnea in patients with type 2 diabetes: a systematic review and meta-analysis. Sleep Science Practice 6, 6 (2022). https://doi.org/10.1186/s41606-022-00074-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41606-022-00074-w