Abstract
Background
Ultrasonography is a noninvasive modality for the initial assessment of thyroid nodules. The American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) has demonstrated good performance in differentiating malignant thyroid nodules. However, the combination of ACR TI-RADS categories and cytology has not been studied extensively, in Uganda. The study aims to correlate ACR TI-RADS with cytology among patients referred for US-guided fine-needle aspiration at Mulago National Referral Hospital.
Methods
This was a hospital-based cross-sectional study that recruited 132 patients with thyroid nodules. Spearman’s correlation was used to establish a relationship between TI-RADS and cytology findings. The diagnostic accuracy of TI-RADS was assessed using sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios.
Results
Of 132 study participants, 90% (n = 117) were females, and the mean age was 41 ± 13 years. One hundred sixty-one thyroid nodules were analyzed. More than half of the thyroid nodules (54.7%, n = 87) were solid or almost solid, 96.9% (n = 154) were shaped wider than tall, 57.2% (n = 91) had smooth margins, 83.7% (n = 133) were hyperechoic or isoechoic, and 88.7% (n = 141) had no echogenic foci. TI-RADS 3 was the most common at 42.9% (n = 69). The proportions of malignancy for TI-RADS 4 and TI-RADS 5 were 73.3% and 85.7%, respectively. The correlation between ACR TI-RADS and the Bethesda system of thyroid classification scores was r = 0.577. The sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios of ACR TI-RADS were 90.9%, 98.5%, 90%, 99.3%, 62.3, and 0.1, respectively.
Conclusion
We found that ACR TI-RADS classification is an appropriate and noninvasive method for assessing thyroid nodules in routine practice. It can safely reduce the number of unnecessary fine-needle aspiration in a significant proportion of benign thyroid lesions. Thyroid nodules classified as TI-RADS 3 should be followed routinely. ACR TI-RADS should be standardized as the screening tool in resource-limited areas.
Similar content being viewed by others
Background
Thyroid nodules (TNs) are a common thyroid disorder with a global prevalence ranging from 4–7% by palpation, 19–68% by ultrasound (US), and 8–65% by pathologic examination at autopsy [1, 2] This increase is thought to be related to early detection by high-resolution ultrasound and the discovery of subclinical TNs [3, 4] TNs can be classified as either benign or malignant. Most them are benign, and less than 5–10% are malignant [4]. In Africa, the prevalence of benign TNs is 89%, while that of malignant TNs stands at 11%, showing some variation from the expected global benign and malignant TNs percentages [5]. This could be due to the high prevalence of iodine deficiency goiter [6]. In Uganda, nodular thyroid disease is more common than diffuse thyroid disease, accounting for 82% of all patients referred with thyroid symptoms [7]. Furthermore, a study performed at Mulago National Referral Hospital (MNRH) found that 5% of the TNs evaluated were malignant, 18% were suspicious, and 75% were benign [7]. Hence, the need to identify suitable tools to assess the risk of malignancy in patients with TNs is crucial [8].
The differentiation of malignant and benign TNs of utmost importance in clinical evaluation since treatment is different for each type of nodule [9]. Ultrasound can be used to differentiate benign from malignant nodules based on certain characteristics [9]. To improve the diagnostic sensitivity and specificity of the ultrasound evaluation of TNs, the Thyroid Imaging Reporting and Data System (TI-RADS) was proposed [10]. The American College of Radiology Thyroid Imaging Reporting and Data Systems (ACR TI-RADS) is a 5-point classification system developed to determine the risk of cancer in TNs based on ultrasound characteristics. This system has been mainly used for TNs that are ≥ 1 cm. This system evaluates ultrasound features in five categories: composition, echogenicity, shape, margin, and echogenic foci; the nodule’s total points determine its risk level, which ranges from TI-RADS 1 (TR1) (benign) to TI-RADS 5 (TR5) (highly suspicious) [11]. None of these ultrasound features can be used in isolation to accurately differentiate benign from malignant TNs. Fine-needle aspiration (FNA) biopsy is the next critical step in the workup of a nodule after ultrasound identifies features that warrant biopsy [12]. The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) [13] was developed to standardize thyroid cytology diagnoses to convey the biopsy findings according to a classification system that provides clear management guidelines and the associated risk of malignancy [10]. ACR TI-RADS is relatively new [14] and has not been widely adopted for use in Uganda. Furthermore, the correlation of ACR TI-RADS with cytology has not been extensively studied in Uganda.
Age and sex correlate with the pathogenesis and increased prevalence of TNs [15, 16].
The incidence of nodules has been reported to be four times higher in women than in men [17]. This could be a result of hormonal influences of both estrogen and progesterone [18] Smoking, radiation exposure, pregnancy, multiparity, and abnormal body mass index ranges have also been identified as predisposing factors [19] Genetic factors, environmental influences, lifestyle, and access to medical care could be associated with variation in thyroid cancer incidence by geographic area and ethnicity [20]. Thyroid nodules are uncommonly cited in third world countries, where the disease is attributed to iodine deficiency disorders due to low salt consumption [21]. The study, therefore, sought to investigate the correlation of ACR TI-RADS with cytology among patients referred for US-guided FNA of thyroid nodules at MNRH.
Methods
Study design and setting
This was a hospital-based descriptive cross-sectional study conducted at the ultrasound unit of the Department of Radiology and Department of Pathology of MNRH, Kampala, Uganda, between November 2020 and March 2021. The radiology department provides wide imaging services, including US, computed tomography, plain radiography, and interventional radiology. It has eleven radiographers, five consultant radiologists, and four nurses. The department of pathology is situated at the School of Biomedical Science and serves the roles of teaching and research, as well as offering diagnostic histopathology/cytopathology and autopsy services. Most the patients referred for US-guided FNA are from the endocrine-surgical outpatient clinic at MNRH. The clinic runs every Wednesday from 8:00 AM to 2:00 PM and receives approximately 15–17 patients weekly.
Study population
All consenting participants with thyroid nodules ≥ 1 cm on B-mode ultrasound scans were scheduled for US-guided FNA. All participants were at the age of 18 and above during the study period. Participants with prolonged bleeding time, extensively calcified nodules, emphysema, and clinical and laboratory features of thyrotoxicosis were excluded from the study.
Sample size
The sample size was determined using Kish Leslie’s formula.
where:
N = desired sample size.
Z = Z score corresponding to 1.96 for 95% confidence level.
p = the estimated proportion of people with suspicious nodular thyroid sonography findings; 50% was used to obtain the maximum sample size
d = margin of error at the 95% level of significance, which is 0.05
Taking the prevalence of suspicious nodular thyroid sonographic findings as 50%, we obtained an approximate sample size of 385 participants.
The finite population correction formula was used to adjust the sample size before data collection since the accessible population was 200 patients for the duration of the study. The 200 participants were estimated by multiplying the number of FNA Referrals received per week [10] by 20 weeks (anticipated duration of the study).
Using the finite correction formula, the final adjusted sample size was 132 participants.
where:
S is the adjusted sample size.
Population size was the expected number of participants within the 5-month study period.
Study procedure
All patients referred from the endocrine-surgical outpatient clinic with TNs in a B-mode US scan scheduled for US-guided FNA during the study period were screened for nodules using US. Those with TNs ≥ 1 cm in B-mode US and who consented were recruited into the study. Under the supervision of a radiologist, The US evaluation was performed on an SIUI machine, model Apogee 5300, manufactured January 2015 by Hamburg Germany. Ultrasound machine with high-frequency linear probes of 7.5 MHz for obese patients or large thyroid lesions, a 5 MHz transducer was used for greater penetration. US was performed with the patient in the supine position and the neck hyperextended, and the entire gland was examined. Hyperextension of the neck was obtained by placing a pillow under the shoulders. The neck was scanned in sagittal, transverse, and oblique sections to optimally visualize both lobes of the thyroid and isthmus. Color Doppler imaging was utilized. Imaging of the lower poles of the thyroid was obtained by making the patient swallow as this tends to raise the thyroid gland in the neck.
Thyroid nodules sonographic characteristics, such as composition, shape, echogenicity, margins and echogenic foci, were recorded, and points were assigned to each nodule for separate categories according to ACR TI-RADS guidelines [11]. The sum of the points in each category determined the TI-RADS level assigned to each nodule, with TR1 indicating 0 points; TR2 – 2 points; TR3 – 3 points; TR4 – 4–6 points; and TR5 – 7 or more points (Fig. 1). The final sonographic diagnosis was reached with the help of a consultant radiologist. The data obtained from the ACR point table were used to correlate with cytology results. A 23-gauge needle with a clear hub and clear syringe (5–10 ml) was used to obtain a sample from each nodule, and a maximum of two nodules were sampled per patient. The sample was gently expelled onto the surface of a labeled microscope slide from the needle tip. A smearing slide was then slid over the specimen, ensuring that both slides were smeared. One slide underwent wet fixation with alcohol, which was stained using the Papanicolaou method, while the other slide was air-dried at room temperature and stained with the Diff quick method. After this, an experienced pathologist evaluated all samples according to the TBSRTC [13]. The categories and their risk of malignancy were recorded as follows in (Table 1).
Nomenclature of categorization of thyroid nodule features per the five lexicon categories [22]
The ACR TI-RADS level, which ranges from TR1 (benign) to TR5 (high suspicion of malignancy), was also used to categorize the nodules. Coded US images were stored and printed.
Statistical analysis
The data were entered into EpiData version 3.1 and then exported into Stata statistical software version 14 for analysis. To describe patient characteristics, categorical variables were summarized using frequencies and percentages, while continuous variables used the mean and standard deviation. While 132 patients were enrolled in the study, 29 of them had 2 or more nodules but only two nodules were biopsied, resulting in an analytic sample size of 161. Pairwise analysis was not performed to control for clustering because the patient identifiers were replaced with study numbers for the study purpose. The ACR TI-RADS classification criteria were used to classify nodules and then presented as frequencies and percentages. The difference in the proportions of the ACR TI-RADS sonographic criteria was tested using Fischer’s exact test. Spearman’s correlation coefficient was used to establish the correlation between ACRTI-RADS and cytology findings.
To determine the diagnostic effectiveness of ACR TI-RADS in characterizing thyroid nodules and predicting cytological findings, sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios with corresponding 95% confidence levels were calculated using the Bethesda system of thyroid classification as a gold standard. ACR TI-RADS was dichotomized by considering TR4 and TR5 as a positive screen for malignancy and TR1 to 3 as screen negative. The Bethesda System was also dichotomized by classifying 4 to 6 as malignancy and 1–3 as no malignancy.
Results
Of the 132 study participants, the majority were females (90%, n = 117) with a mean age of 41 ± 13. Twenty-nine (22%) had 2 or more nodules, but only two nodules were biopsied, giving a total sample size of 161. Of these, 2 nodules of 2 patients were inadequate and were excluded from the final analysis. Most of the participants were from the central region of Uganda, 74 (56.9%) (Table 2).
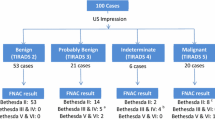
More than half of the nodules (87, 54.7%) had a composition that was mostly solid or almost solid, and 154 (96.9%) were shaped wider than tall. One hundred thirty-three (83.7%) of the nodules were hyperechoic/isoechoic, 60 (37.7%) had ill-defined margins, and 141 (88.7%) had no comet tail artifact or large comet tail artifacts (Table 3). Most of the nodules (69, 42.9%) were classified as TR3, followed by TR2 (56, 34.8%), 14 (8.7%) were classified as TR1 and 7 (4.3%) were classified as TR5. Furthermore, TR3 was the most frequently observed categorization in both males (42.9%) and females (44.1%) (Fig. 2).
Two (1.2%) of the nodules classified as Bethesda 1 and 141 (85.5%) classified as Bethesda II were considered benign, and 18 (11.2%) nodules classified as Bethesda 4–6 were considered malignant. Six nodules (3.7%) that were categorized as TR5 truly turned out to be malignant according to the Bethesda classification (Bethesda 6). Similarly, most of the nodules categorized as TR4 were suspicious for malignancy according to the Bethesda classification (Bethesda 5). One out of the 141 nodules characterized as TR5 on ultrasound was Riedel’s thyroiditis (Bethesda 2).
Moreover, one [1] out of the 69 nodules categorized as TR3 was classified as suspicious for follicular neoplasm (Bethesda classification 4). When comparing the ACR TI-RADS classification with the TBSRTC, the proportion of malignancy for TR1, 2, 3, 4, and 5 was 0, 0, 1.4, 73.3, and 85.7%, respectively. The risk of malignancy was determined by dividing total Bethesda scores from 4–6 by the total ACR TI-RADS level (Table 4). There was a moderate correlation between ACR TI-RADS and the Bethesda system of thyroid classification scores (r = 0.577), and this correlation was statistically significant (p < 0.001).
The sensitivity and specificity of ACR TI-RADS to detect malignancy were 94.4% with a 95% CI of 0.944 (0.8–1.0) and 96.5% with a 95% CI of 0.965 (0.9–0.99), respectively. The positive (PPV) and negative (NPV) predictive values corresponding to the above sensitivity and specificity were 77.3% and 99.3%, respectively, while the positive and negative likelihood ratios were 27 and 0.06, respectively (Table 5). Hypoechoic echogenicity and solid composition combined with hypoechoic echogenicity showed the highest sensitivity to detect malignancy of 54.6% and 57.1%, respectively. All the parameters used in the classification of ACR TI-RADS except for composition were statistically significantly associated with cytology results, p < 0.005. This significant association was noted for nodules that were either solid and hypoechoic or solid and hyperechoic (Table 6).
An US images of the TR3 and TR5 nodules with their corresponding categories of II (Benign follicular cells) and VI Bethesda system (papillary carcinoma) were shown in Figs. 3 and 4.
A Transverse sonogram of a well-defined wider than taller isoechoic solid nodule in the upper outer quadrant of the left lobe in 24-year-old women. It was classified as solid (composition score of 2), With 1 more point for iso-echogenicity and none in other categories, its total point was 3 (TR3). B Cytology result showing abundant thick colloid benign follicular cells (diff-quick, × 40) (category II bethesda system)
A A solid hypoechoic nodule with punctate calcification in an 63-year-old man. The nodule received 2 points for composition, 2 for being hypoechoic, and 3 for punctate calcification, for a total of 7 (TR5). B shows papillae lined by cells with marked enlarged, and crowded/overlapped nuclei (Diff-Quick,40) (papillary carcinoma-Category VI Bethesda system)
Discussion
This study sought to determine the correlation of ACR TI-RADS with TBSRTC among patients attending MNRH. We found high sensitivity and specificity of ACR TI-RADS to detect malignancy and a strong positive correlation between ACR TI-RADS and TBSRTC. Moreover, the majority of the nodules were classified as TR3 based on sonographic appearance, and the majority of the TNs referred for FNA were solid/almost solid, wider than tall, hyperechoic or isoechoic, had a smooth margin, and had no echogenic foci.
The study observed that the majority of the patients were females with an average age of early forties, which was consistent with other studies performed in Uganda [7], India [23], and Saudi Arabia [24] that reported a similar female to male ratio and average age. This can be explained by the fact that females are more prone to symptomatic thyroid nodular disease as a result of hormonal influences of estrogen and progesterone [25].
The sonographic appearance of thyroid nodules based on ACR TI-RADS demonstrated the majority to be solid or almost solid, wider than tall in appearance, smooth margins, hyperechoic or isoechoic and having no echogenic foci. These findings are consistent with features often seen on benign nodules. A cross-sectional study performed in India among 104 patients showed similar sonographic features on the thyroid gland nodules analyzed [26]. Another comparable study in the Philippines showed that the most frequent characteristics of nodules on US were solid in composition, isoechoic to hyperechoic, and wider than tall; however, few had well-circumscribed margins [27].
Of all the 161 nodules categorized based on ACR TI-RADS, approximately 42.9% were classified as TR3, followed by TR2, only less than 10% were TR4 and TR1, and the least common was TR5. Our findings and those from previous studies present a heterogeneous picture of ACR TI-RADS classification. For instance, a French study [28] observed a similar finding to ours, with the majority having TR3 nodules. However, a similar study from India reported TR2 as the most prevailing category [17] Regardless of these differences in ACR TI-RADS categorization, the majority of the nodules in these studies were still classified as benign nodules. Our study also observed that the risk of malignancy increased as the level of ACR TI-RADS categorization increased, from 0% in TR1 and TR2 to 73% and 86% in TR4 and TR5, respectively. These findings were consistent with studies from France [28] and South Korea [9].
Our study demonstrated a significant strong positive correlation between the ACR TI-RADS scoring of thyroid nodules and Bethesda System classification scores. Other studies have also found a strong correlation between the two methods [29]. In addition, the study found a high sensitivity (94%) and specificity (96%) with excellent PPV (77%) and MPV (99%). The ACR TI-RADS showed a positive likelihood ratio of 27 and a negative likelihood ratio of 0.06, which implies that ACR TI-RADS is moderately good at ruling in benign or malignant thyroid nodules and ruling out benign or malignant ones, respectively. The ACR TI-RADS was also statistically significantly associated with cytology results (p < 0.001). Compared to other studies, a study in India revealed a comparable sensitivity and specificity of over 90% [17]. The study, however, reported a lower PPV and similar NPV [17]. The low PPV in the Indian study is possibly due to a higher prevalence of thyroid malignancy compared to a lower prevalence in Uganda.
This study found hypoechogenicity on ultrasound to be a predictor of malignancy with a reduced sensitivity of 54.6% but increased specificity and positive and negative predictive values of over 90%. Similar studies that were performed in Sri Lanka [30] and India [31] also demonstrated similar findings. Furthermore, irregular margins as well as taller than wider shapes are also predictors of malignancy, albeit with a low sensitivity of 31.8%, while the specificity and positive and negative predictive values were almost 90%. Comparable findings were reported by the same study from India [31], who observed that poorly defined irregular margins had equally low sensitivity but high specificity and positive predictive value. These findings are also similar to a study reported by Jabar et al. that showed irregular margins and taller than wider appearances had low sensitivity and PPV and high specificity and NPV [32]. On the other hand, the French study [28] showed that taller than wide as a predictor for malignancy had a very low sensitivity, good specificity, and high PPV and NPV.
The study had some limitations. Analysis of intra-rater variability could not be conducted since the study did not have a control group, and patients could not be used as their controls due to the limited number of biopsies that can be tolerated by patients. Also, some of the study limitations were short sample size and dichotomization of the Bethesda System.
Since patients with only ultrasound scan results were included, these introduced selection bias. The use of two biopsies from a single participant may have introduced a clustering effect, which may have biased our findings.
Conclusion
We found that ACR TI-RADS is an appropriate and noninvasive method for assessing thyroid nodules in routine practice. This scoring system can safely reduce the number of unnecessary biopsies in a significant proportion of patients with benign thyroid lesions. Thyroid nodules classified as TR3 should be followed routinely. We recommend sonographic categorization of thyroid nodules using ACR TI-RADS in Uganda to create uniformity in reporting and easy guidance of appropriate biopsy.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACR:
-
American College of Radiology
- FNA:
-
Fine needle aspiration
- MNRH:
-
Mulago National Referral Hospital
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- TBSRTC:
-
The Bethesda System for Reporting Thyroid Cytopathology
- TNs:
-
Thyroid nodules
- TI-RADS:
-
Thyroid Imaging Reporting and Data System
- TR:
-
TI-RADS
- US:
-
Ultrasonography
References
Dean DS, Gharib H. Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab. 2008;22(6):901–11.
Al Dawish MA, Alwin Robert A, Thabet MA, Braham R. Thyroid nodule management: thyroid-stimulating hormone, ultrasound, and cytological classification system for predicting malignancy. Cancer informatics. 2018;17:1176935118765132.
Wiltshire JJ, Drake TM, Uttley L, Balasubramanian SP. Systematic review of trends in the incidence rates of thyroid cancer. Thyroid : official journal of the American Thyroid Association. 2016;26(11):1541–52.
Joseph-Auguste J, Lin L, Demar M, Duffas O, Molinie V, Sulpicy C, et al. Epidemiologic, clinical, ultrasonographic, and cytological features of thyroid nodules in predicting malignancy risk: a retrospective study of 442 French Afro-Caribbean patients. International journal of endocrinology. 2020;2020:4039290.
Bhuiyan MM, Machowski A. Nodular thyroid disease and thyroid malignancy: Experience at Polokwane Mankweng Hospital Complex, Limpopo Province, South Africa. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2015;105(7):570–2.
Melak T, Mathewos B, Enawgaw B, Damtie D. Prevalence and types of thyroid malignancies among thyroid enlarged patients in Gondar, Northwest Ethiopia: a three years institution based retrospective study. BMC Cancer. 2014;14:899.
Nassanga R, Kisembo H, Othieno E, Bugeza S, Fualal J. Sonographic correlation of thyroid nodules with ultrasound aided fine needle non aspiration cytology. East African Med J. 2015; 92(6):270
Tessler FN, Middleton WD, Grant EG. Thyroid imaging reporting and data system (TI-RADS): a user’s guide. Radiology. 2018;287(1):29–36.
Kwak JY, Han KH, Yoon JH, Moon HJ, Son EJ, Park SH, et al. Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology. 2011;260(3):892–9.
Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS committee. J Am Coll Radiol. 2017;14(5):587–95.
Azab EA, Abdelrahman AS, Ibrahim MEA. A practical trial to use Thyroid Imaging Reporting and Data System (TI-RADS) in differentiation between benign and malignant thyroid nodules. Egyptian J Radiol Nuclear Med. 2019;50(1):17.
Modi L, Sun W, Shafizadeh N, Negron R, Yee-Chang M, Zhou F, et al. Does a higher American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) score forecast an increased risk of malignancy? A correlation study of ACR TI-RADS with FNA cytology in the evaluation of thyroid nodules. Cancer Cytopathol. 2020;128(7):470–81.
Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology. Thyroid : official journal of the American Thyroid Association. 2009;19(11):1159–65.
Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ, et al. Managing incidental thyroid nodules detected on imaging: white paper of the ACR incidental thyroid findings committee. J Am Coll Radiol. 2015;12(2):143–50.
Akushevich I, Kravchenko J, Ukraintseva S, Arbeev K, Kulminski A, Yashin AI. Morbidity risks among older adults with pre-existing age-related diseases. Exp Gerontol. 2013;48(12):1395–401.
Luo J, McManus C, Chen H, Sippel RS. Are there predictors of malignancy in patients with multinodular goiter? J Surg Res. 2012;174(2):207–10.
Periakaruppan G, Seshadri KG, Vignesh Krishna GM, Mandava R, Sai VPM, Rajendiran S. Correlation between Ultrasound-based TIRADS and Bethesda system for reporting thyroid-cytopathology: 2-year experience at a tertiary care center in India. Indian J Endocrinol Metabol. 2018;22(5):651–5.
Kung AW, Chau MT, Lao TT, Tam SC, Low LC. The effect of pregnancy on thyroid nodule formation. J Clin Endocrinol Metab. 2002;87(3):1010–4.
Knudsen N, Laurberg P, Perrild H, Bülow I, Ovesen L, Jørgensen T. Risk factors for goiter and thyroid nodules. Thyroid. 2002;12(10):879–88.
Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013;2013: 965212.
Kelly FC, Snedden WW. Prevalence and geographical distribution of endemic goitre. Bull World Health Organ. 1958;18(1–2):5–173.
Grant EG, Tessler FN, Hoang JK, Langer JE, Beland MD, Berland LL, et al. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. JACR. 2015;12(12 Pt A):1272–9.
Biswas A, Basu K, De S, Karmakar S, De D, Sengupta M, et al. Correlation between thyroid imaging reporting and data system and Bethesda system of reporting of thyroid cytopathology of thyroid nodule: a single center experience. J Cytology. 2020;37(4):193–9.
Al-Ghanimi IA, Al-Sharydah AM, Al-Mulhim S, Faisal S, Al-Abdulwahab A, Al-Aftan M, et al. Diagnostic accuracy of ultrasonography in classifying thyroid nodules compared with fine-needle aspiration. Saudi J Med Med Sci. 2020;8(1):25–31.
Thattarakkal VR, Ahmed TSF, Saravanam PK, Murali S. Evaluation of thyroid nodule: Thyroid Imaging Reporting and Data System (TIRADS) and clinicopathological correlation. Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 3):5850–5.
Patil YP, Sekhon RK, Kuber RS, Patel CR. Correlation of ACR-TIRADS(thyroid imaging, reporting and data system)-2017 and cytological/ Histopathological (HPE) findings in evaluation of thyroid nodules. Int J Health Clin Res. 2020;3(11):6–19.
Dy JG, Kasala R, Yao C, Ongoco R, Mojica DJ. Thyroid Imaging Reporting and Data System (TIRADS) in stratifying risk of thyroid malignancy at the medical city. J ASEAN Fed Endocrine Soc. 2017;32(2):108–16.
Moifo B, Takoeta EO, Tambe J, Blanc Fo, Fotsin JG. Reliability of Thyroid Imaging Reporting and Data System (TIRADS) classification in differentiating Benign from malignant thyroid nodules. Open J Radiol. 2013;3(3):103.
Na DG, Baek JH, Sung JY, Kim JH, Kim JK, Choi YJ, et al. Thyroid imaging reporting and data system risk stratification of thyroid nodules: categorization based on solidity and echogenicity. Thyroid. 2016;26(4):562–72.
Wettasinghe MC, Rosairo S, Ratnatunga N, Wickramasinghe ND. Diagnostic accuracy of ultrasound characteristics in the identification of malignant thyroid nodules. BMC Res Notes. 2019;12(1):193.
Bhatnagar S, Mohi JK, Kaur N, Kaur A, Singh L. Correlation of tirads [thyroid imaging reporting and data system] and histopathological findings in evaluation of thyroid nodules. Int J Approximate Reasoning. 2017;5:1597–603.
Jabar ASS, Koteshwara P, Andrade J. Diagnostic reliability of the Thyroid Imaging Reporting and Data System (TI-RADS) in routine practice. Pol J Radiol [Internet]. 2019 2019; 84:[e274-e80 pp.].
Acknowledgements
We would like to acknowledge the endocrine surgery clinic staff for actively supporting the process of mobilization of study participants and data collection. We would also like to thank our statistician for his input from sample size estimation to data analysis. Special regards also to the study participants. We would like to commend the departments of radiology and pathology for collaborative work throughout the study period.
Funding
Self and partially funded by Islamic Development Bank.
Author information
Authors and Affiliations
Contributions
HMI, contributed conceptualization, investigation, writing-original draft, writing-review and draft. SGS, contributed conceptualization, investigation, writing-original draft. RL, contributed methodology, supervision, validation, visualization, writing –review and editing. RN, made substantial contributions to methodology, supervision, validation, visualization, writing-review and editing. FJO, made substantial contributions to Methodology, supervision, investigation, Validation, Visualization, Writing - review and editing. SB, made substantial contributions to methodology, supervision, investigation, validation, visualization, writing - review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all participants to participate in the study. Ethical approval was obtained from the Makerere University School of Medicine Research and Ethics committee (REC REF 2020–200), and administrative clearance was sought from Mulago National Referral Hospital. The study was also carried out following relevant guidlines and regulations according to the Helsinki declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Isse, H.M., Lukande, R., Sereke, S.G. et al. Correlation of the ultrasound thyroid imaging reporting and data system with cytology findings among patients in Uganda. Thyroid Res 16, 26 (2023). https://doi.org/10.1186/s13044-023-00169-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13044-023-00169-1