Abstract
Ischemic stroke (IS), a devastating cerebrovascular accident, presents with high mortality and morbidity. Following IS onset, a cascade of pathological changes, including excitotoxicity, inflammatory damage, and blood-brain barrier disruption, significantly impacts prognosis. However, current clinical practices struggle with early diagnosis and identifying these alterations. Metabolomics, a powerful tool in systems biology, offers a promising avenue for uncovering early diagnostic biomarkers for IS. By analyzing dynamic metabolic profiles, metabolomics can not only aid in identifying early IS biomarkers but also evaluate Traditional Chinese Medicine (TCM) efficacy and explore its mechanisms of action in IS treatment. Animal studies demonstrate that TCM interventions modulate specific metabolite levels, potentially reflecting their therapeutic effects. Identifying relevant metabolites in cerebral ischemia patients holds immense potential for early diagnosis and improved outcomes. This review focuses on recent metabolomic discoveries of potential early diagnostic biomarkers for IS. We explore variations in metabolites observed across different ages, genders, disease severity, and stages. Additionally, the review examines how specific TCM extracts influence IS development through metabolic changes, potentially revealing their mechanisms of action. Finally, we emphasize the importance of integrating metabolomics with other omics approaches for a comprehensive understanding of IS pathophysiology and TCM efficacy, paving the way for precision medicine in IS management.
Similar content being viewed by others
Introduction
Ischemic stroke (IS), a neurological disorder caused by stenosis or occlusion of cerebral artery, is a leading cause of chronic disability worldwide and a serious threat to human life [1]. In addition to vascular occlusion caused by major atherosclerosis, IS can also be caused by acute cerebral infarction with definite etiology such as cardiogenic embolism, arteriolar occlusion, infectious disease, non-immune vascular disease, hypercoagulable state, and cryptogenic stroke with unclear etiology. Among them, the middle cerebral artery is a common occluded blood vessel, while occlusion of the vertebrobasilar artery, posterior cerebral artery, and anterior cerebral artery is less frequent [2, 3]. In the United States alone, over 750,000 stroke cases occur annually, making it the fifth leading cause of death and the top cause of disability [4]. Globally, IS ranks second in mortality and first in disability, with a concerning rise in younger individuals experiencing the disease [5]. Strokes can be hemorrhagic or ischemic, with over 85% being ischemic due to interrupted blood flow to the brain, leading to irreversible cell damage [6]. Inflammatory response [7], autophagy [8], and cell apoptosis are the primary mechanisms underlying brain tissue damage in IS [9]. Treatment for IS patients depends on the time of onset, neurological deficits, and neuroimaging results [10]. Despite significant advancements in thrombolysis and mechanical thrombectomy over the past decade, IS remains a major contributor to global healthcare burden [11]. Recombinant human tissue plasminogen activator (rt-PA) is an established intervention for acute IS, with clinical studies demonstrating increasing usage since 2006, highlighting the effectiveness of intravenous thrombolytic therapy [12]. However, the therapeutic window for rt-PA is narrow, and its effectiveness is limited by slow reperfusion. Additionally, rt-PA carries a significant risk of bleeding, which is roughly 10 times higher than in patients who do not receive rt-PA. According to clinical data statistics, the incidence of bleeding transformation after thrombolytic therapy in acute IS patients ranges from 10 to 43%, with symptomatic intracranial hemorrhage occurring at a rate of 1.7–10.3% [13, 14]. This highlights the urgent need for new diagnostic tools and therapies, particularly for early IS detection. Metabolomics, with its ability to detect rapid changes in body metabolites during disease onset, holds immense potential for early diagnosis and improved treatment strategies for IS. This review explores the current research landscape of metabolomics in IS and summarizes its promising applications in clinical settings.
Overview of metabolomics
What is metabolomics
Metabolomics, an emerging field within systems biology and an extension of omics technologies like genomics, transcriptomics, and proteomics, has gained widespread application in life sciences due to rapid advancements in analytical techniques [15]. First proposed by Professor Nicholson in 1999 [16], metabolomics focuses on studying the metabolic product profiles and dynamic changes of organisms, tissues, or cells under different physiological and pathological stimuli [21]. Conversely, non-targeted metabolomics involves a comprehensive analysis of all measurable analytes (including unidentified metabolites) within a sample under given conditions, providing a more comprehensive picture and avoiding potential biases in research direction [22]. This method is often used for exploratory studies, analyzing metabolites without prior knowledge of their identities. Non-targeted metabolomics holds immense potential for a holistic approach in biomedical research, enabling the discovery of novel biomarkers through comparison with metabolomics libraries, ultimately improving disease diagnosis and understanding of underlying pathological mechanisms [23]. In clinical practice, biological samples for metabolomics analysis are primarily obtained from blood, urine, feces, cerebrospinal fluid, saliva, and tissues. The core objective lies in analyzing the relationships between metabolites and physiological/pathological changes within the body from these samples, ultimately aiming to reveal the pathogenesis of diseases at a holistic level [24]. As a relatively new research method, metabolomics offers several advantages, including ease of sample acquisition, simplified protein detection, minimal requirements for large-scale database construction, convenient data processing, and high detection efficiency. These attributes have contributed to the growing interest in this field in recent years.
Research methods and data analysis of metabolomics
The rapid development of metabolomics is inextricably linked to advancements in its technology. Liquid chromatography (LC) and gas chromatography (GC) are the most prevalent methods for metabolite separation, while metabolite detection primarily relies on nuclear magnetic resonance (NMR) and mass spectrometry (MS) [25]. In metabolomics analysis, LC and GC are often coupled with MS, whereas NMR typically functions as a standalone tool. These techniques have become the mainstream platform for identifying and quantifying metabolites [26]. The combination of high-performance separation chromatography with highly specific and sensitive mass spectrometry enables rapid metabolite identification and accurate quantitative analysis. GC-MS excels at analyzing thermally stable and volatile metabolites with minimal matrix effects from complex samples [27]. LC-MS, on the other hand, boasts broader analytical capabilities. It can be combined with diverse chromatographic columns and other conditions for analysis, enabling the separation and identification of a wider range of metabolites within the sample without extensive pre-treatment. Notably, its high sensitivity makes it ideal for analyzing thermally unstable, non-volatile, and higher molecular weight substances [28]. NMR offers several advantages, including fast analysis speed, high reproducibility, suitability for high-throughput analysis, non-destructive nature, minimal bias, and simple sample preparation. It can simultaneously detect multiple organic compounds, making it widely used in metabolomics analysis [29].
The primary analytical methods in metabolomics encompass univariate and multivariate analysis. Univariate analysis, characterized by its simplicity, intuitiveness, and ease of understanding, is commonly employed in metabolomics research to swiftly examine differences between metabolite categories. Due to the challenges of metabolomics data meeting the assumptions of parametric testing, non-parametric methods like the Wilcoxon rank sum test, Kruskal-Wallis test, and t-test are frequently used. Additionally, calculating fold changes in metabolite concentration between groups and the area under the ROC curve (AUC) are common practices. Multivariate analysis encompasses various techniques such as principal component analysis (PCA), partial least squares discriminant analysis (PLS-DA), orthogonal projection to latent structures (OPLS), and cluster analysis (CA). PCA leverages the relationships between original variables, transforming them into a set of independent, comprehensive indicators (principal components) based on maximizing variation. Typically, 2–3 principal components are plotted to visually depict differences in metabolic patterns and clustering between groups. Load plots are then used to identify original variables contributing to group classification as potential biomarkers [150]. They identified 26 differential metabolites, including γ-aminobutyric acid (GABA), lysine, and glutamate, which are involved in various processes such as inhibiting oxidative stress (Fig. 5) and promoting angiogenesis. The reversal of these changes by folic acid treatment suggests its potential for neuroprotection through multiple mechanisms.
Ma et al. investigated the mechanism of action of Edaravone (EDA), a medication used clinically for IS, despite an unclear mechanism [151]. Using metabolomic analysis of urine and serum samples, they found that EDA treatment normalized levels of metabolites involved in valine, leucine, isoleucine biosynthesis, and taurine metabolism. The most significant change was observed in taurine metabolism, with EDA increasing the activity of the enzyme cysteine sulfite decarboxylase, which inhibits endothelial cell apoptosis. These findings suggest that EDA may exert its neuroprotective effects by regulating taurine metabolism and endothelial cell function (Fig. 6).
Zhou et al. investigated the effects of Danshen Chuanxiongqin injection (DSCXQ) on IS in a rat model [152]. They observed that DSCXQ treatment modulated the levels of various metabolites, including those involved in lipid metabolism (L-tryptophan, LysoPC), sphingolipid metabolism (dihydrosphingosine 1-phosphate), and oxidative stress(Fig. 5) (indole-3-methylacetate). These findings suggest that DSCXQ exerts its neuroprotective effects through regulation of multiple metabolic pathways.
Hou et al. studied the mechanism of Duzhi Wan (DZW), a TCM formula used for IS prevention and treatment [153]. They identified complement C3 (C3) and C5a complement factor receptor 1 (C5ar1) as core targets of DZW, while also pinpointing key metabolites involved in its neuroprotective effects, such as acetylcholine and inosine 5’-monophosphate. In vivo studies showed that DZW reduced levels of inflammatory markers after IS treatment, suggesting that it exerts its effects by inhibiting neuroinflammation (Fig. 7).
Ye et al. investigated the mechanism of Dengzhan Shengmai capsule (DZSM), a TCM formula used for brain dysfunction [154]. They found that DZSM treatment significantly increased the concentration of 2-ketoglutarate, a metabolite involved in the citric acid cycle and glutamate metabolism. 2-ketoglutarate can be converted to glutamate, which can act as a neurotransmitter or be converted into an inhibitor of the NF-κB signaling pathway, an inflammatory pathway. These findings suggest that DZSM may exert neuroprotective and anti-inflammatory effects through the regulation of the citric acid cycle and glutamate metabolism (Fig. 7).
Outlook
Compared to other strokes, IS is characterized by high mortality and disability rates, which seriously affect the quality of life of patients, especially those with acute IS [155]. While advancements in treatment methods and clinical management have reduced the incidence and disability rates, they remain high [156]. Therefore, new methods for early diagnosis and prognosis of IS are crucial.
Metabolomics has been applied to IS research for over a decade. Initial research focused on blood metabolomic changes during IS to identify potential biomarkers. However, these haven’t been widely used in clinical practice for diagnosis, progression assessment, or prognosis of IS. Cerebrospinal fluid (CSF) offers a better reflection of metabolic changes during IS due to its proximity to the brain environment [157]. Identifying CSF biomarkers with high sensitivity and specificity for IS would be revolutionary for guiding clinical decisions, improving survival rates, and reducing disability. It would allow for accurate diagnosis of ongoing or imminent cerebral ischemia or infarction, and predict outcomes. Current limitations in biomarker research include insufficient sample size, and inconsistent effects of factors like age and gender on metabolites. Future efforts should focus on expanding research cohorts, standardizing analysis methods, develo** a wider range of cost-effective biomarkers for clinical decision-making, and acknowledging the need for multi-biomarker approaches due to the heterogeneity of stroke [158].
While metabolomics has revealed various metabolic changes in IS across age, gender, and severity, its application in understanding the pathogenesis of IS remains limited, partly due to high costs [159]. Prior research focused on downstream damage mechanisms like excitotoxicity [160], early inflammatory damage [161], oxidative stress response [162], immune response [163], and various forms of cell death [164]. This review proposes a bolder approach – linking metabolic changes to the mechanisms of post-IS damage. By doing so, metabolomics can reveal the pathogenesis of IS and deepen our understanding of the disease.
Another recent application of metabolomics in IS research is exploring drug targets for TCM. This approach shows promise in analyzing the material basis of TCM efficacy in IS and develo** new TCM drugs for the disease. The rapid development of emerging metabolomic technologies like stable isotope tracing metabolomics and mass spectrometry imaging space metabolomics will create new opportunities for IS diagnosis, TCM drug development, and a more comprehensive understanding of disease mechanisms [165]. Stable isotope tracing metabolomics can elucidate the role of metabolites in metabolic pathways, while mass spectrometry imaging space metabolomics allows for quantitative localization analysis of metabolites in large samples, both of which can provide valuable insights [166].
Limitations
Metabolomics is a high-throughput technology used to study the metabolic status of organisms. Although it has important application value in early disease diagnosis, drug development, and other aspects, it also has limitations [167]. Firstly, it requires processing a large amount of data, which can be time-consuming and requires skilled personnel [168]. Furthermore, standardization across various aspects of metabolomics techniques, including sample collection, quality control, and data analysis, is crucial to enhance the data’s credibility and comparability. This will require addressing current limitations in these areas.
IS is a complex multifactorial disease. In this article, we mainly review the potential pathogenesis of metabolic factors in IS. However, factors such as oxidative stress, apoptosis, pyroptosis, and inflammatory damage are also important contributors to post-IS brain injury. Additionally, research on other omics technologies [169], such as transcriptomics (gene expression), proteomics (protein analysis), imaging omics, and single-cell sequencing are limited in studying IS progression, drug targets, and pharmacological mechanisms. Integrating metabolomics with these other approaches in future studies can provide a more comprehensive understanding of IS.
Conclusion
In conclusion, future studies on IS using metabolomics should consider integrating these new technologies with other omics approaches like transcriptomics and proteomics. This comprehensive and systematic analysis will enhance our understanding of the pathological mechanisms of IS and the efficacy mechanisms of TCM, ultimately promoting the development of precision medicine for IS.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AA:
-
Arachidonic acid
- ADMA:
-
Asymmetric dimethylarginine
- AIS:
-
Acute ischemic stroke
- AMP:
-
Adenosine monophosphate
- AMPAR:
-
Glutamate AMPA receptor
- AMPK:
-
Adenosine 5’-monophosphate (AMP)-activated protein kinase
- Ang2:
-
Angiopoietin 2
- ANPIS:
-
Acute non-progressive ischemic stroke
- APIS:
-
Acute progressive ischemic stroke
- AUC:
-
Area under the ROC curve
- Bax:
-
BCL2-Associated X
- Bcl-2:
-
B-cell lymphoma-2
- BMD:
-
Bai-Mi-Decoction
- CA:
-
Cluster analysis
- Cer:
-
Ceramide
- C1P:
-
Ceramide-1-phosphate
- Cre:
-
Creatine
- CSDA:
-
Cysteine sulfinic acid decarboxylase
- CSF:
-
Cerebrospinal fluid
- Cyt C:
-
Cytochrome C
- dBd:
-
3,4-dihydroxybenzaldehyde
- dGMP:
-
deoxyguanosine-5’-phosphate
- DG:
-
Diacylglycerol
- DGKZ:
-
Diglycerol kinase zeta
- DHA:
-
Docosahexaenoic acid
- DSCXQ:
-
Danshen Chuanxiongqin injection
- DZSM:
-
Dengzhan Shengmai capsule
- DZW:
-
Duzhi Wan
- EDA:
-
Edaravone
- EPA:
-
Eicosapentaenoic acid
- ESL:
-
Eleutherococcus senticosus (Rupr. & Maxim.) Maxim. leaves
- eNOS:
-
nitric oxide synthase
- GABA:
-
γ-aminobutyric acid
- GABAA:
-
γ- aminobutyric acid recepter
- GC:
-
Gas chromatography
- GlyR:
-
Glycine recepter
- GLS:
-
Glutaminase
- GLUT:
-
Glucose transporters
- G6P:
-
Glucose-6-phosphate
- G6PD:
-
Glucose-6-phosphate dehydrogenase
- GSH:
-
Glutathione
- GSH/GSSG:
-
Total glutathione/oxidized glutathione
- GSH-PX:
-
Glutathione peroxidase
- GSSG:
-
Glutathione disulfide
- H2O2 :
-
Harmful hydrogen peroxide
- HO-1:
-
Heme oxygenase-1
- IMP:
-
Inosine monophosphate
- IS:
-
Ischemic stroke
- LAA:
-
Large artery atherosclerosis
- LC:
-
Liquid chromatography
- LPA:
-
Lysophosphatidic acid
- LPC:
-
Lysophosphatidylcholine
- LPE:
-
Lysophosphatidylethanolamine
- LTC:
-
Longxue Tongluo Capsule
- LysoPCs:
-
Lysophosphatidylcholines
- LysoPEs:
-
Lysophosphatidylethanolamines
- MCAO:
-
Middle cerebral artery occlusion
- Mmp:
-
Mitochondrial membrane potential
- mPTP:
-
mitochondrial permeability transition pore
- MS:
-
Mass spectrometry
- NAA:
-
N-acetylaspartate
- NAD+ :
-
Nicotinamide adenine dinucleotide
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate hydrogen
- NMR:
-
Nuclear magnetic resonance
- NO:
-
Nitric oxide
- Nrf2:
-
Nuclear factor E2-related factor 2
- OGT:
-
O-GlcNAc transferase
- OPLS:
-
Orthogonal projection to latent structures
- PAF:
-
Platelet activating factor
- PAGln:
-
Phenylacetylglucosamine
- PCA:
-
Principal component analysis
- PC:
-
Phosphatidylcholine
- PCs:
-
Phosphatidylcholines
- PE:
-
Phosphatidylethanolamine
- PG:
-
Prostaglandin
- PHBA:
-
Para hydroxybenzaldehyde
- Pla:
-
3-phenyllactic acid
- PLA2:
-
Phospholipase A2
- PLCγ1:
-
Phospholipase Cγ1
- PLD1:
-
Phospholipase D1
- PLS-DA:
-
Partial least squares discriminant analysis
- PPARγ:
-
peroxisome proliferator-activated receptorγ
- PSD:
-
Post-Stroke Depression
- PUFAs:
-
Particularly ω-3 polyunsaturated fatty acids
- ROS:
-
Reactive oxygen species
- R5P:
-
Ribose-5-phosphate
- Ru5P:
-
Ribulose-5-phosphate
- rt-PA:
-
Recombinant human tissue plasminogen activator
- SAA1:
-
Serum amyloid protein A1
- SAO:
-
Small artery occlusion
- S1P:
-
Sphingosine-1 phosphate
- SMDA:
-
Symmetric dimethylarginine
- SM:
-
Sphingolipids
- SMase:
-
Sphingomyelinase
- SMs:
-
Sphingomyelins
- Sph:
-
Sphingosine
- Spns2:
-
Spinster 2
- T-AOC:
-
Total antioxidant capacity
- TCM:
-
Traditional Chinese medicine
- TNF-α:
-
Tumor necrosis factor-α
- UDP-Glcnac:
-
Uridine diphosphate N-acetylglucosamine
- UDCA:
-
Ursodeoxycholic acid
- VEGF:
-
Vascular endothelial growth factor
- 4-HHE:
-
4-hydroxy-2E-hexenal
- 6PG:
-
6-phosphogluconate
- β-HB:
-
β-hydroxybutyrate
References
Zhu H, Hu S, Li Y, et al. Interleukins and ischemic stroke. Front Immunol. 2022;13:828447. https://doi.org/10.3389/fimmu.2022.828447.
Salerno A, Strambo D, Nannoni S, Dunet V, Michel P. Patterns of ischemic posterior circulation strokes: a clinical, anatomical, and radiological review. Int J Stroke. 2022;17(7):714–22. https://doi.org/10.1177/17474930211046758.
Arboix A, García-Eroles L, Sellarés N, Raga A, Oliveres M, Massons J. Infarction in the territory of the anterior cerebral artery: clinical study of 51 patients. BMC Neurol. 2009;9(1):30. https://doi.org/10.1186/1471-2377-9-30.
Khandelwal P, Yavagal DR, Sacco RL. Acute ischemic stroke intervention. J Am Coll Cardiol. 2016;67(22):2631–44. https://doi.org/10.1016/j.jacc.2016.03.555.
Fang J, Wang Z, Miao C. Angiogenesis after ischemic stroke. Acta Pharmacol Sin. 2023;44(7):1305–21. https://doi.org/10.1038/s41401-023-01061-2.
Boncoraglio GB, Ranieri M, Bersano A, Parati EA, Del Giovane C. Stem cell transplantation for ischemic stroke. Cochrane Stroke Group. ed Cochrane Database Syst Reviews. 2019;2019(5). https://doi.org/10.1002/14651858.CD007231.pub3.
DeLong JH, Ohashi SN, O’Connor KC, Sansing LH. Inflammatory responses after ischemic stroke. Semin Immunopathol. 2022;44(5):625–48. https://doi.org/10.1007/s00281-022-00943-7.
Wang P, Shao BZ, Deng Z, Chen S, Yue Z, Miao CY. Autophagy in ischemic stroke. Prog Neurobiol. 2018;163–164:98–117. https://doi.org/10.1016/j.pneurobio.2018.01.001.
Radak D, Katsiki N, Resanovic I, et al. Apoptosis and Acute Brain Ischemia in ischemic stroke. CVP. 2017;15(2):115–22. https://doi.org/10.2174/1570161115666161104095522.
Powers WJ. Acute ischemic stroke. Solomon CG. ed N Engl J Med. 2020;383(3):252–60. https://doi.org/10.1056/NEJMcp1917030.
Karandikar P, Gerstl JVE, Kappel AD, et al. SUMOtherapeutics for ischemic stroke. Pharmaceuticals. 2023;16(5):673. https://doi.org/10.3390/ph16050673.
Marko M, Posekany A, Szabo S, et al. Trends of r-tPA (recombinant tissue-type plasminogen activator) treatment and treatment-influencing factors in Acute ischemic stroke. Stroke. 2020;51(4):1240–7. https://doi.org/10.1161/STROKEAHA.119.027921.
Strbian D, Engelter S, Michel P, Meretoja A, Sekoranja L, Ahlhelm FJ, Mustanoja S, Kuzmanovic I, Sairanen T, Forss N, Cordier M, Lyrer P, Kaste M, Tatlisumak T. Symptomatic intracranial hemorrhage after stroke thrombolysis: the SEDAN score. Ann Neurol. 2012;71(5):634–41. https://doi.org/10.1002/ana.23546.
Lee TH, Yeh JC, Tsai CH, et al. Improved thrombolytic effect with focused ultrasound and neuroprotective agent against acute carotid artery thrombosis in rat. Sci Rep. 2017;7(1):1638. https://doi.org/10.1038/s41598-017-01769-2.
Putri SP, Nakayama Y, Matsuda F, et al. Current metabolomics: practical applications. J Biosci Bioeng. 2013;115(6):579–89. https://doi.org/10.1016/j.jbiosc.2012.12.007.
Nicholson JK, Lindon JC, Holmes E. Metabonomics: understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica. 1999;29(11):1181–9. https://doi.org/10.1080/004982599238047.
Qian W, Wu M, Qian T, **e C, Gao Y, Qian S. The roles and mechanisms of gut microbiome and metabolome in patients with cerebral infarction. Front Cell Infect Microbiol. 2023;13:1112148. https://doi.org/10.3389/fcimb.2023.1112148.
Li G, Jian T, Liu X, Lv Q, Zhang G, Ling J. Application of Metabolomics in Fungal Research. Molecules. 2022;27(21):7365. https://doi.org/10.3390/molecules27217365.
Khan V, Putluri N, Sreekumar A, Mindikoglu A. Current applications of Metabolomics in cirrhosis. Metabolites. 2018;8(4):67. https://doi.org/10.3390/metabo8040067.
Wu W, Shi J, ** J, et al. Comprehensive metabolic analyses provide new insights into primary and secondary metabolites in different tissues of Jianghua Kucha tea (Camellia sinensis var. assamica Cv. Jianghua). Front Nutr. 2023;10:1181135. https://doi.org/10.3389/fnut.2023.1181135.
Lee EJ, Kim DJ, Kang DW, et al. Targeted metabolomic biomarkers for Stroke Subty**. Transl Stroke Res Published Online Febr. 2023;11. https://doi.org/10.1007/s12975-023-01137-5.
Dunn WB, Wilson ID, Nicholls AW, Broadhurst D. The importance of experimental design and QC samples in large-scale and MS-driven untargeted metabolomic studies of humans. Bioanalysis. 2012;4(18):2249–64. https://doi.org/10.4155/bio.12.204.
Naz S, Vallejo M, García A, Barbas C. Method validation strategies involved in non-targeted metabolomics. J Chromatogr A. 2014;1353:99–105. https://doi.org/10.1016/j.chroma.2014.04.071.
Shin TH, Lee DY, Basith S, et al. Metabolome changes in cerebral ischemia. Cells. 2020;9(7):1630. https://doi.org/10.3390/cells9071630.
Azad RK, Shulaev V. Metabolomics technology and bioinformatics for precision medicine. Brief Bioinform. 2019;20(6):1957–71. https://doi.org/10.1093/bib/bbx170.
Moco S, Vervoort J, Moco S, Bino RJ, De Vos RCH, Bino R. Metabolomics technologies and metabolite identification. TRAC Trends Anal Chem. 2007;26(9):855–66. https://doi.org/10.1016/j.trac.2007.08.003.
Stettin D, Poulin RX, Pohnert G. Metabolomics benefits from Orbitrap GC–MS—Comparison of low- and high-resolution GC–MS. Metabolites. 2020;10(4):143. https://doi.org/10.3390/metabo10040143.
Fang ZZ, Gonzalez FJ. LC–MS-based metabolomics: an update. Arch Toxicol. 2014;88(8):1491–502. https://doi.org/10.1007/s00204-014-1234-6.
Miggiels P, Wouters B, Van Westen GJP, Dubbelman AC, Hankemeier T. Novel technologies for metabolomics: more for less. TRAC Trends Anal Chem. 2019;120:115323. https://doi.org/10.1016/j.trac.2018.11.021.
Chong J, Wishart DS, **a J. Using MetaboAnalyst 4.0 for Comprehensive and Integrative Metabolomics Data Analysis. CP Bioinf. 2019;68(1):e86. https://doi.org/10.1002/cpbi.86.
Lasalvia M, Capozzi V, Perna G. A comparison of PCA-LDA and PLS-DA techniques for classification of Vibrational Spectra. Appl Sci. 2022;12(11):5345. https://doi.org/10.3390/app12115345.
Wang K, Wang X, Zhang L, Chen A, Yang S, Xu Z. Identification of novel biomarkers in chilled and frozen chicken using metabolomics profiling and its application. Food Chem. 2022;393:133334. https://doi.org/10.1016/j.foodchem.2022.133334.
Li Z, Lu Y, Guo Y, Cao H, Wang Q, Shui W. Comprehensive evaluation of untargeted metabolomics data processing software in feature detection, quantification and discriminating marker selection. Anal Chim Acta. 2018;1029:50–7. https://doi.org/10.1016/j.aca.2018.05.001.
Kutuzova S, Colaianni P, Röst H, et al. SmartPeak automates targeted and Quantitative Metabolomics Data Processing. Anal Chem. 2020;92(24):15968–74. https://doi.org/10.1021/acs.analchem.0c03421.
Gao X, Wang J, Chen X, et al. Reduning injection prevents carrageenan-induced inflammation in rats by serum and urine metabolomics analysis. Chin Herb Med. 2022;14(4):583–91. https://doi.org/10.1016/j.chmed.2022.01.007.
Huang D, Yang Y, Song W, et al. Untargeted metabonomic analysis of a cerebral stroke model in rats: a study based on UPLC–MS/MS. Front Neurosci. 2023;17:1084813. https://doi.org/10.3389/fnins.2023.1084813.
Zhao L, Wang C, Peng S, et al. Pivotal interplays between fecal metabolome and gut microbiome reveal functional signatures in cerebral ischemic stroke. J Transl Med. 2022;20(1):459. https://doi.org/10.1186/s12967-022-03669-0.
Mottahedin A, Prag HA, Dannhorn A, et al. Targeting succinate metabolism to decrease brain injury upon mechanical thrombectomy treatment of ischemic stroke. Redox Biol. 2023;59:102600. https://doi.org/10.1016/j.redox.2023.102600.
Guo J, Wang H, Jiang X et al. An Untargeted Lipidomics Study of Acute Ischemic Stroke with Hyperglycemia Based on Ultrahigh-Performance Liquid Chromatography-Mass Spectrometry. Ren X, ed. Computational and Mathematical Methods in Medicine. 2022;2022:1–13. https://doi.org/10.1155/2022/8332278.
Guo Y, Chen S, Zhang Y, et al. Circulating metabolites associated with incident myocardial infarction and stroke: a prospective cohort study of 90 438 participants. J Neurochem. 2022;162(4):371–84. https://doi.org/10.1111/jnc.15659.
Tiedt S, Brandmaier S, Kollmeier H, et al. Circulating metabolites differentiate Acute Ischemic Stroke from Stroke mimics. Ann Neurol. 2020;88(4):736–46. https://doi.org/10.1002/ana.25859.
Rashad S, Saigusa D, Yamazaki T, et al. Metabolic basis of neuronal vulnerability to ischemia; an in vivo untargeted metabolomics approach. Sci Rep. 2020;10(1):6507. https://doi.org/10.1038/s41598-020-63483-w.
Sidorov E, Bejar C, Xu C, et al. Potential metabolite biomarkers for Acute Versus Chronic Stage of ischemic stroke: a pilot study. J Stroke Cerebrovasc Dis. 2020;29(4):104618. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104618.
Sidorov EV, Rout M, Xu C, et al. Difference in acute and chronic stage ischemic stroke metabolic markers with controls. J Stroke Cerebrovasc Dis. 2023;32(8):107211. https://doi.org/10.1016/j.jstrokecerebrovasdis.2023.107211.
Sidorov EV, Xu C, Garcia-Ramiu J, Blair A, Ortiz-Garcia J, Gordon D, Chainakul J, Sanghera DK. Global metabolomic profiling reveals disrupted lipid and amino acid metabolism between the Acute and chronic stages of ischemic stroke. J Stroke Cerebrovasc Dis. 2022;31(4):106320. https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106320.
Lai M, Zhang X, Zhou D, et al. Integrating serum proteomics and metabolomics to compare the common and distinct features between acute aggressive ischemic stroke (APIS) and acute non-aggressive ischemic stroke (ANPIS). J Proteom. 2022;261:104581. https://doi.org/10.1016/j.jprot.2022.104581.
Sidorov EV, Bejar C, Xu C, et al. Novel metabolites as potential indicators of ischemic infarction volume: a pilot study. Transl Stroke Res. 2021;12(5):778–84. https://doi.org/10.1007/s12975-020-00876-z.
Persky RW, Turtzo LC, McCullough LD. Stroke in women: disparities and outcomes. Curr Cardiol Rep. 2010;12(1):6–13. https://doi.org/10.1007/s11886-009-0080-2.
Wolf V, Abdul Y, Li W, Ergul A. Impact of diabetes and ischemic stroke on the cerebrovasculature: a female perspective. Neurobiol Dis. 2022;167:105667. https://doi.org/10.1016/j.nbd.2022.105667.
Arboix A, Milian M, Oliveres M, García-Eroles L, Massons J. Impact of female gender on prognosis in type 2 Diabetic patients with ischemic stroke. Eur Neurol. 2006;56(1):6–12. https://doi.org/10.1159/000094249.
Zhang Q, Guo P, Wang J, Yang M, Kong L. Gender-specific metabolic responses in focal cerebral ischemia of rats and Huang-Lian-Jie-Du decoction treatment. RSC Adv. 2015;5(116):95558–75. https://doi.org/10.1039/C5RA19934D.
Dylla L, Higgins HM, Piper C, Poisson SN, Herson PS, Monte AA. Sex as a biological variable in determining the metabolic changes influencing acute ischemic stroke outcomes—where is the data: a systematic review. Front Neurol. 2022;13:1026431. https://doi.org/10.3389/fneur.2022.1026431.
Balasubramanian R, Hu J, Guasch-Ferre M, et al. Metabolomic profiles Associated With Incident Ischemic Stroke. Neurology. 2022;98(5):e483–92. https://doi.org/10.1212/WNL.0000000000013129.
Poupore N, Chosed R, Arce S, Rainer R, Goodwin RL, Nathaniel TI. Metabolomic profiles of men and women ischemic stroke patients. Diagnostics. 2021;11(10):1786. https://doi.org/10.3390/diagnostics11101786.
Jacob MA, Ekker MS, Allach Y, Cai M, Aarnio K, Arauz A, Arnold M, Bae HJ, Bandeo L, Barboza MA, Bolognese M, Bonardo P, Brouns R, Chuluun B, Chuluunbatar E, Cordonnier C, Dagvajantsan B, Debette S, Don A, Enzinger C, Ekizoglu E, Fandler-Höfler S, Fazekas F, Fromm A, Gattringer T, Hora TF, Jern C, Jood K, Kim YS, Kittner S, Kleinig T, Klijn CJM, Kõrv J, Kumar V, Lee KJ, Lee TH, Maaijwee NAM, Martinez-Majander N, Marto J, Mehndiratta MM, Mifsud V, Montanaro V, Pacio G, Patel VB, Phillips MC, Piechowski-Jozwiak B, Pikula A, Ruiz-Sandoval J, von Sarnowski B, Swartz RH, Tan KS, Tanne D, Tatlisumak T, Thijs V, Viana-Baptista M, Vibo R, Wu TY, Yesilot N, Waje-Andreassen U, Pezzini A, Putaala J, Tuladhar AM, de Leeuw FE. Global differences in risk factors, etiology, and outcome of ischemic stroke in young Adults-A Worldwide Meta-analysis. GOAL Initiative Neurol. 2022;98(6):e573–88. https://doi.org/10.1212/WNL.0000000000013195.
Arboix A, Martí-Vilalta JL. Lacunar stroke. Expert Rev Neurother. 2009;9(2):179–96. https://doi.org/10.1586/14737175.9.2.179.
Arboix A, Estevez S, Rouco R, Oliveres M, García-Eroles L, Massons J. Clinical characteristics of acute lacunar stroke in young adults. Expert Rev Neurother. 2015;15(7):825–31. https://doi.org/10.1586/14737175.2015.1049997.
Liu J, Yuan J, Zhao J, Zhang L, Wang Q, Wang G. Serum metabolomic patterns in young patients with ischemic stroke: a case study. Metabolomics. 2021;17(2):24. https://doi.org/10.1007/s11306-021-01774-7.
Ke C, Shi M, Guo D, et al. Metabolomics on vascular events and death after acute ischemic stroke: a prospective matched nested case-control study. Atherosclerosis. 2022;351:1–8. https://doi.org/10.1016/j.atherosclerosis.2022.05.001.
Chi NF, Chang TH, Lee CY, et al. Untargeted metabolomics predicts the functional outcome of ischemic stroke. J Formos Med Assoc. 2021;120(1):234–41. https://doi.org/10.1016/j.jfma.2020.04.026.
Liu T, Song H, et al. Targeted Metabolomic Profiling reveals Association between altered amino acids and poor functional recovery after stroke. Front Neurol. 2020;10:1425. https://doi.org/10.3389/fneur.2019.01425.
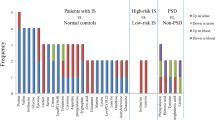
Liu H, Pu J, Zhou Q, Yang L, Bai D. Peripheral blood and urine metabolites and biological functions in post-stroke depression. Metab Brain Dis. 2022;37(5):1557–68. https://doi.org/10.1007/s11011-022-00984-9.
Wang X, Zhang L, Sun W, et al. Changes of metabolites in Acute ischemic stroke and its subtypes. Front Neurosci. 2021;14:580929. https://doi.org/10.3389/fnins.2020.580929.
Chen C, Qiao X, Guo J, et al. Related factors based on non-targeted metabolomics methods in minor ischaemic stroke. Front Endocrinol. 2022;13:952918. https://doi.org/10.3389/fendo.2022.952918.
Wu W, Sun Y, Luo N, et al. Integrated 16S rRNA gene sequencing and LC-MS analysis revealed the interplay between gut microbiota and plasma metabolites in rats with ischemic stroke. J Mol Neurosci. 2021;71(10):2095–106. https://doi.org/10.1007/s12031-021-01828-4.
Lewerenz J, Maher P. Chronic glutamate toxicity in neurodegenerative diseases—what is the evidence? Front Neurosci. 2015;9. https://doi.org/10.3389/fnins.2015.00469.
Neves D, Salazar IL, Almeida RD, Silva RM. Molecular mechanisms of ischemia and glutamate excitotoxicity. Life Sci. 2023;328:121814. https://doi.org/10.1016/j.lfs.2023.121814.
Pajarillo E, Rizor A, Lee J, Aschner M, Lee E. The role of astrocytic glutamate transporters GLT-1 and GLAST in neurological disorders: potential targets for neurotherapeutics. Neuropharmacology. 2019;161:107559. https://doi.org/10.1016/j.neuropharm.2019.03.002.
Walls AB, Waagepetersen HS, Bak LK, Schousboe A, Sonnewald U. The Glutamine–Glutamate/GABA cycle: function, Regional differences in Glutamate and GABA Production and effects of interference with GABA metabolism. Neurochem Res. 2015;40(2):402–9. https://doi.org/10.1007/s11064-014-1473-1.
Liu M, Zhou K, Li H, et al. Potential of serum metabolites for diagnosing post-stroke cognitive impairment. Mol BioSyst. 2015;11(12):3287–96. https://doi.org/10.1039/C5MB00470E.
Luo L, Li Y, Shan H, et al. L-glutamine protects mouse brain from ischemic injury via up‐regulating heat shock protein 70. CNS Neurosci Ther. 2019;25(9):1030–41. https://doi.org/10.1111/cns.13184.
Campos F, Sobrino T, Ramos-Cabrer P, Castillo J, Oxaloacetate. A novel neuroprotective for acute ischemic stroke. Int J Biochem Cell Biol. 2012;44(2):262–5. https://doi.org/10.1016/j.biocel.2011.11.003.
Nitz K, Lacy M, Atzler D. Amino acids and their metabolism in atherosclerosis. ATVB. 2019;39(3):319–30. https://doi.org/10.1161/ATVBAHA.118.311572.
Grosse GM, Schwedhelm E, Worthmann H, Choe C. un. Arginine Derivatives in Cerebrovascular Diseases: Mechanisms and Clinical Implications. IJMS. 2020;21(5):1798. https://doi.org/10.3390/ijms21051798.
Jarzebska N, Mangoni AA, Martens-Lobenhoffer J, Bode-Böger SM, Rodionov RN. The Second Life of Methylarginines as Cardiovascular targets. IJMS. 2019;20(18):4592. https://doi.org/10.3390/ijms20184592.
Yoo HS, Shanmugalingam U, Smith PD. Potential roles of branched-chain amino acids in neurodegeneration. Nutrition. 2022;103–104:111762. https://doi.org/10.1016/j.nut.2022.111762.
Liu R, Zhang L, You H. Insulin Resistance and impaired branched-chain amino acid metabolism in Alzheimer’s Disease. JAD. 2023;93(3):847–62. https://doi.org/10.3233/JAD-221147.
Kimberly WT, Wang Y, Pham L, Furie KL, Gerszten RE. Metabolite Profiling identifies a branched chain amino acid signature in Acute Cardioembolic Stroke. Stroke. 2013;44(5):1389–95. https://doi.org/10.1161/STROKEAHA.111.000397.
Yudkoff M, Daikhin Y, Melø TM, Nissim I, Sonnewald U, Nissim I. The ketogenic Diet and Brain metabolism of amino acids: relationship to the anticonvulsant effect. Annu Rev Nutr. 2007;27(1):415–30. https://doi.org/10.1146/annurev.nutr.27.061406.093722.
Yudkoff M. Interactions in the metabolism of glutamate and the branched-chain amino acids and ketoacids in the CNS. Neurochem Res. 2017;42(1):10–8. https://doi.org/10.1007/s11064-016-2057-z.
Batch BC, Hyland K, Svetkey LP. Branch chain amino acids: biomarkers of health and disease. Current opinion in Clinical Nutrition and Metabolic Care. Published Online Dec 2013:1. https://doi.org/10.1097/MCO.0000000000000010.
Stephan J, Friauf E. Functional analysis of the inhibitory neurotransmitter transporters GlyT1, GAT-1, and GAT‐3 in astrocytes of the lateral superior olive. Glia. 2014;62(12):1992–2003. https://doi.org/10.1002/glia.22720.
Zhong Z, Wheeler MD, Li X, et al. L-Glycine: a novel antiinflammatory, immunomodulatory, and cytoprotective agent. Curr Opin Clin Nutr Metab Care. 2003;6(2):229–40. https://doi.org/10.1097/00075197-200303000-00013.
Bie X, Chen Y, Han J, Dai H, Wan H, Zhao T. Effects of gastrodin on amino acids after cerebral ischemia-reperfusion injury in rat striatum. Asia Pac J Clin Nutr. 2007;16(Suppl 1):305–8. PMID: 17392124.
Chen YH, Yu Z, Fu L, et al. Vitamin D3 inhibits lipopolysaccharide-induced placental inflammation through reinforcing interaction between vitamin D receptor and nuclear factor kappa B p65 subunit. Sci Rep. 2015;5(1):10871. https://doi.org/10.1038/srep10871.
Rahimpour S, Zheng W, Monaghan KL, Wan ECK. A potential monocyte-regulatory T cell axis in neurorestoration following ischemic stroke. J Immunol. 2022;208(1Supplement):54. https://doi.org/10.4049/jimmunol.208.Supp.54.13.
Spence JD. Homocysteine-lowering therapy: a role in stroke prevention? Lancet Neurol. 2007;6(9):830–8. https://doi.org/10.1016/S1474-4422(07)70219-3.
Pinzon RT, Wijaya VO, Veronica V. The role of homocysteine levels as a risk factor of ischemic stroke events: a systematic review and meta-analysis. Front Neurol. 2023;14:1144584. https://doi.org/10.3389/fneur.2023.1144584.
Upchurch GR, Welch GN, Fabian AJ, et al. Homocyst(e)ine decreases bioavailable nitric oxide by a mechanism involving Glutathione Peroxidase. J Biol Chem. 1997;272(27):17012–7. https://doi.org/10.1074/jbc.272.27.17012.
Görtz P, Hoinkes A, Fleischer W, et al. Implications for hyperhomocysteinemia: not homocysteine but its oxidized forms strongly inhibit neuronal network activity. J Neurol Sci. 2004;218(1–2):109–14. https://doi.org/10.1016/j.jns.2003.11.009.
Boldyrev A, Bryushkova E, Mashkina A, Vladychenskaya E. Why is homocysteine toxic for the nervous and Immune systems? CAS. 2013;6(1):29–36. https://doi.org/10.2174/18746098112059990007.
Rabelo NN, Telles JPM, Pipek LZ et al. TJ Siddiqi ed. 2022 Homocysteine is associated with higher risks of ischemic stroke: a systematic review and meta-analysis. PLoS ONE 17 10 e0276087 https://doi.org/10.1371/journal.pone.0276087.
Korczowska-Łącka I, Hurła M, Banaszek N, et al. Selected biomarkers of oxidative stress and Energy Metabolism disorders in Neurological diseases. Mol Neurobiol. 2023;60(7):4132–49. https://doi.org/10.1007/s12035-023-03329-4.
Vo**ovic D, Kalaoja M, Trompet S, et al. Association of circulating metabolites in plasma or serum and risk of stroke: Meta-analysis from 7 prospective cohorts. Neurology. 2021;96(8):e1110–23. https://doi.org/10.1212/WNL.0000000000011236.
Floegel A, Stefan N, Yu Z, et al. Identification of serum metabolites Associated with risk of type 2 diabetes using a targeted Metabolomic Approach. Diabetes. 2013;62(2):639–48. https://doi.org/10.2337/db12-0495.
Tracey TJ, Steyn FJ, Wolvetang EJ, Ngo ST. Neuronal lipid metabolism: multiple pathways driving functional outcomes in Health and Disease. Front Mol Neurosci. 2018;11:10. https://doi.org/10.3389/fnmol.2018.00010.
Pradas I, Jové M, Huynh K, et al. Exceptional human longevity is associated with a specific plasma phenotype of ether lipids. Redox Biol. 2019;21:101127. https://doi.org/10.1016/j.redox.2019.101127.
Venø SK, Schmidt EB, Bork CS. Polyunsaturated fatty acids and risk of ischemic stroke. Nutrients. 2019;11(7):1467. https://doi.org/10.3390/nu11071467.
Wang J, Shi Y, Zhang L, et al. Omega-3 polyunsaturated fatty acids enhance cerebral angiogenesis and provide long-term protection after stroke. Neurobiol Dis. 2014;68:91–103. https://doi.org/10.1016/j.nbd.2014.04.014.
Zhang M, Wang S, Mao L, et al. Omega-3 fatty acids protect the brain against Ischemic Injury by activating Nrf2 and Upregulating Heme Oxygenase 1. J Neurosci. 2014;34(5):1903–15. https://doi.org/10.1523/JNEUROSCI.4043-13.2014.
Chao XD, Ma YH, Luo P, et al. Up-regulation of Heme oxygenase-1 attenuates brain damage after cerebral ischemia via simultaneous inhibition of superoxide production and preservation of NO bioavailability. Exp Neurol. 2013;239:163–9. https://doi.org/10.1016/j.expneurol.2012.09.020.
Lv H, Jia S, Sun Y, et al. Docosahexaenoic acid promotes M2 microglia phenotype via activating PPARγ-mediated ERK/AKT pathway against cerebral ischemia-reperfusion injury. Brain Res Bull. 2023;199:110660. https://doi.org/10.1016/j.brainresbull.2023.110660.
Zhang Y. Mechanism of neuroprotective effect of stevioside on cerebral ischemia-reperfusion injury via PPAR-γ activation. Immunopharmacol Immunotoxicol. 2021;43(6):704–12. https://doi.org/10.1080/08923973.2021.1966034.
Sabogal-Guáqueta AM, Villamil-Ortiz JG, Arias-Londoño JD, Cardona-Gómez GP. Inverse Phosphatidylcholine/Phosphatidylinositol Levels as Peripheral Biomarkers and Phosphatidylcholine/Lysophosphatidylethanolamine-Phosphatidylserine as hippocampal Indicator of Postischemic Cognitive impairment in rats. Front Neurosci. 2018;12:989. https://doi.org/10.3389/fnins.2018.00989.
Rabiei Z, Bigdeli MR, Rasoulian B, Ghassempour A, Mirzajani F. The neuroprotection effect of pretreatment with olive leaf extract on brain lipidomics in rat stroke model. Phytomedicine. 2012;19(10):940–6. https://doi.org/10.1016/j.phymed.2012.06.003.
Koizumi S, Yamamoto S, Hayasaka T, et al. Imaging mass spectrometry revealed the production of lyso-phosphatidylcholine in the injured ischemic rat brain. Neuroscience. 2010;168(1):219–25. https://doi.org/10.1016/j.neuroscience.2010.03.056.
Wang R, Liu S, Liu T, et al. Mass spectrometry-based serum lipidomics strategy to explore the mechanism of Eleutherococcus senticosus (rupr. & Maxim.) Maxim. Leaves in the treatment of ischemic stroke. Food Funct. 2021;12(10):4519–34. https://doi.org/10.1039/D0FO02845B.
Ma Y, Chen Z, He Q, et al. Spatiotemporal lipidomics reveals key features of brain lipid dynamic changes after cerebral ischemia and reperfusion therapy. Pharmacol Res. 2022;185:106482. https://doi.org/10.1016/j.phrs.2022.106482.
Bitar L, Uphaus T, Thalman C, et al. Inhibition of the enzyme autotaxin reduces cortical excitability and ameliorates the outcome in stroke. Sci Transl Med. 2022;14(641):eabk0135. https://doi.org/10.1126/scitranslmed.abk0135.
Lind L, Salihovic S, Ganna A, et al. A Multi-cohort Metabolomics Analysis discloses Sphingomyelin (32:1) levels to be inversely related to Incident Ischemic Stroke. J Stroke Cerebrovasc Dis. 2020;29(2):104476. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104476.
Signorelli P, Conte C, Albi E. The multiple roles of Sphingomyelin in Parkinson’s Disease. Biomolecules. 2021;11(9):1311. https://doi.org/10.3390/biom11091311.
Nielsen MMB, Lambertsen KL, Clausen BH, et al. Mass spectrometry imaging of biomarker lipids for phagocytosis and signalling during focal cerebral ischaemia. Sci Rep. 2016;6(1):39571. https://doi.org/10.1038/srep39571.
Novgorodov SA, Gudz TI. Ceramide and mitochondria in ischemic brain injury. Int J Biochem Mol Biol 2011;2(4):347 – 61. Epub 2011 Nov 25. PMID: 22187669.
Adibhatla RM, Hatcher JF, Larsen EC, Chen X, Sun D, Tsao FHC. CDP-choline significantly restores phosphatidylcholine levels by differentially affecting phospholipase A2 and CTP: Phosphocholine Cytidylyltransferase after Stroke. J Biol Chem. 2006;281(10):6718–25. https://doi.org/10.1074/jbc.M512112200.
Lamour NF, Wijesinghe DS, Mietla JA, Ward KE, Stahelin RV, Chalfant CE. Ceramide kinase regulates the production of Tumor necrosis factor α (TNFα) via inhibition of TNFα-converting enzyme. J Biol Chem. 2011;286(50):42808–17. https://doi.org/10.1074/jbc.M111.310169.
Kawahara A, Nishi T, Hisano Y, Fukui H, Yamaguchi A, Mochizuki N. The Sphingolipid Transporter Spns2 functions in Migration of zebrafish myocardial precursors. Science. 2009;323(5913):524–7. https://doi.org/10.1126/science.1167449.
Sun N, Keep RF, Hua Y, ** G. Critical role of the Sphingolipid Pathway in Stroke: a review of current utility and potential therapeutic targets. Transl Stroke Res. 2016;7(5):420–38. https://doi.org/10.1007/s12975-016-0477-3.
Wang YY, Lin SY, Chang CY, et al. α7 nicotinic acetylcholine receptor agonist improved brain injury and impaired glucose metabolism in a rat model of ischemic stroke. Metab Brain Dis. 2023;38(4):1249–59. https://doi.org/10.1007/s11011-023-01167-w.
Vannucci SJ, Seaman LB, Vannucci RC. Effects of hypoxia-ischemia on GLUT1 and GLUT3 glucose transporters in immature rat brain. J Cereb Blood Flow Metab. 1996;16(1):77–81. https://doi.org/10.1097/00004647-199601000-00009.
Geng J, Zhang Y, Li S, et al. Metabolomic profiling reveals that reprogramming of cerebral glucose metabolism is involved in Ischemic Preconditioning-Induced Neuroprotection in a Rodent Model of ischemic stroke. J Proteome Res Published Online. October 2018;26. :acs.jproteome.8b00339.
Enciu AM, Gherghiceanu M, Popescu BO. Triggers and effectors of oxidative stress at blood-brain barrier level: relevance for Brain Ageing and Neurodegeneration. Oxidative Med Cell Longev. 2013;2013:1–12. https://doi.org/10.1155/2013/297512.
Huang L, Xu G, Zhang R, et al. Increased admission serum total bile acids can be associated with decreased 3-month mortality in patients with acute ischemic stroke. Lipids Health Dis. 2022;21(1):15. https://doi.org/10.1186/s12944-021-01620-8.
Zhu Z, Yang P, Jia Y, Wang Y, Shi M, Zhong C, Peng H, Sun L, Guo D, Xu Q, Chen J, Wang A, Xu T, He J, Zhang Y. Plasma amino acid neurotransmitters and ischemic stroke prognosis: a Multicenter prospective study. Am J Clin Nutr. 2023;118(4):754–62. https://doi.org/10.1016/j.ajcnut.2023.06.014.
Goulart VAM, Sena MM, Mendes TO, et al. Amino acid biosignature in plasma among ischemic stroke subtypes. Biomed Res Int. 2019;2019:1–11. https://doi.org/10.1155/2019/8480468.
Wang Z, Li J, Xu Y, et al. Elevated gut microbiota metabolite bile acids confer protective effects on clinical prognosis in ischemic stroke patients. Front Neurosci. 2024;18:1388748. https://doi.org/10.3389/fnins.2024.1388748.
Wu M, Chang C, Lin Y, Chen C. Identification of a potential prognostic plasma biomarker of acute ischemic stroke via untargeted LC-MS metabolomics. Proteomics clinical apps. Published Online June. 2023;27:2200081. https://doi.org/10.1002/prca.202200081.
Zheng Y, Hu FB, Ruiz-Canela M, et al. Metabolites of Glutamate Metabolism are Associated With Incident Cardiovascular events in the PREDIMED PREvención con DIeta MEDiterránea (PREDIMED) trial. JAHA. 2016;5(9):e003755. https://doi.org/10.1161/JAHA.116.003755.
Huang Y, Gu C, **a X, Li X. Metabolomics analysis on patients with ischemic stroke based on ultra-performance liquid chromatography with quadrupole-timeof-flight mass spectrometry. Int J Clin Exp Med. 2017;10:10277–86.
Wang D, Kong J, Wu J, Wang X, Lai M. GC–MS-based metabolomics identifies an amino acid signature of acute ischemic stroke. Neurosci Lett. 2017;642:7–13. https://doi.org/10.1016/j.neulet.2017.01.039.
Yu Y, Wen X, Lin JG, et al. Identification of three potential novel biomarkers for early diagnosis of acute ischemic stroke via plasma lipidomics. Metabolomics. 2023;19(4):32. https://doi.org/10.1007/s11306-023-01990-3.
Yang L, Lv P, Ai W, et al. Lipidomic analysis of plasma in patients with lacunar infarction using normal-phase/reversed-phase two-dimensional liquid chromatography–quadrupole time-of-flight mass spectrometry. Anal Bioanal Chem. 2017;409(12):3211–22. https://doi.org/10.1007/s00216-017-0261-6.
Yu F, Li X, Feng X, et al. Phenylacetylglutamine, a Novel Biomarker in Acute ischemic stroke. Front Cardiovasc Med. 2021;8:798765. https://doi.org/10.3389/fcvm.2021.798765.
Qi B, Zhang Y, Xu B, et al. Metabolomic characterization of Acute ischemic stroke facilitates metabolomic Biomarker Discovery. Appl Biochem Biotechnol. 2022;194(11):5443–55. https://doi.org/10.1007/s12010-022-04024-1.
Lin CN, Hsu KC, Huang KL, Huang WC, Hung YL, Lee TH. Identification of Metabolomics Biomarkers in Extracranial Carotid artery stenosis. Cells. 2022;11(19):3022. https://doi.org/10.3390/cells11193022.
Zhou W, Li S, Sun G, et al. Early warning of ischemic stroke based on Atherosclerosis Index Combined with serum markers. J Clin Endocrinol Metabolism. 2022;107(7):1956–64. https://doi.org/10.1210/clinem/dgac176.
Zhao T, Yan Q, Wang C, et al. Identification of serum biomarkers of ischemic stroke in a Hypertensive Population based on Metabolomics and Lipidomics. Neuroscience. 2023;533:22–35. https://doi.org/10.1016/j.neuroscience.2023.09.017.
Arboix A, Besses C. Cerebrovascular disease as the initial clinical presentation of haematological disorders. Eur Neurol. 1997;37(4):207–11. https://doi.org/10.1159/000117444.
Wang T, Liu J, Luo X, Hu L, Lu H. Functional metabolomics innovates therapeutic discovery of traditional Chinese medicine derived functional compounds. Pharmacol Ther. 2021;224:107824. https://doi.org/10.1016/j.pharmthera.2021.107824.
Mu F, Lin R, Lu X, et al. Protective effect and mechanism of styrax on ischemic stroke rats: metabonomic insights by UPLC-Q/TOF-MS analysis. Pharm Biol. 2023;61(1):1318–31. https://doi.org/10.1080/13880209.2023.2246501.
Yu X, Luo Y, Yang L, Duan X. Plasma metabonomic study on the effect of para –hydroxybenzaldehyde intervention in a rat model of transient focal cerebral ischemia. Mol Med Rep. 2023;28(5):224. https://doi.org/10.3892/mmr.2023.13111.
Sun J, Chen X, Wang Y, et al. Neuroprotective effects of Longxue Tongluo Capsule on ischemic stroke rats revealed by LC-MS/MS-based metabolomics approach. Chin Herb Med. 2023;15(3):430–8. https://doi.org/10.1016/j.chmed.2022.12.010.
Zhang J, Qi A, Liu L, Cai C, Xu H. Gas chromatography–Mass Spectrometry-based cerebrospinal fluid metabolomics to reveal the Protection of Coptisine against transient focal cerebral ischemia–reperfusion Injury via Anti-inflammation and antioxidant. Molecules. 2023;28(17):6350. https://doi.org/10.3390/molecules28176350.
Chen J, Zhuang Y, Zhang ZF, et al. Glycine confers neuroprotection through microRNA-301a/PTEN signaling. Mol Brain. 2016;9(1):59. https://doi.org/10.1186/s13041-016-0241-3.
Hong J, Li G, Zhang Q, Ritter J, Li W, Li PL. D-Ribose induces podocyte NLRP3 inflammasome activation and Glomerular Injury via AGEs/RAGE pathway. Front Cell Dev Biol. 2019;7:259. https://doi.org/10.3389/fcell.2019.00259.
Wang R, Sun Y, Wang M, Li H, Liu S, Liu Z. Therapeutic effect of Eleutherococcus senticosus (Rupr. & Maxim.) Maxim. leaves on ischemic stroke via the microbiota–gut–brain axis. Phytotherapy Research. Published online July 30, 2023:ptr.7947. https://doi.org/10.1002/ptr.7947.
Wang K, Chen Y, Cao J, et al. Mechanism of Huangqi–honghua combination regulating the gut microbiota to affect bile acid metabolism towards preventing cerebral ischaemia–reperfusion injury in rats. Pharm Biol. 2022;60(1):2189–99. https://doi.org/10.1080/13880209.2022.2136209.
Yang L, Su X, Lu F, et al. Serum and brain metabolomic study reveals the protective effects of Bai-Mi-Decoction on rats with ischemic stroke. Front Pharmacol. 2022;13:1005301. https://doi.org/10.3389/fphar.2022.1005301.
Luo Y, Chen P, Yang L, Duan X. Metabolomic analysis and pharmacological validation of the cerebral protective effect of 3,4–dihydroxybenzaldehyde on cerebral ischemia–reperfusion injury. Mol Med Rep. 2022;27(1):9. https://doi.org/10.3892/mmr.2022.12896.
Chen C, Duan F, **e Y, et al. Nuciferine attenuates acute ischemic stroke in a rat model: a metabolomic approach for the mechanistic study. Mol Omics. 2022;18(8):765–78. https://doi.org/10.1039/D2MO00158F.
Yang Yhui, Lei L, Bao Y, **, Zhang L. An Integrated Metabolomic Screening Platform discovers the potential biomarkers of ischemic stroke and reveals the protective effect and mechanism of folic acid. Front Mol Biosci. 2022;9:783793. https://doi.org/10.3389/fmolb.2022.783793.
Ma Hfen, Zheng F, Su Ljie, et al. Metabolomic profiling of Brain Protective Effect of Edaravone on Cerebral Ischemia-Reperfusion Injury in mice. Front Pharmacol. 2022;13:814942. https://doi.org/10.3389/fphar.2022.814942.
Zhou P, Zhou L, Shi Y, et al. Neuroprotective effects of Danshen Chuanxiongqin Injection against ischemic stroke: metabolomic insights by UHPLC-Q-Orbitrap HRMS Analysis. Front Mol Biosci. 2021;8:630291. https://doi.org/10.3389/fmolb.2021.630291.
Hou Jyi, Cao G, zhao, Tian L, liang, et al. Integrated transcriptomics and metabolomics analysis reveals that C3 and C5 are vital targets of DuZhi Wan in protecting against cerebral ischemic injury. Biomed Pharmacother. 2022;155:113703. https://doi.org/10.1016/j.biopha.2022.113703.
Ye J, Huang F, Zeng H, et al. Multi-omics and network pharmacology study reveals the effects of Dengzhan Shengmai capsule against neuroinflammatory injury and thrombosis induced by ischemic stroke. J Ethnopharmacol. 2023;305:116092. https://doi.org/10.1016/j.jep.2022.116092.
Saini V, Guada L, Yavagal DR. Global Epidemiology of Stroke and Access to acute ischemic stroke interventions. Neurology. 2021;97(20S):S6–16. https://doi.org/10.1212/WNL.0000000000012781.
Rabinstein AA. Update on treatment of Acute ischemic stroke. CONTINUUM: Lifelong Learn Neurol. 2020;26(2):268–86. https://doi.org/10.1212/CON.0000000000000840.
Naik A, Adeleye O, Koester SW, et al. Cerebrospinal fluid biomarkers for diagnosis and the prognostication of Acute ischemic stroke: a systematic review. IJMS. 2023;24(13):10902. https://doi.org/10.3390/ijms241310902.
Ng GJL, Quek AML, Cheung C, Arumugam TV, Seet RCS. Stroke biomarkers in clinical practice: a critical appraisal. Neurochem Int. 2017;107:11–22. https://doi.org/10.1016/j.neuint.2017.01.005.
Chumachenko MS, Waseem TV, Fedorovich SV. Metabolomics and metabolites in ischemic stroke. Rev Neurosci. 2022;33(2):181–205. https://doi.org/10.1515/revneuro-2021-0048.
Khoshnam SE, Winlow W, Farzaneh M, Farbood Y, Moghaddam HF. Pathogenic mechanisms following ischemic stroke. Neurol Sci. 2017;38(7):1167–86. https://doi.org/10.1007/s10072-017-2938-1.
Vidale S, Consoli A, Arnaboldi M, Consoli D. Postischemic inflammation in Acute Stroke. J Clin Neurol. 2017;13(1):1. https://doi.org/10.3988/jcn.2017.13.1.1.
Elsayed WM, Abdel-Gawad EHA, Mesallam DIA, El-Serafy TS. The relationship between oxidative stress and acute ischemic stroke severity and functional outcome. Egypt J Neurol Psychiatry Neurosurg. 2020;56(1):74. https://doi.org/10.1186/s41983-020-00206-y.
Wicks EE, Ran KR, Kim JE, Xu R, Lee RP, Jackson CM. The translational potential of Microglia and Monocyte-Derived macrophages in ischemic stroke. Front Immunol. 2022;13:897022. https://doi.org/10.3389/fimmu.2022.897022.
Tuo Q, Zhang S, Lei P. Mechanisms of neuronal cell death in ischemic stroke and their therapeutic implications. Med Res Rev. 2022;42(1):259–305. https://doi.org/10.1002/med.21817.
Jang C, Chen L, Rabinowitz JD. Metabolomics and isotope tracing. Cell. 2018;173(4):822–37. https://doi.org/10.1016/j.cell.2018.03.055.
Johnson CH, Ivanisevic J, Siuzdak G. Metabolomics: beyond biomarkers and towards mechanisms. Nat Rev Mol Cell Biol. 2016;17(7):451–9. https://doi.org/10.1038/nrm.2016.25.
Cui L, Lu H, Lee YH. Challenges and emergent solutions for LC-MS/MS based untargeted metabolomics in diseases. Mass Spectrom Rev. 2018;37(6):772–92. https://doi.org/10.1002/mas.21562.
Alves S, Paris A, Rathahao-Paris E. Mass spectrometry-based metabolomics for an in-depth questioning of human health. Adv Clin Chem. 2020;99:147–91. https://doi.org/10.1016/bs.acc.2020.02.009.
Muiño E, Fernández-Cadenas I, Arboix A. Contribution of Omic studies to the understanding of Cadasil. Syst Rev IJMS. 2021;22(14):7357. https://doi.org/10.3390/ijms22147357.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from Ningbo Natural Science Foundation (2023J019), Ningbo Top Medical and Health Research Program (2022020304), Key Laboratory of Precision Medicine for Atherosclerotic Diseases of Zhejiang Province (2022E10026).
Author information
Authors and Affiliations
Contributions
Conceptualization, X.G. and Y.H.; methodology, L.W., S.C., X.D., Y.L., H.W; writing—original draft preparation, L.W.; writing—review and editing, Y.H. and X.G.; project administration, Y.H.; funding acquisition, X.G. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, L., Chen, S., Deng, X. et al. Metabolomic discoveries for early diagnosis and traditional Chinese medicine efficacy in ischemic stroke. Biomark Res 12, 63 (2024). https://doi.org/10.1186/s40364-024-00608-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40364-024-00608-7