Abstract
Background
In Alzheimer’s disease (AD), pathological changes may arise up to 20 years before the onset of dementia. This pre-dementia window provides a unique opportunity for secondary prevention. However, exposing non-demented subjects to putative therapies requires reliable biomarkers for subject selection, stratification, and monitoring of treatment. Neuroimaging allows the detection of early pathological changes, and longitudinal imaging can assess the effect of interventions on markers of molecular pathology and rates of neurodegeneration. This is of particular importance in pre-dementia AD trials, where clinical outcomes have a limited ability to detect treatment effects within the typical time frame of a clinical trial. We review available evidence for the use of neuroimaging in clinical trials in pre-dementia AD. We appraise currently available imaging markers for subject selection, stratification, outcome measures, and safety in the context of such populations.
Main body
Amyloid positron emission tomography (PET) is a validated in-vivo marker of fibrillar amyloid plaques. It is appropriate for inclusion in trials targeting the amyloid pathway, as well as to monitor treatment target engagement. Amyloid PET, however, has limited ability to stage the disease and does not perform well as a prognostic marker within the time frame of a pre-dementia AD trial. Structural magnetic resonance imaging (MRI), providing markers of neurodegeneration, can improve the identification of subjects at risk of imminent decline and hence play a role in subject inclusion. Atrophy rates (either hippocampal or whole brain), which can be reliably derived from structural MRI, are useful in tracking disease progression and have the potential to serve as outcome measures. MRI can also be used to assess comorbid vascular pathology and define homogeneous groups for inclusion or for subject stratification. Finally, MRI also plays an important role in trial safety monitoring, particularly the identification of amyloid-related imaging abnormalities (ARIA). Tau PET to measure neurofibrillary tangle burden is currently under development. Evidence to support the use of advanced MRI markers such as resting-state functional MRI, arterial spin labelling, and diffusion tensor imaging in pre-dementia AD is preliminary and requires further validation.
Conclusion
We propose a strategy for longitudinal imaging to track early signs of AD including quantitative amyloid PET and yearly multiparametric MRI.
Similar content being viewed by others
Background
Alzheimer’s disease (AD) is the leading cause of dementia worldwide and it is pathologically characterised by the deposition of extracellular β-amyloid plaques and intracellular neurofibrillary tangles of hyperphosphorylated tau proteins [1]. Pathological changes may start up to 20 years before the onset of symptoms [2,3,4,5]. To date, treatments have only been approved for the dementia stage of the disease and provide modest symptomatic benefit but no slowing of progression. A global research priority is to find therapies to prevent or delay symptom onset and functional decline [6], and a number of candidate agents have shown promise in cell or animal models. Despite this, clinical trials of potential disease-modifying treatments have proven unsuccessful thus far. This may be partly due to limitations of the treatments (e.g. incorrect molecular target or inadequate target engagement, dose, or duration). However, the failures could also reflect inappropriate trial populations. Typically, trials have recruited patients with mild to moderate dementia in whom the disease process may be too advanced to be amenable to treatment. An alternative approach is to treat subjects at risk of AD dementia, which is the aim of secondary prevention—preventing neurodegeneration, cognitive decline, and dementia [7, 8].
Research criteria from the International Working Group (IWG) [9, 10] and the National Institute on Ageing-Alzheimer Association (NIA-AA) [11,12,13] propose the use of biomarkers to define pre-clinical AD as the disease stage characterised by amyloid pathology, with or without neurofibrillary tangles and/or features of neurodegeneration, even in the absence of clinical manifestations. Mild cognitive impairment (MCI) is used to denote an intermediate stage between normal cognition and dementia in which subjects have objective cognitive impairment in the absence of functional disability interfering with daily activities. MCI with biomarker evidence of AD has been termed prodromal AD under the IWG criteria [9, 10] and MCI due to AD by the NIA-AA in 2011 [12], but the 2018 research framework does not take into account syndromic diagnosis [11]. Non-demented subjects with evidence of amyloid pathology, i.e. subjects with AD without dementia [14], provide an opportunity for intervention prior to irreversible neuronal loss. Designing trials for subjects in pre-dementia stages of AD is greatly facilitated by the ability to identify subjects at increased risk of cognitive decline and progression to dementia. In the earliest stage, neuropsychological testing to detect subtle cognitive abnormalities in the absence of obvious symptoms has some predictive value [15], but biomarkers that are sensitive to underlying pathological change could further increase prognostic accuracy. Ideally, early-stage biomarkers should predict risk and likely timing of cognitive decline and progression to dementia in a reliable, non-invasive, and cost-effective manner. Secondly, trials in non-demented subjects would benefit from biomarkers that can monitor treatment effects and should thus reflect disease progression, be sensitive to detect pathologically significant changes over time and in response to treatment, and be highly reproducible and reliable in a multi-centre setting. Neuroimaging techniques have developed rapidly over the past decade and they currently offer a comprehensive armamentarium that can be employed to address this unmet need. Over and above structural neuroimaging markers that are widely available and used to support AD diagnosis at the dementia stage, advances in imaging techniques allow the detection and quantification of molecular, functional, and structural brain changes that precede gross atrophy.
In this paper, we discuss the use of neuroimaging markers in subject selection for inclusion or stratification in secondary prevention trials, their potential to serve as outcome markers in trials, and for monitoring trial safety. The overall aim is to devise a neuroimaging strategy that will maximise the information required to enrol and monitor secondary prevention trials in AD (including progression from MCI to dementia). To identify potential imaging markers, a comprehensive review of the existing literature was performed. Based on the evidence from the literature and the personal experience of the authors, recommendations are centred around three domains: 1) imaging markers for subject selection and stratification; 2) imaging markers with potential to be used as outcome measures in clinical trials; and 3) imaging markers for monitoring trial safety. The utility of longitudinal imaging as a run-in for clinical trials, identification of exclusion criteria, and vascular comorbidity were also taken into account.
Methods
Neuroimaging modalities: from molecular changes to structural damage
The past two decades have seen major advances in neuroimaging. Different imaging modalities are now able to track different aspects of the hypothesised pathological cascade of events in AD in vivo [3] (Box 1, Figs. 1, and 2). Positron emission tomography (PET) with amyloid-specific tracers, and more recently also tau-binding ligands, can visualise and quantify molecular pathology at an early stage. Alterations in functional imaging biomarkers, reflecting early synaptic dysfunction and neuronal injury, can be measured with various PET and magnetic resonance imaging (MRI) measures. Collectively, molecular and functional changes may lead to synaptic loss, inflammation, white matter damage, and neuronal cell death, eventually leading to macroscopic changes such as regional and global brain atrophy seen on structural MRI. Increasing evidence demonstrates that cerebrovascular changes have an additive effect on neurodegeneration, accelerate cognitive decline and progression to dementia, and may even be part of the pathological cascade of AD [16,17,18]; hence, we also address MRI markers of vascular pathology.
PET imaging biomarkers. Examples of normal (top) and abnormal (bottom) positron emission tomography (PET) imaging markers in three different subjects. For all images, the warmer the colour, the more tracer binding. Left: amyloid PET with [18F]-flutemetamol. In the abnormal scan, diffuse tracer binding to fibrillary amyloid can be observed. Middle: tau PET with [18F]-AV-1451. In the abnormal scan, tracer binding to tau can be observed in the temporal lobes. Right: Fluorodeoxyglucose (FDG)-PET scan. In the abnormal scan, there is hypometabolism of the parietal lobes
MRI imaging biomarkers. Left: T1-weighted MRI (top) showing severe hippocampal atrophy and example of diffusion tensor imaging (DTI) (bottom). Middle: example of functional imaging markers with arterial spin labelling (ASL) (top) and resting state functional magnetic resonance imaging (rs-fMRI) (bottom). Right: imaging of vascular pathology with thalamus lacune on T2 (top; arrow) and white matter hyper-intensities on fluid attenuated inversion recovery (FLAIR) (bottom)
Search strategy and selection criteria
References for this review were identified by searching the PubMed/Medline database in August 2017. Relevant articles were identified using the following search terms alone and in varying combinations: “amyloid PET”, “tau PET”, “MRI”, “structural MRI”, “functional MRI”, “FDG PET”, “fluorodeoxyglucose PET”, “TSPO PET”, “diffusion tensor imaging”, “arterial spin labeling”, “magnetic resonance spectroscopy”, “cognitively healthy”, “normal cognition”, “mild cognitive impairment”, “subjective cognitive decline”, “Alzheimer’s disease”. Papers published in English were included. Further references were obtained by screening references from retrieved articles and on the basis of the personal knowledge of the authors. In the case of topics already extensively covered in the literature, as was often the case for MCI, a reference article or review was selected by the authors. The final selection of articles was based on relevance to the topics covered in this review, as judged by the authors
Subject selection and stratification
Various planned and ongoing clinical trials for AD primarily target the amyloid cascade, aiming at the removal of amyloid plaques or prevention of misfolding of amyloid into the β conformation [19]. We recommend that trials targeting the amyloid pathway should include methods to recruit subjects with evidence of an appropriate level of amyloid pathology. Various PET tracers are capable of measuring and spatially localising β-amyloid deposits. Alternatively, β-amyloid peptides may be measured in cerebrospinal fluid (CSF). Studies have demonstrated good concordance between CSF β-amyloid 1–42 and amyloid PET measures, even though these markers might represent different pools of amyloid in the brain [20]. Several studies suggest that CSF β-amyloid levels become abnormal prior to an amyloid PET signal [21,22,1: Table S1). Imaging changes associated with other neurodegenerative disorders are, however, unlikely to be present in the early stages, which may preclude the reliable exclusion of these subjects.
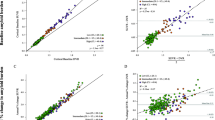
Step-wise approach for subject inclusion and testing. Information from clinical measurements (and, in the near future, possibly also plasma) may be used to select subjects with an increased risk of amyloid pathology (screening). Provided there are no exclusion criteria, molecular measurements of amyloid (or tau, depending on the treatment target) can be used to screen-in subjects for clinical trials. Finally, imaging measures predicting imminent cognitive decline may be used for additionally enrichment. APOE apolipoprotein E, CSF cerebrospinal fluid, MRI magnetic resonance imaging, PET positron emission tomography
Structural and functional imaging markers can also be used to identify subjects at risk of imminent cognitive decline, which will be reviewed in the following paragraphs. This is especially relevant for phase 3 trials in subjects with pre-clinical AD targeting cognition as a primary outcome. Enrichment of clinical trials targeting clinical end-points by means of amyloid PET and/or MRI may reduce sample sizes and costs, as shown in subjects with MCI [27, 28], but this work needs to be extended to the pre-clinical phase. Table 1 summarises the available evidence for the use of different imaging markers for subject selection in clinical trials.
Molecular imaging
Amyloid PET: predictor of decline?
Amyloid pathology measured with PET is an established prognostic marker in subjects with MCI (sensitivity 82% (95% confidence interval (CI) 74–88) and specificity 56% (95% CI 49–64) to distinguish stable MCI patients from those who progress to dementia) [29]. In cognitively normal subjects, amyloid positivity has been associated with an increased risk of cognitive decline and progression to dementia in several longitudinal studies [30,31,32,33,34,35,36,37,38,39,40,41], although studies with sufficiently long follow-up and large sets of data to establish the exact risk are required [40,41,42,43] (Table 2). The method of choice to classify subjects as amyloid-positive or amyloid-negative remains a matter of debate (Box 2). Recent evidence has also suggested that amyloid plaques might follow consistent deposition patterns in different regions of the brain, making it possible to stage amyloid pathology [44]. Although the relationship between amyloid positivity and later cognitive decline in cognitively normal subjects has been established, it has been suggested that the rate at which this occurs depends on the presence of neurodegeneration [45, 46]. Amyloid positivity is also consistently associated with increased brain atrophy rates in cognitively normal subjects (Additional file 1: Table S2). Hence, amyloid pathology is a necessary factor to assess whether an individual will decline due to AD pathology but is not sufficient to stage disease, or to predict when and how fast the decline will occur, since the timing depends on the rate of neurodegeneration [41, 46,47,8]).
Structural imaging
Grey matter atrophy
Patients with AD dementia show a pattern of widespread cerebral atrophy. Measures of global cortical atrophy have been used as an outcome marker in clinical trials in MCI and AD dementia (e.g. [172,173,174]). Besides global measures, regional changes can also be examined. Regional changes in different brain regions will likely relate more or less strongly to changes in different cognitive instruments, depending on the cognitive domains they subserve [175].
Hippocampal atrophy rates are a good candidate to serve as an outcome marker in multi-centre clinical trials, as long as standardisation of image acquisition between centres, consistent within-subject scanner acquisition, and uniform post-processing methods are performed. Test-retest reliability of repeated manual and automated hippocampal measurements from the same scanner is usually high (test-retest variability 1–4%) [176, 177], but some algorithms are more robust than others [178]. Efforts to standardise the measurement of hippocampal volumetry in multi-centre studies have been undertaken and it is now standard practice for trials to employ single algorithms and centralised analysis [89, 179]. With the establishment of the Harmonised Protocol for hippocampal segmentation, there is a new gold standard against which automated measurement may be validated [180]. Variability between scanners using the same acquisition protocol and measurement algorithm is low [176]. However, the agreement in terms of absolute volumes varies with acquisition protocols and field strength. For example, change in voxel size can lead to systematic errors in the range of 5% for hippocampal volume [181]. Methods to correct for these variabilities are being investigated [86].
Using data from the Australian Imaging, Biomarker and Lifestyle (AIBL) study, a sample size of 384 subjects per arm was estimated to be needed to detect 25% slowing of hippocampal atrophy rates over 18 months in subjects with pre-clinical AD with a power of 80% [182]. These numbers will be larger when taking into account atrophy occurring with normal ageing, which should be considered [183]. Measures of hippocampal atrophy rates have already been used as (secondary) end-points in various clinical trials in MCI and mild AD dementia, with varying results [151].
Diffusion tensor imaging
To date, there is little evidence for the use of DTI measures in (multi-centre) clinical trials. Several studies have pointed to the variability of DTI measurements in multi-centre studies and the need for extensive site harmonisation and calibration prior to starting [184,185,186]. More work is needed on the optimisation of DTI measurements in multi-centre settings, which is now being addressed [187]. So far, longitudinal DTI measures have only sparsely been used as (secondary) outcomes in clinical trials [188].
Monitoring of side-effects
Amyloid-related imaging abnormalities
MRI scans play an important role in safety monitoring during clinical trials. An issue of particular importance in the Alzheimer’s field is the occurrence of amyloid-related imaging abnormalities (ARIA) that have emerged in several anti-amyloid immunotherapy trials [189], although ARIA also occurs spontaneously—including in placebo arms [190]. ARIA consists of ARIA-E (parenchymal oedema or sulcal effusion) with signal hyper-intensities on FLAIR, and ARIA-H (cerebral microbleeds or superficial siderosis) with hypo-intensity due to hemosiderin on T2*-weighted or susceptibility-sensitive pulse sequences (Fig. 4). Adequate training for radiological reads is recommended for both ARIA-E and ARIA-H to ensure reliable detection of subtle cases and to maximise consistency between raters [191]. Severity of ARIA-E can be rated using dedicated rating scales [192]. Central assessment of the images is recommended to guarantee quality control and to minimise differences in visual inspection and quantification.
The detection of ARIA-H is dependent on the pulse sequence contrast mechanism and parameters (e.g. echo time and slice thickness) as well as field strength [189]. The reported prevalence of microbleeds in AD dementia subjects ranges from 18% at 1 T to 71% at 7 T [193]. Since the presence of cerebral microbleeds confers a risk for future haemorrhage and development of ARIA, many trials limit the number of microbleeds at entry and monitor development of new microbleeds during the trial. A key consideration in the management of emergent ARIA cases during a trial is whether any clinical symptoms are associated with the radiological observations.
In pre-clinical AD populations, the baseline incidence and the frequency of spontaneous emergent ARIA is less well characterised than in clinically demented subjects, although one study observed a lower incidence than in MCI and AD dementia populations [194]. Although several large randomised clinical trials in pre-clinical AD populations have recently commenced, the ARIA findings are not yet available to the wider community.
Regulatory perspective
In 2011, following observations in the bapineuzumab trials [195] and recommendations from an Alzheimer’s Association Round Table workgroup [189], the US Food and Drug Administration (FDA) requested the adoption of ARIA-based exclusion and discontinuation criteria for amyloid-targeting therapies. These limited the enrolment to subjects with at most four microbleeds at baseline and defined minimum acquisition standards. Since that time, for non-amyloid targeting mechanisms or if the ARIA risk for a particular compound or mechanism has been discharged in earlier trials, these criteria have been relaxed in some trials. Nevertheless, these recommendations have become a de facto standard. Systematic data collection and comparison between 2D-T2* and more sensitive sequences (e.g. 3D susceptibility-weighted imaging) is lacking. A well-controlled head-to-head comparison of the above T2* sequence prescription with a more sensitive alternative sequence would further the field’s understanding of ARIA prevalence and evolution in the natural history and provide data to help establish meaningful and comparable cut-off criteria for these alternative sequences early in the disease course.
Conclusions and practical implementation
Neuroimaging allows visualisation of many aspects of the pathological cascade of AD, including the presence of (pre-clinical) molecular pathology and downstream functional and structural markers of neurodegeneration before the onset of dementia. Information derived from imaging can aid in identifying non-demented subjects with an increased risk of future cognitive decline and disease progression to be included in secondary prevention trials. Combining information on underlying Alzheimer’s pathology from amyloid PET (or CSF) with markers of neurodegeneration from structural MRI (or FDG-PET) provides the optimal strategy to identify subjects who are at highest risk of cognitive decline within the typical time frame of a clinical trial. Advanced functional and structural imaging techniques to predict cognitive decline at a pre-dementia stage hold promise but await further research and validation. Neuroimaging can help to characterise subjects in terms of comorbidities (e.g. cerebrovascular disease) or to define more homogeneous subgroups that can be used for stratification. Neuroimaging can also serve as a (secondary) outcome marker in trials. Amyloid PET can be used to assess target engagement for pharmacological compounds targeting the amyloid cascade, and structural imaging (or FDG-PET) can be used to assess possible treatment effects on neurodegeneration. Finally, imaging is crucial for monitoring safety and potential side effects, such as ARIA, during trials.
Trials in non-demented subjects are greatly facilitated by the establishment of a cohort of well-phenotyped subjects that can be included in clinical trials. This is an approach that has been taken by the European Prevention for Alzheimer’s Dementia (EPAD; http://ep-ad.org/) study [196]. Within EPAD, subjects at elevated risk for AD are identified from various parent cohorts throughout Europe and enrolled into a longitudinal observational cohort study to serve as a trial-readiness cohort for proof-of-concept intervention studies. In addition to screening subjects, this trial-readiness cohort also provides an opportunity to apply run-in designs in which pre-trial longitudinal imaging can be used to determine within-subject rates of change, which increases the statistical power to detect treatment effects and reduces required sample sizes [197].
There are no formal guidelines on the use of neuroimaging measures in such trial-readiness cohorts of non-demented subjects. Some experience has been gathered through longitudinal imaging from multi-centre studies with large cohorts such as ADNI, with a strong focus on the MCI and dementia stages, and more recently with the AIBL study, with a focus on cognitively normal subjects [198, 199]. In ADNI, the imaging protocol initially included structural MRI and a subgroup with amyloid PET, and was later complemented by FDG-PET and advanced MR techniques such as ASL, DTI, and rs-fMRI in ADNI-2. Subjects in ADNI-3 also undergo tau PET. In AIBL, the imaging protocol includes structural MRI and amyloid PET. Based on the literature reviewed in this paper, experience gained in other studies, and practical considerations, neuroimaging recommendations for the EPAD longitudinal cohort study have been formulated (Table 4). These recommendations are based on a combination of desired information richness, patient burden, stratification capabilities, and provision of run-in data for trials. The recommended core imaging protocol for the EPAD longitudinal cohort study consists of yearly MRI scans including isotropic 3D-T1 and 3D-FLAIR sequences, as well as a short 2D-T2W and 2D-T2* sequence to assess neurodegenerative and vascular pathology. Advanced sequences such as 3D-T2*/SWI, DTI, ASL, and rs-fMRI will be acquired in subsets of patients depending on site interest and experience with acquisition methodology. Centralised assessment of the scans will be performed to guarantee quality control and maximise consistency in visual rating scales and quantification. All subjects in EPAD will undergo lumbar puncture to assess amyloid pathology in CSF. A large subgroup will also undergo amyloid PET, financed through the sister project Amyloid Imaging to Prevent AD (AMYPAD; http://amypad.eu/). Amyloid PET was prioritised as molecular imaging based on its potential to confirm and localise amyloid pathology, its broad availability and standardisation, and given that the initial molecular targets in upcoming proof-of-concept trials will likely address the amyloid pathway. Static amyloid PET imaging is currently the most common approach in clinical trials. Dynamic imaging, however, may be preferable to determine the true binding potential rather than an SUVr that may be biased by the choice of the reference region and flow effects. This argument becomes more relevant for longitudinal imaging where changes can be small and in treatment trials where flow alterations may occur. In addition, data from the initial uptake of the tracer can be used as a proxy to measure cerebral blood flow. As FDG-PET would add an additional radiation dose, it has not been included in the EPAD imaging protocol. While tau PET imaging is emerging, current implementation is limited due to costs, availability, and lack of standardisation. Development and accessibility of tau PET is encouraged as a potentially more proximate biomarker and predictor of disease progression and as therapies targeting tau enter clinical trials.
Abbreviations
- AD:
-
Alzheimer’s disease
- AMYPAD:
-
Amyloid Imaging to Prevent Alzheimer’s Disease
- APOE:
-
Apolipoprotein E
- ARIA:
-
Amyloid-related imaging abnormalities
- ASL:
-
Arterial spin labelling
- CI:
-
Confidence interval
- CSF:
-
Cerebrospinal fluid
- DLB:
-
Lewy body dementia
- DTI:
-
Diffusion tensor imaging
- EPAD:
-
European Prevention for Alzheimer’s Dementia
- FDG:
-
Fluorodeoxyglucose
- FLAIR:
-
Fluid attenuated inversion recovery
- MCI:
-
Mild cognitive impairment
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- PiB:
-
Pittsburgh compound B
- rs-fMRI:
-
Resting state functional magnetic resonance imaging
- SUVr:
-
Standardised uptake value ratio
References
Scheltens P, Blennow K, Breteler MMB, de Strooper B, Frisoni GB, Salloway S, et al. Alzheimer’s disease. Lancet. 2016;388:505–17.
Villain N, Chételat G, Grassiot B, Bourgeat P, Jones G, Ellis KA, et al. Regional dynamics of amyloid-β deposition in healthy elderly, mild cognitive impairment and Alzheimer’s disease: a voxelwise PiB–PET longitudinal study. Brain. 2012;135:2126–39.
Jack CR, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207–16.
Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12:357–67.
Villeneuve S, Rabinovici GD, Cohn-Sheehy BI, Madison C, Ayakta N, Ghosh PM, et al. Existing Pittsburgh compound-B positron emission tomography thresholds are too high: statistical and pathological evaluation. Brain. 2015;138:2020–33.
Fox NC, Petersen RC. The G8 dementia research summit—a starter for eight? Lancet. 2013;382:1968–9.
Reiman EM, Langbaum JBS, Fleisher AS, Caselli RJ, Chen K, Ayutyanont N, et al. Alzheimer’s Prevention Initiative: a plan to accelerate the evaluation of presymptomatic treatments. J Alzheimers Dis. 2011;26(Suppl 3):321–9.
Sperling RA, Rentz DM, Johnson KA, Karlawish J, Donohue M, Salmon DP, et al. The A4 study: stop** AD before symptoms begin? Sci Transl Med. 2014;6:228fs13.
Dubois B, Feldman HH, Jacova C, DeKosky ST, Barberger-Gateau P, Cummings J, et al. Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS–ADRDA criteria. Lancet Neurol. 2007;6:734–46.
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13:614–29.
Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9.
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:280–92.
Visser PJ, Tijms B. Brain amyloid pathology and cognitive function: Alzheimer disease without dementia? JAMA. 2017;317:2285–7.
Mortamais M, Ash JA, Harrison J, Kaye J, Kramer J, Randolph C, et al. Detecting cognitive changes in preclinical Alzheimer’s disease: a review of its feasibility. Alzheimers Dement. 2017;13:468–92.
Jokinen H, Lipsanen J, Schmidt R, Fazekas F, Gouw AA, van der Flier WM, et al. Brain atrophy accelerates cognitive decline in cerebral small vessel disease: the LADIS study. Neurology. 2012;78:1785–92.
Prins ND, Scheltens P. White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol. 2015;11:157–65.
Lee S, Viqar F, Zimmerman ME, Narkhede A, Tosto G, Benzinger TLS, et al. White matter hyperintensities are a core feature of Alzheimer’s disease: evidence from the dominantly inherited Alzheimer network. Ann Neurol. 2016;79:929–39.
Bachurin SO, Bovina EV, Ustyugov AA. Drugs in clinical trials for Alzheimer’s disease: the major trends. Med Res Rev. 2017;37:1186–225.
Roberts BR, Lind M, Wagen AZ, Rembach A, Frugier T, Li Q-X, et al. Biochemically-defined pools of amyloid-β in sporadic Alzheimer’s disease: correlation with amyloid PET. Brain. 2017;140:1486–98.
Mattsson N, Insel PS, Donohue M, Landau S, Jagust WJ, Shaw LM, et al. Independent information from cerebrospinal fluid amyloid-β and florbetapir imaging in Alzheimer’s disease. Brain. 2015;138:772–83.
Palmqvist S, Mattsson N, Hansson O. Alzheimer’s Disease Neuroimaging Initiative. Cerebrospinal fluid analysis detects cerebral amyloid-β accumulation earlier than positron emission tomography. Brain. 2016;139:1226–36.
Schindler SE, Gray JD, Gordon BA, **ong C, Batrla-Utermann R, Quan M, et al. Cerebrospinal fluid biomarkers measured by Elecsys assays compared to amyloid imaging. Alzheimers Dement. 2018.
Insel PS, Palmqvist S, Mackin RS, Nosheny RL, Hansson O, Weiner MW, et al. Assessing risk for preclinical β-amyloid pathology with APOE, cognitive, and demographic information. Alzheimers Dement. 2016;4:76–84.
Nakamura A, Kaneko N, Villemagne VL, Kato T, Doecke J, Doré V, et al. High performance plasma amyloid-β biomarkers for Alzheimer’s disease. Nature. 2018;554:249–54.
Nabers A, Perna L, Lange J, Mons U, Schartner J, Güldenhaupt J, et al. Amyloid blood biomarker detects Alzheimer’s disease. EMBO Mol Med. 2018;10:e8763.
Yu P, Sun J, Wolz R, Stephenson D, Brewer J, Fox NC, et al. Operationalizing hippocampal volume as an enrichment biomarker for amnestic mild cognitive impairment trials: effect of algorithm, test-retest variability, and cut point on trial cost, duration, and sample size. Neurobiol Aging. 2014;35:808–18.
Wolz R, Schwarz AJ, Gray KR, Yu P, Hill DLG. Alzheimer’s Disease Neuroimaging Initiative. Enrichment of clinical trials in MCI due to AD using markers of amyloid and neurodegeneration. Neurology. 2016;87:1235–41.
Frisoni GB, Bocchetta M, Chételat G, Rabinovici GD, de Leon MJ, Kaye J, et al. Imaging markers for Alzheimer disease: which vs how. Neurology. 2013;81:487–500.
Morris JC, Roe CM, Grant EA, Head D, Storandt M, Goate AM, et al. Pittsburgh compound B imaging and prediction of progression from cognitive normality to symptomatic Alzheimer disease. Arch Neurol. 2009;66:1469–75.
Storandt M, Mintun M, Head D, Morris J. Cognitive decline and brain volume loss as signatures of cerebral amyloid-β peptide deposition identified with Pittsburgh compound B: cognitive decline associated with aβ deposition. Arch Neurol. 2009;66:1476–81.
Resnick SM, Sojkova J, Zhou Y, An Y, Ye W, Holt DP, et al. Longitudinal cognitive decline is associated with fibrillar amyloid-beta measured by [11C]PiB. Neurology. 2010;74:807–15.
Villemagne VL, Pike KE, Chételat G, Ellis KA, Mulligan RS, Bourgeat P, et al. Longitudinal assessment of Aβ and cognition in aging and Alzheimer disease. Ann Neurol. 2011;69:181–92.
Lim YY, Ellis KA, Pietrzak RH, Ames D, Darby D, Harrington K, et al. Stronger effect of amyloid load than APOE genotype on cognitive decline in healthy older adults. Neurology. 2012;79:1645–52.
Lim YY, Maruff P, Pietrzak RH, Ames D, Ellis KA, Harrington K, et al. Effect of amyloid on memory and non-memory decline from preclinical to clinical Alzheimer’s disease. Brain. 2014;137:221–31.
Kawas CH, Greenia DE, Bullain SS, Clark CM, Pontecorvo MJ, Joshi AD, et al. Amyloid imaging and cognitive decline in nondemented oldest-old: the 90+ Study. Alzheimers Dement. 2013;9:199–203.
Doraiswamy PM, Sperling RA, Johnson K, Reiman EM, Wong TZ, Sabbagh MN, et al. Florbetapir F 18 amyloid PET and 36-month cognitive decline: a prospective multicenter study. Mol Psychiatry. 2014;19:1044–51.
Vemuri P, Lesnick TG, Przybelski SA, Knopman DS, Preboske GM, Kantarci K, et al. Vascular and amyloid pathologies are independent predictors of cognitive decline in normal elderly. Brain. 2015;138:761–71.
Petersen RC, Wiste HJ, Weigand SD, Rocca WA, Roberts RO, Mielke MM, et al. Association of elevated amyloid levels with cognition and biomarkers in cognitively normal people from the community. JAMA Neurol. 2016;73:85.
Donohue MC, Sperling RA, Petersen R, Sun C-K, Weiner MW, Aisen PS, et al. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA. 2017;317:2305–16.
Rowe CC, Bourgeat P, Ellis KA, Brown B, Lim YY, Mulligan R, et al. Predicting Alzheimer disease with β-amyloid imaging: results from the Australian imaging, biomarkers, and lifestyle study of ageing. Ann Neurol. 2013;74:905–13.
Ewers M, Insel P, Jagust WJ, Shaw L, Trojanowski JQ, Aisen P, et al. CSF biomarker and PIB-PET-derived beta-amyloid signature predicts metabolic, gray matter, and cognitive changes in nondemented subjects. Cereb Cortex. 2012;22:1993–2004.
Dickerson BC, Wolk DA, Alzheimer’s Disease Neuroimaging Initiative. Biomarker-based prediction of progression in MCI: comparison of AD signature and hippocampal volume with spinal fluid amyloid-β and tau. Front Aging Neurosci. 2013;5:55.
Grothe MJ, Barthel H, Sepulcre J, Dyrba M, Sabri O, Teipel SJ, et al. In vivo staging of regional amyloid deposition. Neurology. 2017;89:2031–8.
Wirth M, Villeneuve S, Haase CM, Madison CM, Oh H, Landau SM, et al. Associations between Alzheimer disease biomarkers, neurodegeneration, and cognition in cognitively normal older people. JAMA Neurol. 2013;70:1512–9.
Mormino EC, Betensky RA, Hedden T, Schultz AP, Amariglio RE, Rentz DM, et al. Synergistic effect of β-amyloid and neurodegeneration on cognitive decline in clinically normal individuals. JAMA Neurol. 2014;71:1379–85.
Jack CR, Lowe VJ, Weigand SD, Wiste HJ, Senjem ML, Knopman DS, et al. Serial PIB and MRI in normal, mild cognitive impairment and Alzheimer’s disease: implications for sequence of pathological events in Alzheimer’s disease. Brain. 2009;132:1355–65.
Vos SJ, **ong C, Visser PJ, Jasielec MS, Hassenstab J, Grant EA, et al. Preclinical Alzheimer’s disease and its outcome: a longitudinal cohort study. Lancet Neurol. 2013;12:957–65.
Braak H, Braak E. Evolution of the neuropathology of Alzheimer’s disease. Acta Neurol Scand. 1996;94:3–12.
Desikan RS, McEvoy LK, Thompson WK, Holland D, Brewer JB, Aisen PS, et al. Amyloid-β--associated clinical decline occurs only in the presence of elevated P-tau. Arch Neurol. 2012;69:709–13.
Villemagne VL, Fodero-Tavoletti MT, Masters CL, Rowe CC. Tau imaging: early progress and future directions. Lancet Neurol. 2015;14:114–24.
Hall B, Mak E, Cervenka S, Aigbirhio FI, Rowe JB, O’Brien JT. In vivo tau PET imaging in dementia: pathophysiology, radiotracer quantification, and a systematic review of clinical findings. Ageing Res Rev. 2017;36:50–63.
Betthauser J, Cody KA, Zammit MD, Murali D, Converse AK, Barnhart TE, et al. In vivo characterization and quantification of neurofibrillary tau PET radioligand [18F]MK-6240 in humans from Alzheimer’s disease dementia to young controls. J Nucl Med jnumed. 2018:118.209650.
Schöll M, Lockhart SN, Schonhaut DR, O’Neil JP, Janabi M, Ossenkoppele R, et al. PET imaging of tau deposition in the aging human brain. Neuron. 2016;89:971–82.
Hanseeuw BJ, Betensky RA, Schultz AP, Papp KV, Mormino EC, Sepulcre J, et al. Fluorodeoxyglucose metabolism associated with tau-amyloid interaction predicts memory decline. Ann Neurol. 2017;81:583–96.
Mosconi L, Berti V, Glodzik L, Pupi A, De Santi S, de Leon MJ. Pre-clinical detection of Alzheimer’s disease using FDG-PET, with or without amyloid imaging. J Alzheimers Dis. 2010;20:843–54.
Arbizu J, Festari C, Altomare D, Walker Z, Bouwman F, Rivolta J, et al. Clinical utility of FDG-PET for the clinical diagnosis in MCI. Eur J Nucl Med Mol Imaging. 2018;45(9):1497–508.
Mosconi L, De Santi S, Li J, Tsui WH, Li Y, Boppana M, et al. Hippocampal hypometabolism predicts cognitive decline from normal aging. Neurobiol Aging. 2008;29:676–92.
Ewers M, Brendel M, Rizk-Jackson A, Rominger A, Bartenstein P, Schuff N, et al. Reduced FDG-PET brain metabolism and executive function predict clinical progression in elderly healthy subjects. Neuroimage Clin. 2014;4:45–52.
Chen Y, Wolk DA, Reddin JS, Korczykowski M, Martinez PM, Musiek ES, et al. Voxel-level comparison of arterial spin-labeled perfusion MRI and FDG-PET in Alzheimer disease. Neurology. 2011;77:1977–85.
Binnewijzend MAA, Kuijer JPA, Benedictus MR, van der Flier WM, Wink AM, Wattjes MP, et al. Cerebral blood flow measured with 3D pseudocontinuous arterial spin-labeling MR imaging in Alzheimer disease and mild cognitive impairment: a marker for disease severity. Radiology. 2013;267:221–30.
Chao LL, Buckley ST, Kornak J, Schuff N, Madison C, Yaffe K, et al. ASL perfusion MRI predicts cognitive decline and conversion from MCI to dementia. Alzheimer Dis Assoc Disord. 2010;24:19–27.
Xekardaki A, Rodriguez C, Montandon M-L, Toma S, Tombeur E, Herrmann FR, et al. Arterial spin labeling may contribute to the prediction of cognitive deterioration in healthy elderly individuals. Radiology. 2015;274:490–9.
Verfaillie SCJ, Adriaanse SM, Binnewijzend MAA, Benedictus MR, Ossenkoppele R, Wattjes MP, et al. Cerebral perfusion and glucose metabolism in Alzheimer’s disease and frontotemporal dementia: two sides of the same coin? Eur Radiol. 2015;25:3050–9.
Fällmar D, Haller S, Lilja J, Danfors T, Kilander L, Tolboom N, et al. Arterial spin labeling-based Z-maps have high specificity and positive predictive value for neurodegenerative dementia compared to FDG-PET. Eur Radiol. 2017;27(10):4237–46.
Scott CJ, Jiao J, Melbourne A, Schott JM, Hutton BF, Ourselin S. ASL-incorporated pharmacokinetic modelling of PET data with reduced acquisition time: application to amyloid imaging. Medical Image Computing and Computer-Assisted Intervention—MICCAI 2016. Cham: Springer; 2016. p. 406–13. Available from: https://springer.longhoe.net/chapter/10.1007/978-3-319-46726-9_47. [cited 2017 May 31]
Rostomian AH, Madison C, Rabinovici GD, Jagust WJ. Early 11C-PIB frames and 18F-FDG PET measures are comparable: a study validated in a cohort of AD and FTLD patients. J Nucl Med. 2011;52:173–9.
Hsiao I-T, Huang C-C, Hsieh C-J, Hsu W-C, Wey S-P, Yen T-C, et al. Correlation of early-phase 18F-florbetapir (AV-45/Amyvid) PET images to FDG images: preliminary studies. Eur J Nucl Med Mol Imaging. 2012;39:613–20.
Tiepolt S, Hesse S, Patt M, Luthardt J, Schroeter ML, Hoffmann K-T, et al. Early [(18)F]florbetaben and [(11)C]PiB PET images are a surrogate biomarker of neuronal injury in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2016;43:1700–9.
Barkhof F, Haller S, Rombouts SARB. Resting-state functional MR imaging: a new window to the brain. Radiology. 2014;272:29–49.
Sheline YI, Raichle ME, Snyder AZ, Morris JC, Head D, Wang S, et al. Amyloid plaques disrupt resting state default mode network connectivity in cognitively normal elderly. Biol Psychiatry. 2010;67:584–7.
Mormino EC, Smiljic A, Hayenga AO, Onami SH, Greicius MD, Rabinovici GD, et al. Relationships between beta-amyloid and functional connectivity in different components of the default mode network in aging. Cereb Cortex. 2011;21:2399–407.
Lim HK, Nebes R, Snitz B, Cohen A, Mathis C, Price J, et al. Regional amyloid burden and intrinsic connectivity networks in cognitively normal elderly subjects. Brain. 2014;137:3327–38.
Elman JA, Madison CM, Baker SL, Vogel JW, Marks SM, Crowley S, et al. Effects of beta-amyloid on resting state functional connectivity within and between networks reflect known patterns of regional vulnerability. Cereb Cortex. 2016;26:695–707.
Chhatwal JP, Schultz AP, Johnson KA, Hedden T, Jaimes S, Benzinger TLS, et al. Preferential degradation of cognitive networks differentiates Alzheimer’s disease from ageing. Brain. 2018;141:1486–500.
Bai F, **e C, Watson DR, Shi Y, Yuan Y, Wang Y, et al. Aberrant hippocampal subregion networks associated with the classifications of aMCI subjects: a longitudinal resting-state study. PLoS One. 2011;6:e29288.
Binnewijzend MAA, Schoonheim MM, Sanz-Arigita E, Wink AM, van der Flier WM, Tolboom N, et al. Resting-state fMRI changes in Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging. 2012;33:2018–28.
Wang Z, Liang P, Jia X, ** G, Song H, Han Y, et al. The baseline and longitudinal changes of PCC connectivity in mild cognitive impairment: a combined structure and resting-state fMRI study. PLoS One. 2012;7:e36838.
Serra L, Cercignani M, Mastropasqua C, Torso M, Spanò B, Makovac E, et al. Longitudinal changes in functional brain connectivity predicts conversion to Alzheimer’s disease. J Alzheimers Dis. 2016;51:377–89.
Jack CR, Wiste HJ, Vemuri P, Weigand SD, Senjem ML, Zeng G, et al. Brain beta-amyloid measures and magnetic resonance imaging atrophy both predict time-to-progression from mild cognitive impairment to Alzheimer’s disease. Brain. 2010;133:3336–48.
van Rossum IA, Vos SJB, Burns L, Knol DL, Scheltens P, Soininen H, et al. Injury markers predict time to dementia in subjects with MCI and amyloid pathology. Neurology. 2012;79:1809–16.
den Heijer T, Geerlings MI, Hoebeek FE, Hofman A, Koudstaal PJ, Breteler MMB. Use of hippocampal and amygdalar volumes on magnetic resonance imaging to predict dementia in cognitively intact elderly people. Arch Gen Psychiatry. 2006;63:57–62.
den Heijer T, van der Lijn F, Koudstaal PJ, Hofman A, van der Lugt A, Krestin GP, et al. A 10-year follow-up of hippocampal volume on magnetic resonance imaging in early dementia and cognitive decline. Brain. 2010;133:1163–72.
Martin SB, Smith CD, Collins HR, Schmitt FA, Gold BT. Evidence that volume of anterior medial temporal lobe is reduced in seniors destined for mild cognitive impairment. Neurobiol Aging. 2010;31:1099–106.
Burnham SC, Bourgeat P, Doré V, Savage G, Brown B, Laws S, et al. Clinical and cognitive trajectories in cognitively healthy elderly individuals with suspected non-Alzheimer’s disease pathophysiology (SNAP) or Alzheimer’s disease pathology: a longitudinal study. Lancet Neurol. 2016;15:1044–53.
Potvin O, Mouiha A, Dieumegarde L, Duchesne S. Alzheimer’s Disease Neuroimaging Initiative. Normative data for subcortical regional volumes over the lifetime of the adult human brain. NeuroImage. 2016;137:9–20.
Frankó E, Joly O, Alzheimer’s Disease Neuroimaging Initiative. Evaluating Alzheimer’s disease progression using rate of regional hippocampal atrophy. PLoS One. 2013;8:e71354.
Barnes J, Bartlett JW, van de Pol LA, Loy CT, Scahill RI, Frost C, et al. A meta-analysis of hippocampal atrophy rates in Alzheimer’s disease. Neurobiol Aging. 2009;30:1711–23.
Hill DLG, Schwarz AJ, Isaac M, Pani L, Vamvakas S, Hemmings R, et al. Coalition Against Major Diseases/European Medicines Agency biomarker qualification of hippocampal volume for enrichment of clinical trials in predementia stages of Alzheimer’s disease. Alzheimers Dement. 2014;10:421–429.e3.
de Flores R, La Joie R, Chételat G. Structural imaging of hippocampal subfields in healthy aging and Alzheimer’s disease. Neuroscience. 2015;309:29–50.
Csernansky JG, Wang L, Swank J, Miller JP, Gado M, McKeel D, et al. Preclinical detection of Alzheimer’s disease: hippocampal shape and volume predict dementia onset in the elderly. NeuroImage. 2005;25:783–92.
Apostolova LG, Mosconi L, Thompson PM, Green AE, Hwang KS, Ramirez A, et al. Subregional hippocampal atrophy predicts Alzheimer’s dementia in the cognitively normal. Neurobiol Aging. 2010;31:1077–88.
Achterberg HC, van der Lijn F, den Heijer T, Vernooij MW, Ikram MA, Niessen WJ, et al. Hippocampal shape is predictive for the development of dementia in a normal, elderly population. Hum Brain Mapp. 2014;35:2359–71.
Stoub TR, Bulgakova M, Leurgans S, Bennett DA, Fleischman D, Turner DA, et al. MRI predictors of risk of incident Alzheimer disease: a longitudinal study. Neurology. 2005;64:1520–4.
Smith CD, Chebrolu H, Wekstein DR, Schmitt FA, Jicha GA, Cooper G, et al. Brain structural alterations before mild cognitive impairment. Neurology. 2007;68:1268–73.
Younes L, Albert M, Miller MI. BIOCARD Research Team. Inferring changepoint times of medial temporal lobe morphometric change in preclinical Alzheimer’s disease. Neuroimage Clin. 2014;5:178–87.
Hall AM, Moore RY, Lopez OL, Kuller L, Becker JT. Basal forebrain atrophy is a presymptomatic marker for Alzheimer’s disease. Alzheimers Dement. 2008;4:271–9.
Tondelli M, Wilcock GK, Nichelli P, De Jager CA, Jenkinson M, Zamboni G. Structural MRI changes detectable up to ten years before clinical Alzheimer’s disease. Neurobiol Aging. 2012;33:825.e25–36.
Jack CR, Wiste HJ, Weigand SD, Knopman DS, Mielke MM, Vemuri P, et al. Different definitions of neurodegeneration produce similar amyloid/neurodegeneration biomarker group findings. Brain. 2015;138:3747–59.
Dickerson BC, Stoub TR, Shah RC, Sperling RA, Killiany RJ, Albert MS, et al. Alzheimer-signature MRI biomarker predicts AD dementia in cognitively normal adults. Neurology. 2011;76:1395–402.
Verfaillie SCJ, Tijms B, Versteeg A, Benedictus MR, Bouwman FH, Scheltens P, et al. Thinner temporal and parietal cortex is related to incident clinical progression to dementia in patients with subjective cognitive decline. Alzheimers Dement (Amst). 2016;5:43–52.
Chiang GC, Insel PS, Tosun D, Schuff N, Truran-Sacrey D, Raptentsetsang S, et al. Identifying cognitively healthy elderly individuals with subsequent memory decline by using automated MR temporoparietal volumes. Radiology. 2011;259:844–51.
Pettigrew C, Soldan A, Zhu Y, Wang M-C, Moghekar A, Brown T, et al. Cortical thickness in relation to clinical symptom onset in preclinical AD. Neuroimage Clin. 2016;12:116–22.
Araque Caballero MÁ, Klöppel S, Dichgans M, Ewers M, Initiative A’s DN. Spatial patterns of longitudinal gray matter change as predictors of concurrent cognitive decline in amyloid positive healthy subjects. J Alzheimers Dis. 2016;55:343–58.
Whitwell JL, Dickson DW, Murray ME, Weigand SD, Tosakulwong N, Senjem ML, et al. Neuroimaging correlates of pathologically defined subtypes of Alzheimer’s disease: a case-control study. Lancet Neurol. 2012;11:868–77.
Chua TC, Wen W, Slavin MJ, Sachdev PS. Diffusion tensor imaging in mild cognitive impairment and Alzheimerʼs disease: a review. Curr Opin Neurol. 2008;21:83–92.
Clerx L, Visser PJ, Verhey F, Aalten P. New MRI markers for Alzheimer’s disease: a meta-analysis of diffusion tensor imaging and a comparison with medial temporal lobe measurements. J Alzheimers Dis. 2012;29:405–29.
Molinuevo JL, Ripolles P, Simó M, Lladó A, Olives J, Balasa M, et al. White matter changes in preclinical Alzheimer’s disease: a magnetic resonance imaging-diffusion tensor imaging study on cognitively normal older people with positive amyloid β protein 42 levels. Neurobiol Aging. 2014;35:2671–80.
Racine AM, Adluru N, Alexander AL, Christian BT, Okonkwo OC, Oh J, et al. Associations between white matter microstructure and amyloid burden in preclinical Alzheimer’s disease: a multimodal imaging investigation. NeuroImage Clin. 2014;4:604–14.
Oishi K, Mielke MM, Albert M, Lyketsos CG, Mori S. The Fornix sign: a potential sign for Alzheimer’s disease based on diffusion tensor imaging. J Neuroimaging. 2012;22:365–74.
Zhuang L, Sachdev PS, Trollor JN, Kochan NA, Reppermund S, Brodaty H, et al. Microstructural white matter changes in cognitively normal individuals at risk of amnestic MCI. Neurology. 2012;79:748–54.
van Uden IWM, Tuladhar AM, van der Holst HM, van Leijsen EMC, van Norden AGW, de Laat KF, et al. Diffusion tensor imaging of the hippocampus predicts the risk of dementia; the RUN DMC study. Hum Brain Mapp. 2016;37:327–37.
Scola E, Bozzali M, Agosta F, Magnani G, Franceschi M, Sormani MP, et al. A diffusion tensor MRI study of patients with MCI and AD with a 2-year clinical follow-up. J Neurol Neurosurg Psychiatry. 2010;81:798–805.
Mielke MM, Okonkwo OC, Oishi K, Mori S, Tighe S, Miller MI, et al. Fornix integrity and hippocampal volume predict memory decline and progression to Alzheimer’s disease. Alzheimers Dement. 2012;8:105–13.
Douaud G, Menke RAL, Gass A, Monsch AU, Rao A, Whitcher B, et al. Brain microstructure reveals early abnormalities more than two years prior to clinical progression from mild cognitive impairment to Alzheimer’s disease. J Neurosci. 2013;33:2147–55.
Selnes P, Aarsland D, Bjørnerud A, Gjerstad L, Wallin A, Hessen E, et al. Diffusion tensor imaging surpasses cerebrospinal fluid as predictor of cognitive decline and medial temporal lobe atrophy in subjective cognitive impairment and mild cognitive impairment. J Alzheimers Dis. 2013;33:723–36.
Brueggen K, Barkhof F, Hausner L, Filippi M, Nestor PJ, Hauenstein K, et al. Basal forebrain and hippocampus as predictors of conversion to Alzheimer’s disease in patients with mild cognitive impairment—a multicenter DTI and volumetry study. J Alzheimers Dis. 2015;48:197–204.
Donaghy P, Thomas AJ, O’Brien JT. Amyloid PET imaging in Lewy body disorders. Am J Geriatr Psychiatry. 2015;23:23–37.
Smith R, Puschmann A, Schöll M, Ohlsson T, van Swieten J, Honer M, et al. 18F-AV-1451 tau PET imaging correlates strongly with tau neuropathology in MAPT mutation carriers. Brain. 2016;139:2372–9.
Barrio JR, Small GW, Wong K-P, Huang S-C, Liu J, Merrill DA, et al. In vivo characterization of chronic traumatic encephalopathy using [F-18]FDDNP PET brain imaging. Proc Natl Acad Sci. 2015;112:E2039–47.
Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I, et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 2014;128:755–66.
Barnes J, Whitwell J, Frost C, Josephs K, Rossor M, Fox N. Measurements of the amygdala and hippocampus in pathologically confirmed Alzheimer disease and frontotemporal lobar degeneration. Arch Neurol. 2006;63:1434–9.
Bastos-Leite AJ, van der FWM, van SECW, Staekenborg SS, Scheltens P, Barkhof F. The contribution of medial temporal lobe atrophy and vascular pathology to cognitive impairment in vascular dementia. Stroke. 2007;38:3182–5.
de Souza LC, Chupin M, Bertoux M, Lehéricy S, Dubois B, Lamari F, et al. Is hippocampal volume a good marker to differentiate Alzheimer’s disease from frontotemporal dementia? J Alzheimers Dis. 2013;36:57–66.
Harper L, Barkhof F, Scheltens P, Schott JM, Fox NC. An algorithmic approach to structural imaging in dementia. J Neurol Neurosurg Psychiatry. 2014;85:692–8.
Likeman M, Anderson VM, Stevens JM, Waldman AD, Godbolt AK, Frost C, et al. Visual assessment of atrophy on magnetic resonance imaging in the diagnosis of pathologically confirmed young-onset dementias. Arch Neurol. 2005;62:1410–5.
Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11:1006–12.
Vos S, van Rossum I, Burns L, Knol D, Scheltens P, Soininen H, et al. Test sequence of CSF and MRI biomarkers for prediction of AD in subjects with MCI. Neurobiol Aging. 2012;33:2272–81.
Besson FL, La Joie R, Doeuvre L, Gaubert M, Mézenge F, Egret S, et al. Cognitive and brain profiles associated with current neuroimaging biomarkers of preclinical Alzheimer’s disease. J Neurosci. 2015;35:10402–11.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–38.
Muñoz Maniega S, Chappell FM, Valdés Hernández MC, Armitage PA, Makin SD, Heye AK, et al. Integrity of normal-appearing white matter: influence of age, visible lesion burden and hypertension in patients with small-vessel disease. J Cereb Blood Flow Metab. 2017;37:644–56.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. Am J Neuroradiol. 1987;8:421–6.
Wahlund LO, Barkhof F, Fazekas F, Bronge L, Augustin M, Sjögren M, et al. A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke. 2001;32:1318–22.
Cordonnier C, van der Flier WM. Brain microbleeds and Alzheimer’s disease: innocent observation or key player? Brain. 2011;134:335–44.
Akoudad S, Wolters FJ, Viswanathan A, de Bruijn RF, van der Lugt A, Hofman A, et al. Association of cerebral microbleeds with cognitive decline and dementia. JAMA Neurol. 2016;73:934–43.
Meier IB, Gu Y, Guzaman VA, Wiegman AF, Schupf N, Manly JJ, et al. Lobar microbleeds are associated with a decline in executive functioning in older adults. Cerebrovasc Dis. 2014;38:377–83.
van Straaten ECW, Scheltens P, Knol DL, van Buchem MA, van Dijk EJ, Hofman PAM, et al. Operational definitions for the NINDS-AIREN criteria for vascular dementia: an interobserver study. Stroke. 2003;34:1907–12.
Ritchie K, Ropacki M, Albala B, Harrison J, Kaye J, Kramer J, et al. Recommended cognitive outcomes in preclinical Alzheimer’s disease: consensus statement from the European Prevention of Alzheimer’s Dementia project. Alzheimers Dement. 2017;13:186–95.
Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95.
Jack CR, Wiste HJ, Lesnick TG, Weigand SD, Knopman DS, Vemuri P, et al. Brain β-amyloid load approaches a plateau. Neurology. 2013;80:890–6.
Sojkova J, Beason-Held L, Zhou Y, An Y, Kraut MA, Ye W, et al. Longitudinal cerebral blood flow and amyloid deposition: an emerging pattern? J Nucl Med. 2008;49:1465–71.
Vlassenko AG, Mintun MA, **ong C, Sheline YI, Goate AM, Benzinger TLS, et al. Amyloid-beta plaque growth in cognitively normal adults: longitudinal [11C]Pittsburgh compound B data. Ann Neurol. 2011;70:857–61.
Chételat G, La Joie R, Villain N, Perrotin A, de La Sayette V, Eustache F, et al. Amyloid imaging in cognitively normal individuals, at-risk populations and preclinical Alzheimer’s disease. NeuroImage Clin. 2013;2:356–65.
Villemagne VL, Rowe CC, Barnham KJ, Cherny R, Woodward M, Bozinosvski S, et al. A randomized, exploratory molecular imaging study targeting amyloid β with a novel 8-OH quinoline in Alzheimer’s disease: the PBT2-204 IMAGINE study. Alzheimers Dement (N Y). 2017;3:622–35.
Schmidt ME, Chiao P, Klein G, Matthews D, Thurfjell L, Cole PE, et al. The influence of biological and technical factors on quantitative analysis of amyloid PET: points to consider and recommendations for controlling variability in longitudinal data. Alzheimers Dement. 2015;11:1050–68.
Fleisher AS, Joshi AD, Sundell KL, Chen Y-F, Kollack-Walker S, Lu M, et al. Use of white matter reference regions for detection of change in florbetapir positron emission tomography from completed phase 3 solanezumab trials. Alzheimers Dement. 2017;13(10):1117–24.
Villemagne VL, Ong K, Mulligan RS, Holl G, Pejoska S, Jones G, et al. Amyloid imaging with (18)F-florbetaben in Alzheimer disease and other dementias. J Nucl Med. 2011;52:1210–7.
Joshi AD, Pontecorvo MJ, Clark CM, Carpenter AP, Jennings DL, Sadowsky CH, et al. Performance characteristics of amyloid PET with florbetapir F 18 in patients with alzheimer’s disease and cognitively normal subjects. J Nucl Med. 2012;53:378–84.
Vandenberghe R, Adamczuk K, Dupont P, Laere KV, Chételat G. Amyloid PET in clinical practice: its place in the multidimensional space of Alzheimer’s disease. NeuroImage Clin. 2013;2:497–511.
van Berckel BNM, Ossenkoppele R, Tolboom N, Yaqub M, Foster-Dingley JC, Windhorst AD, et al. Longitudinal amyloid imaging using 11C-PiB: methodologic considerations. J Nucl Med. 2013;54:1570–6.
Cash DM, Rohrer JD, Ryan NS, Ourselin S, Fox NC. Imaging endpoints for clinical trials in Alzheimer’s disease. Alzheimers Res Ther. 2014;6:87.
Sevigny J, Chiao P, Bussière T, Weinreb PH, Williams L, Maier M, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537:50–6.
Chiotis K, Saint-Aubert L, Savitcheva I, Jelic V, Andersen P, Jonasson M, et al. Imaging in-vivo tau pathology in Alzheimer’s disease with THK5317 PET in a multimodal paradigm. Eur J Nucl Med Mol Imaging. 2016;43:1686–99.
Chiotis K, Saint-Aubert L, Rodriguez-Vieitez E, Leuzy A, Almkvist O, Savitcheva I, et al. Longitudinalchanges of tau PET imaging in relation to hypometabolism in prodromal and Alzheimer’s disease dementia. Mol Psychiatry. 2018;23:1666–1673.
Jack CR, Wiste HJ, Schwarz CG, Lowe VJ, Senjem ML, Vemuri P, et al. Longitudinal tau PET in ageing and Alzheimer’s disease. Brain. 2018;141:1517–28.
Li C, Götz J. Tau-based therapies in neurodegeneration: opportunities and challenges. Nat Rev Drug Discov. 2017;16(12):863–83.
Joshi A, Koeppe RA, Fessler JA. Reducing between scanner differences in multi-center PET studies. NeuroImage. 2009;46:154–9.
Schmidt ME, Matthews D, Andrews R, Mosconi L. Positron emission tomography in Alzheimer disease: diagnosis and use as biomarker endpoints. In: RA MA, editor. Translational neuroimaging: tools for CNS drug discovery, development and treatment: Academic Press; 2013. p. 131–74. Available from: http://www.sciencedirect.com/science/article/pii/B9780123869456000056. [cited 2015 Aug 20].
Chen K, Langbaum JBS, Fleisher AS, Ayutyanont N, Reschke C, Lee W, et al. Twelve-month metabolic declines in probable Alzheimer’s disease and amnestic mild cognitive impairment assessed using an empirically pre-defined statistical region-of-interest: findings from the Alzheimer’s Disease Neuroimaging Initiative. NeuroImage. 2010;51:654–64.
Baker LD. Exercise and memory decline. Alzheimers Dement. 2016;12:P220–1.
Chen Y, Wang DJJ, Detre JA. Test-retest reliability of arterial spin labeling with common labeling strategies. J Magn Reson Imaging. 2011;33:940–9.
Wu B, Lou X, Wu X, Ma L. Intra- and interscanner reliability and reproducibility of 3D whole-brain pseudo-continuous arterial spin-labeling MR perfusion at 3T. J Magn Reson Imaging. 2014;39:402–9.
Mutsaerts HJMM, Steketee RME, Heijtel DFR, Kuijer JPA, van Osch MJP, Majoie CBLM, et al. Inter-vendor reproducibility of pseudo-continuous arterial spin labeling at 3 Tesla. PLoS One. 2014;9:e104108.
Alsop DC, Detre JA, Golay X, Günther M, Hendrikse J, Hernandez-Garcia L, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2015;73:102–16.
Mutsaerts HJMM, van Osch MJP, Zelaya FO, Wang DJJ, Nordhøy W, Wang Y, et al. Multi-vendor reliability of arterial spin labeling perfusion MRI using a near-identical sequence: implications for multi-center studies. NeuroImage. 2015;113:143–52.
Biswal BB, Mennes M, Zuo X-N, Gohel S, Kelly C, Smith SM, et al. Toward discovery science of human brain function. PNAS. 2010;107:4734–9.
Zuo X-N, Anderson JS, Bellec P, Birn RM, Biswal BB, Blautzik J, et al. An open science resource for establishing reliability and reproducibility in functional connectomics. Sci Data. 2014;1:140049.
Jovicich J, Minati L, Marizzoni M, Marchitelli R, Sala-Llonch R, Bartrés-Faz D, et al. Longitudinal reproducibility of default-mode network connectivity in healthy elderly participants: a multicentric resting-state fMRI study. NeuroImage. 2016;124:442–54.
Marchitelli R, Minati L, Marizzoni M, Bosch B, Bartrés-Faz D, Müller BW, et al. Test-retest reliability of the default mode network in a multi-centric fMRI study of healthy elderly: effects of data-driven physiological noise correction techniques. Hum Brain Mapp. 2016;37:2114–32.
Lorenzi MM, Beltramello A, Mercuri NB, Canu E, Zoccatelli G, Pizzini FB, et al. Effect of memantine on resting state default mode network activity in Alzheimer’s disease. Drugs Aging. 2012;28:205–17.
Solé-Padullés C, Bartrés-Faz D, Lladó A, Bosch B, Peña-Gómez C, Castellví M, et al. Donepezil treatment stabilizes functional connectivity during resting state and brain activity during memory encoding in Alzheimer’s disease. J Clin Psychopharmacol. 2013;33:199–205.
Fox NC, Black RS, Gilman S, Rossor MN, Griffith SG, Jenkins L, et al. Effects of Abeta immunization (AN1792) on MRI measures of cerebral volume in Alzheimer disease. Neurology. 2005;64:1563–72.
Quinn JF, Raman R, Thomas RG, Yurko-Mauro K, Nelson EB, Van Dyck C, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease. JAMA. 2010;304:1903–11.
Wilkinson D, Fox NC, Barkhof F, Phul R, Lemming O, Scheltens P. Memantine and brain atrophy in Alzheimer’s disease: a 1-year randomized controlled trial. J Alzheimers Dis. 2012;29:459–69.
McDonald CR, Gharapetian L, McEvoy LK, Fennema-Notestine C, Hagler DJ, Holland D, et al. Relationship between regional atrophy rates and cognitive decline in mild cognitive impairment. Neurobiol Aging. 2012;33:242–53.
Jovicich J, Czanner S, Han X, Salat D, van der Kouwe A, Quinn B, et al. MRI-derived measurements of human subcortical, ventricular and intracranial brain volumes: reliability effects of scan sessions, acquisition sequences, data analyses, scanner upgrade, scanner vendors and field strengths. NeuroImage. 2009;46:177–92.
Wonderlick JS, Ziegler DA, Hosseini-Varnamkhasti P, Locascio JJ, Bakkour A, van der Kouwe A, et al. Reliability of MRI-derived cortical and subcortical morphometric measures: effects of pulse sequence, voxel geometry, and parallel imaging. NeuroImage. 2009;44:1324–33.
Cover KS, van Schijndel RA, Versteeg A, Leung KK, Mulder ER, Jong RA, et al. Reproducibility of hippocampal atrophy rates measured with manual, FreeSurfer, AdaBoost, FSL/FIRST and the MAPS-HBSI methods in Alzheimer’s disease. Psychiatry Res. 2016;252:26–35.
Wolz R, Schwarz AJ, Yu P, Cole PE, Rueckert D, Jack CR Jr, et al. Robustness of automated hippocampal volumetry across magnetic resonance field strengths and repeat images. Alzheimers Dement. 2014;10:430–438.e2.
Frisoni GB, Jack CR Jr, Bocchetta M, Bauer C, Frederiksen KS, Liu Y, et al. The EADC-ADNI Harmonized Protocol for manual hippocampal segmentation on magnetic resonance: evidence of validity. Alzheimers Dement. 2015;11:111–25.
Haller S, Falkovskiy P, Meuli R, Thiran J-P, Krueger G, Lovblad K-O, et al. Basic MR sequence parameters systematically bias automated brain volume estimation. Neuroradiology. 2016;58:1153–60.
Andrews KA, Modat M, Macdonald KE, Yeatman T, Cardoso MJ, Leung KK, et al. Atrophy rates in asymptomatic amyloidosis: implications for Alzheimer prevention trials. PLoS One. 2013;8:e58816.
Fox NC, Ridgway GR, Schott JM. Algorithms, atrophy and Alzheimer’s disease: cautionary tales for clinical trials. NeuroImage. 2011;57:15–8.
Teipel SJ, Ewers M, Wolf S, Jessen F, Kölsch H, Arlt S, et al. Multicentre variability of MRI-based medial temporal lobe volumetry in Alzheimer’s disease. Psychiatry Res. 2010;182:244–50.
Zhu T, Hu R, Qiu X, Taylor M, Tso Y, Yiannoutsos C, et al. Quantification of accuracy and precision of multi-center DTI measurements: a diffusion phantom and human brain study. NeuroImage. 2011;56:1398–411.
Walker L, Curry M, Nayak A, Lange N, Pierpaoli C. the Brain Development Cooperative Group. A framework for the analysis of phantom data in multicenter diffusion tensor imaging studies. Hum Brain Mapp. 2013;34:2439–54.
Brueggen K, Grothe MJ, Dyrba M, Fellgiebel A, Fischer F, Filippi M, et al. The European DTI Study on Dementia—a multicenter DTI and MRI study on Alzheimer’s disease and mild cognitive impairment. NeuroImage. 2017;144:305–8.
Kilimann I, Likitjaroen Y, Hampel H, Teipel S. Diffusion tensor imaging to determine effects of antidementive treatment on cerebral structural connectivity in Alzheimer’s disease. Curr Pharm Des. 2013;19:6416–25.
Sperling RA, Jack CR, Black SE, Frosch MP, Greenberg SM, Hyman BT, et al. Amyloid-related imaging abnormalities in amyloid-modifying therapeutic trials: recommendations from the Alzheimer’s Association Research Roundtable Workgroup. Alzheimers Dement. 2011;7:367–85.
Carlson C, Siemers E, Hake A, Case M, Hayduk R, Suhy J, et al. Amyloid-related imaging abnormalities from trials of solanezumab for Alzheimer’s disease. Alzheimers Dement. 2016;2:75–85.
Arrighi HM, Barakos J, Barkhof F, Tampieri D, Jack C, Melançon D, et al. Amyloid-related imaging abnormalities-haemosiderin (ARIA-H) in patients with Alzheimer’s disease treated with bapineuzumab: a historical, prospective secondary analysis. J Neurol Neurosurg Psychiatr. 2016;87:106–12.
Barkhof F, Daams M, Scheltens P, Brashear HR, Arrighi HM, Bechten A, et al. An MRI rating scale for amyloid-related imaging abnormalities with edema or effusion. AJNR Am J Neuroradiol. 2013;34:1550–5.
Shams S, Wahlund L-O. Cerebral microbleeds as a biomarker in Alzheimer’s disease? A review in the field. Biomark Med. 2016;10:9–18.
Yates PA, Desmond PM, Phal PM, Steward C, Szoeke C, Salvado O, et al. Incidence of cerebral microbleeds in preclinical Alzheimer disease. Neurology. 2014;82:1266–73.
Salloway S, Sperling R, Gilman S, Fox NC, Blennow K, Raskind M, et al. A phase 2 multiple ascending dose trial of bapineuzumab in mild to moderate Alzheimer disease. Neurology. 2009;73:2061–70.
Ritchie CW, Molinuevo JL, Truyen L, Satlin A, Van der Geyten S, Lovestone S, et al. Development of interventions for the secondary prevention of Alzheimer’s dementia: the European Prevention of Alzheimer’s Dementia (EPAD) project. Lancet Psychiatry. 2016;3:179–86.
Frost C, Kenward MG, Fox NC. Optimizing the design of clinical trials where the outcome is a rate. Can estimating a baseline rate in a run-in period increase efficiency? Stat Med. 2008;27:3717–31.
Ellis KA, Bush AI, Darby D, De Fazio D, Foster J, Hudson P, et al. The Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging: methodology and baseline characteristics of 1112 individuals recruited for a longitudinal study of Alzheimer’s disease. Int Psychogeriatr. 2009;21:672–87.
Jack CR, Bernstein MA, Borowski BJ, Gunter JL, Fox NC, Thompson PM, et al. Update on the magnetic resonance imaging core of the Alzheimer’s disease neuroimaging initiative. Alzheimers Dement. 2010;6:212–20.
Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, Holt DP, et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–19.
Mathis CA, Mason NS, Lopresti BJ, Klunk WE. Development of positron emission tomography β-amyloid plaque imaging agents. Semin Nucl Med. 2012;42:423–32.
Schwarz AJ, Yu P, Miller BB, Shcherbinin S, Dickson J, Navitsky M, et al. Regional profiles of the candidate tau PET ligand 18F-AV-1451 recapitulate key features of Braak histopathological stages. Brain. 2016;139:1539–50.
Frisoni GB, Fox NC, Jack CR, Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6:67–77.
Weston PSJ, Simpson IJA, Ryan NS, Ourselin S, Fox NC. Diffusion imaging changes in grey matter in Alzheimer’s disease: a potential marker of early neurodegeneration. Alzheimers Res Ther. 2015;7:47.
Bartlett JW, Frost C, Mattsson N, Skillbäck T, Blennow K, Zetterberg H, et al. Determining cut-points for Alzheimer’s disease biomarkers: statistical issues, methods and challenges. Biomarkers Med. 2012;6:391–400.
Jack CR, Wiste HJ, Weigand SD, Therneau TM, Lowe VJ, Knopman DS, et al. Defining imaging biomarker cut points for brain aging and Alzheimer’s disease. Alzheimers Dement. 2017;13:205–16.
Yaqub M, Tolboom N, Boellaard R, van Berckel BNM, van Tilburg EW, Luurtsema G, et al. Simplified parametric methods for [11C]PIB studies. NeuroImage. 2008;42:76–86.
Acknowledgements
Not applicable.
Funding
This project has received support from the following EU/EFPIA Innovative Medicines Initiatives (1 and 2) Joint Undertakings: EPAD grant no. 115736, AMYPAD grant no. 115952, and EMIF grant no. 115372. FB was supported by the NIHR biomedical research centre at UCLH. ME was supported by an ERC career integration grant (PCIG12-GA-2012-334259), LMUexcellent and Alzheimer Forschung Initiative. JW was supported by research grants from Fondation Leducq, Medical Research Council, British Heart Foundation and Wellcome Trust.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
MtK and SI researched the literature and drafted the manuscript. AJS, NCF, GC, BNMvB, ME, CF, JDG, DH, MCI, AAL, JLM, CR, PS, MES, PJV, AW, JW, SH, and FB revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
AJS is a full-time employee of Takeda Pharmaceuticals. MCI is a stock-holding employee of Eli Lilly and Company. Florbetapir F18 is owned and marketed by Avid/Lilly. Flortaucipir (18F-AV-1451) is an investigational agent under development by Avid/Lilly. DH is a full-time employee and stockholder of IXICO plc. ME is a full-time employee of Janssen Pharmaceutica. CF is a full-time employee of GE Healthcare. The remaining authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Incidental findings on MRI. Table S2. Effect of amyloid on longitudinal MRI measures in cognitively normal subjects. (PDF 107 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
ten Kate, M., Ingala, S., Schwarz, A.J. et al. Secondary prevention of Alzheimer’s dementia: neuroimaging contributions. Alz Res Therapy 10, 112 (2018). https://doi.org/10.1186/s13195-018-0438-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-018-0438-z