Abstract
Background
Neoadjuvant chemotherapy (NAC) is increasingly used in locally advanced gastric cancer (LAGC), but the clinical safety and efficacy are still controversial. This study aims to compare perioperative chemotherapy (PEC) with adjuvant chemotherapy (AC) for resectable LAGC.
Methods
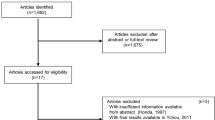
Patients who underwent D2 gastrectomy for resectable LAGC were retrospectively reviewed, and divided into NSA group (NAC plus surgery and AC) and SA group (surgery followed by AC). The baseline characteristics and perioperative data were compared. Survival analysis was based on Kaplan–Meier method. Multivariate analyses for prognostic factors were based on the Cox regression.
Results
A total of 450 patients were eligible for this study. 218 patients received NAC plus surgery and AC, while 232 upfront surgery followed by AC. The baseline characteristics were comparable between the two groups. NSA group showed significant superiority in R0 resection rate (P = 0.014), excised tumor size (P = 0.038), and tumor downstage (all P < 0.001). NAC did not affect postoperative complications or AC-related grade 3/4 adverse events. Patients in NSA group achieved significantly longer OS (P = 0.021) and DFS (P = 0.002). The Cox regression model showed that NAC was independently associated with better OS (HR 0.245, P = 0.039) and DFS (HR 0.591, P = 0.031).
Conclusions
Compared with SA, the administration of NSA was considered safe and feasible for achieving higher R0 resection rate without increasing the postoperative complications or AC-related grade 3/4 adverse events, and NAC was independently associated with better OS and DFS for resectable LAGC.
Similar content being viewed by others
Introduction
Gastric cancer (GC) is the fifth most frequently diagnosed malignancy, accounting for the third leading cause of cancer-related death worldwide [1]. Due to the lack of typical clinical symptoms in early GC, most patients have progressed to the advanced stage at the initial diagnosis [26]. It was worth noting that there was no significant difference in postoperative outcomes and complications between the two groups. This result further confirmed the safety of the perioperative treatment pattern.
There have been currently no unified standard indications for the application of neoadjuvant chemotherapy in LAGC. The Japan Clinical Oncology Group suggested that LAGC patients with clinical T3/T4 and cN+ stage were suitable to receive neoadjuvant chemotherapy [27]. The indications of neoadjuvant chemotherapy for GC in the 2021 Chinese Society of Clinical Oncology (CSCO) guidelines were patients with clinical staging T3–4a and N+ stage [28]; whereas, the ESMO clinical practice guidelines recommended a wider range of indications for neoadjuvant chemotherapy (> cT1N0) [29]. Survival benefits might be brought to patients in the condition of formulating suitable criteria to select the right people and using individualized and suitable treatment. In addition, well-designed studies are required to explore effective chemotherapy regimens and cycles. Precise staging and timely identification of the pathological response would lead to either an intensification of the neoadjuvant strategy in responding patients or to consider surgical treatment in the absence of clinical benefit.
We acknowledge that the present study contains certain limitations. Due to its retrospective nature and relatively limited number of patients at a single institution, potential selection bias and excessive hazard ratios in the analysis might exist. Second, even chemotherapy regimen was basically based on platinum drugs and 5-fluorouracil regimens, it was not standardized for NAC or AC, the effects of different regimens were not analyzed. Third, the patient cohort is a selected group (all had undergone resection and AC), and thus, the conclusion could not be extrapolated to all LAGC patients. Finally, our follow-up was relatively short. Despite the limitations above, the present study verified the superiority of perioperative chemotherapy for Asian patients with LAGC to a certain extent.
Conclusions
Compared with SA, the administration of NSA was considered safe and feasible for achieving higher R0 resection rate without increasing the postoperative complications or AC-related grade 3/4 adverse events, and NAC was independently associated with better OS and DFS for resectable LAGC. Our findings are expected to be supported by more high-quality prospective data.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
**e Y, Shi L, He X, Luo Y. Gastrointestinal cancers in China, the USA, and Europe. Gastroenterol Rep. 2021;9:91–104.
Yang W, Hu R, Li G-C, Zhou M-L, Wang Y, Shen L-J, et al. Survival outcomes and patterns of failure after D2 dissection and adjuvant chemoradiotherapy for locally advanced gastric cancer: a retrospective study. Br J Radiol. 2018;91:20170594.
Noh S, Park S, Yang H, Chung H, Chung I, Kim S, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15:1389–96.
Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29:4387–93.
Cunningham D, Allum WH, Stenning SP, Thompson JN, de Velde C, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Wang X, Li S, Sun Y, Li K, Shen X, Xue Y, et al. The protocol of a prospective, multicenter, randomized, controlled phase III study evaluating different cycles of oxaliplatin combined with s-1 (SOX) as neoadjuvant chemotherapy for patients with locally advanced gastric cancer: RESONANCE-II trial. BMC Cancer. 2021;21:20.
Al-Batran SE, Homann N, Pauligk C, Goetze TO, Meiler J, Kasper S, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393:1948–57.
Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–30.
Smalley SR, Benedetti JK, Haller DG, Hundahl SA, Estes NC, Ajani JA, et al. Updated analysis of SWOG-directed intergroup study 0116: a phase III trial of adjuvant radiochemotherapy versus observation after curative gastric cancer resection. J Clin Oncol. 2012;30:2327–33.
Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29:1715–21.
Wang TB, Chen YT, Zhao LL, Zhou H, Wu CR, Zhang XJ, et al. The effect of neoadjuvant therapies for patients with locally advanced gastric cancer: a propensity score matching study. J Cancer. 2021;12:379–86.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Ajani JA, Bentrem DJ, Besh S, D’Amico TA, Das P, Denlinger C, et al. Gastric cancer, version 2.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2013;11:531–46.
Van Cutsem E, Dicato M, Geva R, Arber N, Bang Y, Benson A, et al. The diagnosis and management of gastric cancer: expert discussion and recommendations from the 12th ESMO/World Congress on Gastrointestinal Cancer, Barcelona, 2010. Ann Oncol. 2011;22(Suppl 5):v1-9.
National Cancer Institute. Common terminology criteria for adverse events, version 4.0 [Internet]. National Cancer Institute; 2009. https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/Archive/CTCAE_4.0_2009-05-29_QuickReference_8.5x11.pdf. Accessed 28 May 2009.
Ajani JA, Damico TA, Almhanna K, Bentrem DJ, Chao J, Das P, et al. Gastric cancer, version 3.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2016;14:1286–312.
Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–49.
van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. 2016;388:2654–64.
Cai Z, Yin Y, Shen C, Wang J, Yin XN, Chen ZX, et al. Comparative effectiveness of preoperative, postoperative and perioperative treatments for resectable gastric cancer: a network meta-analysis of the literature from the past 20 years. Surg Oncol. 2018;27:563–74.
Zhang XT, Liang H, Li ZY, Xue YW, Wang YN, Zhou ZW, et al. Perioperative or postoperative adjuvant oxaliplatin with S-1 versus adjuvant oxaliplatin with capecitabine in patients with locally advanced gastric or gastro-oesophageal junction adenocarcinoma undergoing D2 gastrectomy (RESOLVE): an open-label, superiority and non-inferiority, phase 3 randomised controlled trial. Lancet Oncol. 2021;22:1081–92.
Kang YK, Yook JH, Park YK, Lee JS, Kim YW, Kim JY, et al. PRODIGY: a phase III study of neoadjuvant docetaxel, oxaliplatin, and S-1 plus surgery and adjuvant S-1 versus surgery and adjuvant S-1 for resectable advanced gastric cancer. J Clin Oncol. 2021;39:2903–13.
Charruf AZ, Ramos MF, Pereira MA, Dias AR, de Castria TB, Zilberstein B, et al. Impact of neoadjuvant chemotherapy on surgical and pathological results of gastric cancer patients: a case-control study. J Surg Oncol. 2020;121:833–9.
Xu W, Wang LQ, Yan C, He CY, Lu S, Ni ZT, et al. Neoadjuvant chemotherapy versus direct surgery for locally advanced gastric cancer with serosal invasion (cT4NxM0): a propensity score-matched analysis. Front Oncol. 2021;11: 718556.
Cats A, Jansen E, van Grieken N, Sikorska K, Lind P, Nordsmark M, et al. Chemotherapy versus chemoradiotherapy after surgery and preoperative chemotherapy for resectable gastric cancer (CRITICS): an international, open-label, randomised phase 3 trial. Lancet Oncol. 2018;19:616–28.
Baiocchi GL, Giacopuzzi S, Reim D, Piessen G, da Costa PM, Reynolds JV, et al. Incidence and grading of complications after gastrectomy for cancer using the GASTRODATA registry: a European retrospective observational study. Ann Surg. 2020;272:807–13.
Fukagawa T, Katai H, Mizusawa J, Nakamura K, Sano T, Terashima M, et al. A prospective multi-institutional validity study to evaluate the accuracy of clinical diagnosis of pathological stage III gastric cancer (JCOG1302A). Gastric Cancer. 2018;21:68–73.
Wang FH, Zhang XT, Li YF, Tang L, Qu XJ, Ying JE, et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer, 2021. Cancer Commun (Lond). 2021;41:747–95.
Lordick F, Carneiro F, Cascinu S, Fleitas T, Haustermans K, Piessen G, et al. Gastric cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Pract Guidel. 2022;33:1005–20.
Acknowledgements
Not applicable.
Funding
This research was supported by National High Level Hospital Clinical Research Funding (Grant No. 2022-PUMCH-B-005). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
PS and JY designed the study and wrote the manuscript; LJ, YZ, TY and HH contributed to the patient material; PS, LJ, MC and CC collected the clinical data; WK and YL contributed to data analysis and validation. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Clinical data were gathered with written informed consent of patients according to a protocol reviewed and approved by the Institutional Review Board of Peking Union Medical College Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Su, P., Jiang, L., Zhang, Y. et al. Perioperative chemotherapy versus adjuvant chemotherapy treatment for resectable locally advanced gastric cancer: a retrospective cohort study. Eur J Med Res 28, 409 (2023). https://doi.org/10.1186/s40001-023-01400-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01400-3