Abstract
Background
Tripartite Motif Containing 5 alpha (TRIM5α), a restriction factor produced ubiquitously in cells and tissues of the body plays an important role in the immune response against HIV. TRIM5α targets the HIV capsid for proteosomal destruction. Cyclophilin A, an intracellular protein has also been reported to influence HIV infectivity in a cell-specific manner. Accordingly, variations in TRIM5α and Cyclophilin A genes have been documented to influence HIV-1 disease progression. However, these variations have not been documented among Elite controllers in Uganda and whether they play a role in viral suppression remains largely undocumented. Our study focused on identifying the variations in TRIM5α and Cyclophilin A genes among HIV-1 Elite controllers and non-controllers in Uganda.
Results
From the sequence analysis, the rs10838525 G > A mutation in exon 2 of TRIM5α was only found among elite controllers (30%) while the rs3824949 in the 5′UTR was seen among 25% of the non-controllers. In the Cyclophilin A promoter, rs6850 was seen among 62.5% of the non-controllers and only among 10% elite controllers. Furthermore, rs17860048 in the Cyclophillin A promoter was predominantly seen among elite controllers (30%) and 12.5% non-controllers. From gene expression analysis, we noted that the respective genes were generally elevated among elite controllers, however, this difference was not statistically significant (TRIM5α p = 0.6095; Cyclophilin A p = 0.6389).
Conclusion
Variations in TRIM5α and Cyclophillin A promoter may influence HIV viral suppression. The rs10838525 SNP in TRIM5α may contribute to viral suppression among HIV-1 elite controllers. The rs6850 in the cyclophillin A gene may be responsible for HIV-1 rapid progression among HIV-1 non-controllers. These SNPs should be investigated mechanistically to determine their precise role in HIV-1 viral suppression.
Similar content being viewed by others
Background
Currently, 36.7 million people are living with HIV of which 70% are from the WHO African region [1]. To date, there is no documented cure, rather, HIV infected individuals are enrolled in lifelong Anti-retroviral Treatment (ART). Whereas ART enables them to live long healthy lives [1], there are concerns such as; viral latency, drug side effects and, resistance associated with long-term ART [2]. This creates a need to study host immune factors, restriction factors that enable host cells to resist HIV replication.
Restriction factors, dominantly acting proteins that function in a cell-autonomous manner to suppress HIV viral replication at distinct stages have been reported to influence HIV susceptibility and disease progression [3]. These include; Tripartite Motif-containing 5α (TRIM5α), Apolipoprotein B messenger RNA editing enzyme catalytic polypeptide-like 3 (APOBEC3), Tetherin/bone marrow stromal cell antigen (BST2) [3], Myxovirus resistance protein 2 (MxB), and Sterile α motif domain-HD domain-containing protein 1(SAMDH1) [11] of the 1300,000 adults living with HIV in Uganda [12]. Exploring variations in TRIM5α and CypA genes among HIV-1 elite controllers is therefore essential to identify protective mutations that can be used as target molecular markers for host-directed therapy and screening tools for targeted anti-HIV-1 therapy. In this study, we report on the variations in TRIM5α and CypA genes as well as their expression patterns among HIV-1 elite and non-controllers in Uganda.
Results
Participant characteristics
This was a cross-sectional study conducted among 18 HIV-1 chronically infected individuals. These included 10 elite controllers [HIV plasma viral load < 50 viral RNA (vRNA) copies ml−1] and 8 non-controllers (ART controlled) whose demographic characteristics are summarised in Table 1.
TRIM5α and Cyclophilin A gene variations
Considerable evidence suggests that variations in genes of intrinsic cellular defense against HIV influence HIV-1 disease progression [13, 14]. TRIM5α, one of the genes of intrinsic defense against HIV-1 and particularly it’s exon 2 that encodes for the ring domain that has E3 ubiquitin ligase activity and is important for the flexibility of TRIM proteins [15]. We sequenced the gene from the 5′UTR through exon 2 to intron 2. Previously stored PBMCs were thawed and then DNA extracted using Qiagen Blood Genomic DNA Kit (QIAamp DNA kit; Qiagen, Inc., Valencia, California, USA). The DNA was PCR amplified and then sequenced. Results indicate that rs10838525 single nucleotide polymorphisms (SNPs) were predominant among elite controllers (30%) while rs3824949 was more among non-controllers (25%) (Table 2; Fig. 1). Because SNPs in a coding region can affect protein function, we used the gomNAD browser to determine the effect of these mutations on protein function. The rs10838525 SNP in exon 2 was noted to cause R136Q amino acid change that is synonymous (Table 2; Fig. 1)
Additionally, the promoter region for Peptidyl Prolyl Isomerase A (PPIA) gene which encodes for Cyclophilin A protein was also sequenced and SNPs characterized. We found that elite controllers had more rs17860048 SNP (30%) while rs6850 SNP dominated among non-controllers (62.5%) (Table 3; Fig. 2).
TRIM5α and Cyclophilin A gene expression
To determine the effect of these mutations on gene expression, CD4+T cells were isolated using human CD4+ T cell enrichment magnetic kit following the manufacturer’s instructions (StemCell Technologies, Vancouver, Canada). The CD4+T cells were assessed for purity by flow cytometry using the BD FACS CANTO II (BD Bioscience, Franklin Lakes, New Jersey, USA), and then stimulated with plate coated Anti-CD3 and soluble Anti-CD28 monoclonal antibodies for 48 h. The cells were confirmed for activation by flow cytometry prior to gene expression studies (Fig. 3).
Total RNA was extracted using the Quick-RNA™ Whole Blood kit (Zymo Research, California, U.S.A) and mRNA levels of TRIM5α and Cyclophilin A was measured by RT qPCR. The respective genes were more expressed among HIV-1 elite controllers, however, the difference was not statistically significant (Fig. 4).
Graph A shows the difference in expression for TRIM5a gene is not statistically significant between elite controllers (EC) and non-controllers (NC) (p = 0.6095). Similarly, Graph B shows Cyclophillin A gene expression is more among elite controllers, but the difference is not statistically significant (p = 0.6369)
Discussion
Our findings suggest that variations in TRIM5α and the regulatory region of Cyclophilin A genes influence HIV-1 viremic control and consequently HIV disease progression. We have identified rs10838525 SNP in exon 2 of TRIM5α which is predominated among HIV-1 elite controllers (30%) while rs3824949 in the 5′UTR of TRIM5α is concentrated among non-controllers (25%). The rs10838525 SNP in exon 2 results in the amino acid change from Arginine to Glutamine at codon 136 (R136Q). This has been reported to confer protection against HIV for high-risk individuals and slow progress of HIV disease for those infected [7, 13]. In the present study, we report a high frequency of rs10838525 among elite controllers (30%). These findings are comparable to the 32% documented among HIV negative healthy controls in a previous study conducted to identify the distribution of TRIM5α mutations among Brazilian HIV positive individuals and HIV negative healthy controls [16]. Taken together, these findings imply that the rs1083852 confers protection against HIV disease progression. In the present study, the rs3824949 in the 5′UTR of TRIM5α was seen more among HIV-1 non-controllers (25%). The 5′UTR region is known for anchoring binding sites for proteins that regulate translation in response to molecular signals [17], therefore a mutation in this region could affect TRIM5a gene expression, eventually influencing HIV disease progression. Sun et al. in their study among acutely and chronically HIV-infected patients showed that rs3824949GG genotype was associated with rapid disease progression while those with the CC genotype had reduced risk for rapid disease progression [18]. The CG genotype, however, had no significant association with rapid disease progression [18]. Similar findings were reported among HIV-1 positive Caucasian homosexual men enrolled in the Amsterdam cohort Studies (ACS) [14]. The role of rs3824949 genotype has also been observed in other diseases, with the GG genotype being associated with rapid antiretroviral treatment response compared to the CG and CC genotypes among Hepatitis C infected individuals [19, 20]. Since the CG genotype was seen among non-controllers in our study, it may not be of any significance in HIV disease progression.
In the current study, we found rs6850 SNP in the regulatory region of Peptidyl Prolyl Isomerase A (PPIA) gene that encodes for Cyclophilin A protein, to be more concentrated among HIV-1 non-controllers (62.5%). The presence of rs6850 SNP possibly increases Cyclophillin A expression which in turn increases HIV infectivity. Previous studies show that rs6850 is significantly associated with high HIV viral loads and lower CD4+T cell counts [21,22,23]. Moreover, the minor allele rs6850G found among 62.5% of the non-controllers has been previously reported to increase Cyclophillin A mRNA levels [21], thus implying that rs6850 SNP could increase HIV infectivity and disease progression by altering Cyclophillin A plasma levels. This is supported by a study among diabetes patients that demonstrated that rs6850 was associated with increased plasma levels of Cyclophillin A, and an increased likelihood of cardiovascular diseases among patients with or without diabetes [24]. Additionally, Rath et al. also reported that rs6850 was associated with recurrent myocardial infarction among patients with symptomatic coronary artery disease [25]. Taken together, these findings could imply that rs6850 increases Cyclophillin A protein expression that affects signaling and protein folding thus promoting susceptibility to various disease pathologies including HIV infectivity and disease progression among non-controllers. Another SNP, rs17860048 was found to be more prevalent among elite controllers; however, its role in HIV disease progression has not been reported.
Furthermore, we wanted to understand whether the expression of the respective genes varied between HIV-1 elite controllers and non-controllers. Our study findings show that TRIM5α and Cyclophilin A are highly expressed among elite controllers compared to the non-controllers. However, this difference was not statistically significant (TRIM5α p = 0.6095 and CypA p = 0.6389). These findings agree with those from previous studies (40). Vigneault et al. (2011) in their transcriptional profiling study of CD4+ T Cells among HIV-1 patients noted that gene transcripts known to be involved in intrinsic cellular defense against retroviruses, such as the TRIM, tetherin/BST2, cyclophilin A, and other genes were not differentially expressed among elite controllers compared to ART controlled HIV positive individuals [26]. Nonetheless, other studies have found a correlation between elevated expression of Cyp A and HIV disease progression [27]. These findings could mean that the viral suppression effect exhibited by elite controllers could be due to other mechanisms, not necessarily increased expression of the respective genes. However the small sample size in our study may have limited us in producing statistically significant results. Another limitation of this study was the gender imbalance, we cannot rule out the possible effect of gender on these findings. Future studies should consider a more gender balanced approach in investigating the role of variations in TRIM5a and Cylophillin A genes among HIV-1 elite controllers.
Conclusion
In summary, our work reveals key SNPs within genes of intrinsic cellular defense against HIV that potentially play a role in HIV-1 viral suppression. Within the exon 2 of the TRIM5α gene, rs10838525 was only seen among elite controllers while rs6850 within the regulatory region of Cyclophillin A gene was seen predominantly among non–controllers (62.5%). These findings imply that variations in TRIM5α and cyclophilin A genes influence HIV-1 viral suppression. Furthermore, there was slightly higher TRIM5α and cyclophilin A gene expression among elite controllers as opposed to non-controllers although this difference was not statistically significant. This could imply that the elevated levels of genes involved in cellular intrinsic protective mechanisms against HIV may play a role in viral suppression exhibited by elite controllers and this effect needs to be investigated further with a large cohort of participants.
Methods
The aim, research design, and setting of the study
The study aimed at characterizing the variations in TRIM5α and CypA genes among Ugandan HIV-1 elite controllers and non-controllers.
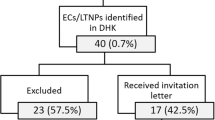
A laboratory-based crossectional study was conducted utilizing PBMC samples from the Elite study cohort. The Elite study was conducted between 2016 and 2018 and its aim was to examine the role of host genes in T cell resistance to HIV among Elite and Viremic controllers in Uganda. The Elite study recruited participants from Makerere University Joint Aids Program (MJAP) ISS clinic.
The laboratory experiments were conducted at Makerere University College of Health Sciences, Molecular and Immunology Laboratories. Other assays were conducted at the Center For AIDS Research (CFAR) laboratory, Joint Clinical Research Center in Kampala, Uganda.
Participant characteristics
The study utilized PBMC samples from two [2] patient groups, namely; a) HIV-1 elite controllers (undetectable viral load with > 5 years in care without ART) and b) non-controllers (HIV infected individuals well controlled on ART).
Elite controllers were selected basing on the following criteria; HIV infected individuals > 18 years old, have been confirmed to be HIV infected by HIV RNA PCR using Abbort real-time HIV-1 Assay (Abbott Molecular, USA), ART naïve for ≥ 5 years with CD4+ T cell count of ≥ 500 cells/ml, have a viral load of < 50copies/ml, have a hemoglobin concentration > 10 g/dl and are able to give written informed consent. Non-controllers were defined as HIV-1 infected individuals who are well controlled on ART. Being well controlled on ART meant CD4+ T cell count of > 500 cells/ml and no opportunistic infections. All those with active opportunistic infections e.g. Pneumocystis jiroveci pneumonia (PJP), Tuberculosis (TB), platelets < 50 and Bleeding disorders were excluded from the study.
Laboratory methods
Treatment of PBMCs before storage
PBMCs isolated using Ficoll gradient centrifugation were washed with PBS and centrifuged at 1700 rpm for 5 min. The supernatant was discarded, and the pellet re-suspended in 40 ml PBS, and the wash step repeated twice. The cells were stained with trypan blue and counted using an automatic cell counter (Invitrogen, Carlsbad, California, USA). Those with viability ≥ 96% were prepared for storage. The cells were re-suspended in 1 ml of freeze media, then 0.5 ml of each sample aliquoted and stored in 2 cryovials. The cryovials were immediately placed in Mr. Frosty storage container (Thermo Fisher Scientific, Waltham, Massachusetts, USA), then stored overnight in a freezer at − 80 °C. The cryovials were transferred to liquid nitrogen for storage the following day until use.
Sample processing and thawing
PBMCs were retrieved from liquid nitrogen and immediately thawed in a water bath set at 37 °C. Thereafter, they were transferred into 10 ml of R-10 media and then centrifuged at 1500 rpm for 10 min. The supernatant was decanted, and the pellet resuspended in 5 ml R-10 media (10% FBS, 1% Pen-strep, 1% l-Glutamine, 1% Hepes Buffer, and RPMI) for counting. The cells were stained with trypan blue and counted using an automatic cell counter (Invitrogen, Carlsbad, California, USA). 1 ml of the sample was removed for DNA extraction.
CD4+T cell isolation
The thawed PBMCS were subjected to CD4+ T cell isolation using human CD4+ T cell enrichment magnetic kit following the manufacturer’s instructions (StemCell Technologies, Vancouver, Canada). The isolated CD4+ T cells were washed in 1 ml PBS, centrifuged at 1500 rpm for 10 min. These were resuspended in 2 ml R-10 media, stained for counting with trypan blue and then incubated at 37 °C on a 24 well plate for 2 h in a CO2 incubator. The cells were also stained for purity using anti-CD3, and anti-CD4 and ran on a BD FACS Canto II (BD Biosciences, Franklin Lakes, New Jersey, USA).
CD4+T cell Stimulation
A 96-well plate coated with 100 μl of 5 μg/ml of Anti-CD3 (eBioscience Clone CD28.2) was incubated at 37 °C for 2 h in a CO2 incubator. For negative control wells, 100 μl of PBS was added. After the 2 h incubation, the plate was bloated. In each well, 100,000 cells from the sample were added and topped up with R-10 media containing 5 μg/ml of anti-CD28 (eBioscience clone OKT3) to make 200 μl per well. For negative control wells, 110 μl of PBS was added. The plate was incubated at 37 °C for 48 h in a CO2 incubator.
RNA extraction
RNA was extracted using Quick-RNA™ Whole Blood kit (Zymo Research, California, U.S.A) following the manufacturer’s instructions. The CD4+ T cell samples previously suspended in RNAlater (Sigma-Aldrich, St. Louis, Missouri, US) were centrifuged at 10.000 g for 1 min and then decanted. The pellet was re-suspended in 300 μl of DNA/RNA Shield™ then 30 μl PK digestion buffer and 15 μl Proteinase K added to the sample and mixed well. The mixture was incubated at 55 °C for 30 min. After incubation, the sample was vortexed and then centrifuged at 16,000 g for 2 min. The supernatant was transferred into RNase-free eppendoff tubes. To the supernatant, 350 μl of RNA recovery buffer was added and mixed well, transferred into a Zymo-Spin™ IIICG Column in a Collection Tube and centrifuged at 16,000g for 30 s. To the filtrate, 700 μl of 100% ethanol was added and mixed well. The mixture was transferred into a Zymo-Spin™ IC Column in a Collection Tube, centrifuged at 16,000g for 30 s and then the filtrate discarded. This was followed by DNase treatment to remove extra traces of DNA in the column. To achieve this, the column was washed with 400 μl RNA wash buffer and centrifuged at 16,000g for 30 s and thereafter the filtrate discarded. A Mixture of 5 μl DNase and 35 μl DNA digestion buffer was made and added directly to the column matrix. The column was incubated at room temperature for 15 min. After DNase treatment, 400 μl RNA prep buffer was added to the column and centrifuged at 16,000g for 30 s. The filtrate was discarded, and 700 μl RNA wash buffer added to the column and centrifuged at 16,000g for 30 s. The filtrate was discarded, 400 μl RNA wash buffer added and then centrifuged for 2 min at 16,000g. The column was then transferred into an RNase free eppendorf tube, thereafter, 15 μl DNase/RNase-free water added directly onto the column matrix to elute RNA. The eluted RNA was quantified by Qubit 4 Fluorometer (Invitrogen, Carlsbad, CA, USA). The RNA was then immediately stored at − 80 °C prior to downstream processes.
cDNA synthesis and reverse transcription PCR
Extracted RNA was subjected to cDNA synthesis and real-time PCR using QuantiTect Probe RT-PCR Kit (Qiagen Inc., Valencia, CA, USA) as described in the manufacturer’s instructions. A 50 μl reaction volume was used for the PCR. Primers and probes used were obtained from a previous study [28] and are summarized in Table 4. For each gene to be measured, separate master mix containing; a) 25 μl 2 × QuantiTect Probe RT-PCR Master Mix (HotStarTaq® DNA Polymerase, QuantiTect Probe RT-PCR Buffer, dNTP mix, including dUTP, ROX™ passive reference dye, and MgCl2), b) 2 μl of each of the forward and reverse primers, c) 1 μl of the probe, d) 0.5 μl of the QuantiTect RT Mix, and e) 12 μl of the RNase free water. In every PCR tube, 42 μl of the master mix was added, and then 4 μl of RNA template added in 3 tubes containing master mix of the 3 respective genes namely; GAPDH (reference gene), Cyclophilin A (target gene), and TRIM5α (target gene). For each of the genes, a negative control was added in each of the experiments containing mastermix and PCR water but no RNA template added. The PCR tubes were loaded into the Rotor gene Q real-time PCR machine (Quiagen Inc, Valencia, California, USA) and PCR set using the following conditions; reverse transcription (cDNA synthesis) at 55 °C for 30 min, PCR initial activation at 95 °C for 15 min, followed by 45 cycles of denaturation at 94 °C for 15 s, and combined annealing and extension 60 °C for 60 s. Ct values for each gene were obtained and analyzed using the delta CT relative quantification method to determine the fold change in gene expression.
DNA extraction
DNA was extracted using the Qiagen Blood Genomic DNA Kit (QIAamp DNA kit; Qiagen, Inc., Valencia, California, USA) in accordance with the manufacturer’s instructions as used in the previous studies [29]. 20 μl of Qiagen Protease was pipetted into the bottom of a 1.5 ml microcentrifuge tube, then 200 μl sample added. 200 μl Buffer AL was then added to the sample and mixed by pulse-vortexing for 15 s. The mixture was incubated at 56 °C for 10 min and centrifuged to remove drops from the inside of the lid. 200 μl ethanol (96–100%) were added to the PBMCs and mixed again by pulse-vortexing for 15 s. After mixing, the tube was again centrifuged to remove drops from the inside of the lid. The reaction mixture was applied to the QIAamp Mini column, centrifuged for 6000g for 1 min and the filtrate discarded. The column was placed in a clean 2 ml collection tube. 500 μl of Buffer AW1 was then added to the QIAamp Mini column and centrifuged at 6000g for 1 min. The tube containing the filtrate was discarded and the column placed in a new clean collection tube. 500 μl Buffer AW2 was also added, centrifuged at 20,000g for 3 min and the tube containing filtrate discarded. The column was placed in a new collection tube, centrifuged at 20,000g for 1 min and the tube containing filtrate discarded. The QIAamp Mini column was then placed in a clean 1.5 ml microcentrifuge tube and 200 μl Buffer AE added. The mixture was incubated at room temperature for 1 min and then centrifuged at 6000g for 1 min to elute DNA. The extracted DNA was stored at − 80 °C prior to PCR amplification.
PCR amplification
Exon 2 of TRIM5α gene
PCR amplification of TRIM5α gene (5′UTR, exon 2 & intron 2) was carried out with 35 cycles of denaturation at 94 °C for 30 s, annealing at 58 °C for 30 s, and extension at 68 °C for 45 s using SuperScript III platinum Taq polymerase (Invitrogen, Carlsbad, California, USA) in the presence of 2× reaction buffer, 5 mM MgCl with primers summarized in Table 5 as described in a similar study [13].
Cyclophillin A gene promoter
PCR amplification of the Cyclophilin A gene was carried out with 40 cycles of denaturing at 95 °C for 30 s, annealing at 65 °C for 45 s, and extension at 68 °C for 45 s using SuperScript III platinum Taq polymerase (Invitrogen, Carlsbad, California, USA) in the presence of 2X reaction buffer, 5 mM MgCl with primers summarized in Table 6 as described in a similar study [30].
PCR Clean up
From all samples positive on gel electrophoresis that have a single band, 10 μl was aliquoted into a new PCR tube and 2 μl of ExosapIT reagent added. The tubes were then transferred into a thermocycler (Applied Biosystems, California, United States) and ran under the following conditions: 37 °C for 45 min, 80 °C for 45 min and held at 4 °C. Thereafter, PCR products were stored at − 20 °C prior to Sanger sequencing.
Sanger sequencing
Cycle sequencing
Sequencing mastermix was prepared including 0.5 μl of big dye terminator, 1.75 μl of 5X sequencing buffer, 2.5 μl of primer, and 4.25 μl of water for the 10 μl reaction. 9 μl of the master mix was added into each plate well and 1 μl of the sample was then added. The plate was loaded in a SimpliAmp thermocycler (Applied Biosystems, California, United States), and ran under the following conditions; 96 °C for 1 min, then 30 cycles of 96 °C for 20 s, 50 °C for 20 s, and 60 °C for 4 min. Thereafter, the plate was held at 4 °C awaiting cleaning.
Clean up
Ethanol precipitation was done as follows. The 96-well sequencing reaction plate was removed from the SimpliAmp thermocycler and the plate centrifuged at 1000 rpm for one minute without cooling. To each well, 2.5 μl of 125 mM EDTA was added, followed by 1.0 μl 3 M Sodium Acetate pH 5.2 and then 30 μl of Absolute Ethanol to each well. The plate was sealed and vortexed briefly for 5 s, then incubated at room temperature for 30 min to precipitate the extension products. The plate was centrifuged at 3000 rpm for 60 min, at 4 °C. The plate cover was then removed, and the plate inverted on a paper towel placed in the microplate carrier assembly in the plate centrifuge. The plate was centrifuge at 500 rpm for one minute. 100 μl of 70% absolute Ethanol were added to each plate well and the plate heated at 90 °C for 1 min in a SimpliAmp thermocycler (Applied Biosystems, California, United States).
Electrophoresis
10 µl of 0.1 mM EDTA was added to each sample well and the plate sealed. The plate was vortexed for 5 s and then centrifuged at 1000 rpm for one minute without cooling to bring down the contents of the wells. The samples were then ready to run in the 3730xl DNA analyzer (Applied Biosystems, California, United States).
Data analysis
Data was entered in excel and exported to GraphPad prism 8 for analysis. CD4+ T cells were analyzed on an 8-laser FACS Canto II (BD Bioscience, Franklin Lakes, New Jersey, USA). Approximately 50,000 events were recorded per sample. In addition, antibody capture beads (BD Bioscience, Franklin Lakes, New Jersey, USA) were used for compensation and prepared individually by separate staining of all the antibodies used in the experiment. FlowJo X 10.6 (Treestar, Oregon, USA) was used for gating analysis. For mRNA quantification, relative quantification using the obtained CT value was done using the delta CT method. Statistical differences between the different groups were determined using the unpaired t test in Graph pad prism v8. Sequence analysis was done using Mutation Surveyor software to identify SNPs in the respective genes. Frequencies and percentages of the SNPs were determined. SNPs in the coding region were analysed using the gnomAD to determine the amino-acid change.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- Cyclophilin A:
-
CypA
- DNA:
-
Deoxyribonucleic acid
- HIV:
-
Human immunodeficiency virus
- MJAP:
-
Makerere University Joint Aids Program
- PBMC:
-
Peripheral blood mononuclear cells
- PCR:
-
Polymerase chain reaction
- RNA:
-
Ribonucleic acid
- SNP:
-
Single nucleotide polymorphism
- TRIM5α:
-
Tripartite Motif containing 5 alpha
- WHO:
-
World Health Organization
References
WHO. HIV/AIDS: World Health Organization; 2017 http://www.who.int/mediacentre/factsheets/fs360/en/.
Pham HT, Mesplede T. The latest evidence for possible HIV-1 curative strategies. Drugs in context. 2018;7:212522.
Malim MH, Bieniasz PD. HIV restriction factors and mechanisms of evasion. Cold Spring Harbor Perspect Med. 2012;2(5):a006940.
Jia X, Zhao Q, **ong Y. HIV suppression by host restriction factors and viral immune evasion. Curr Opin Struct Biol. 2015;31:106–14.
Lukic Z, Hausmann S, Sebastian S, Rucci J, Sastri J, Robia SL, et al. TRIM5α associates with proteasomal subunits in cells while in complex with HIV-1 virions. Retrovirology. 2011;8(1):93.
Kawai T, Akira S. Regulation of innate immune signalling pathways by the tripartite motif (TRIM) family proteins. EMBO Mol Med. 2011;3(9):513–27.
Price H, Lacap P, Tuff J, Wachihi C, Kimani J, Ball TB, et al. A Trim5alpha exon 2 polymorphism is associated with protection from HIV-1 infection in Pumwani sexworker cohort. AIDS (London, England). 2010;24(12):1813.
Sawyer SL, Wu LI, Akey JM, Emerman M, Malik HS. High-frequency persistence of an impaired allele of the retroviral defense gene TRIM5α in humans. Curr Biol. 2006;16(1):95–100.
Burse M, Shi J, Aiken C. Cyclophilin A potentiates TRIM5α inhibition of HIV-1 nuclear import without promoting TRIM5α binding to the viral capsid. PLoS ONE. 2017;12(8):e0182298.
Rits MA, Van Dort KA, Kootstra NA. Polymorphisms in the regulatory region of the Cyclophilin A gene influence the susceptibility for HIV-1 infection. PLoS ONE. 2008;3(12):e3975.
Kayongo A, Gonzalo-Gil E, Gümüşgöz E, Niwaha AJ, Semitala F, Kalyesubula R, et al. Identification of Elite and Viremic Controllers from a Large Urban HIV Ambulatory Center in Kampala, Uganda. J Acquir Immune Defic Syndr. 2018;79(3):394.
UNAIDS. HIV and AIDS estimates: UNAIDS Uganda Country Office; 2020. https://www.unaids.org/en/regionscountries/countries/uganda. Accessed 8 June 2020.
Javanbakht H, An P, Gold B, Petersen DC, O’Huigin C, Nelson GW, et al. Effects of human TRIM5α polymorphisms on antiretroviral function and susceptibility to human immunodeficiency virus infection. Virology. 2006;354(1):15–27.
Van Manen D, Rits MA, Beugeling C, Van Dort K, Schuitemaker H, Kootstra NA. The effect of Trim5 polymorphisms on the clinical course of HIV-1 infection. PLoS Pathog. 2008;4(2):e18.
Grütter MG, Luban J. TRIM5 structure, HIV-1 capsid recognition, and innate immune signaling. Current opinion in virology. 2012;2(2):142–50.
Da Silva RC, Coelho AVC, Arraes LC, Brandão LAC, Crovella S, Guimarães RL. TRIM5 gene polymorphisms in HIV-1-infected patients and healthy controls from Northeastern Brazil. Immunol Res. 2016;64(5–6):1237–42.
Chatterjee S, Pal JK. Role of 5′-and 3′-untranslated regions of mRNAs in human diseases. Biol Cell. 2009;101(5):251–62.
Sun X, Li W, Liu W, Wang R, Li Q, Wu H. Genetic polymorphisms of Trim5a are associated with disease progression in acutely and chronically HIV-infected patients. Int J Clin Exp Med. 2015;8(9):16199.
Mobasheri S, Irani N, Sepahi AA, Sakhaee F, Jamnani FR, Vaziri F, et al. Evaluation of TRIM5 and TRIM22 polymorphisms on treatment responses in Iranian patients with chronic hepatitis C virus infection. Gene. 2018;676:95–100.
Medrano LM, Rallón N, Berenguer J, Jiménez-Sousa MA, Soriano V, Aldámiz-Echevarria T, et al. Relationship of TRIM5 and TRIM22 polymorphisms with liver disease and HCV clearance after antiviral therapy in HIV/HCV coinfected patients. J Transl Med. 2016;14(1):257.
Madlala P, Singh R, An P, Werner L, Mlisana K, Karim SSA, et al. Association of polymorphisms in the regulatory region of the cyclophilin A gene (PPIA) with gene expression and HIV/AIDS disease progression. J Acquir Immune Defic Syndr. 2016;72(5):465.
Bleiber G, May M, Martinez R, Meylan P, Ott J, Beckmann JS, et al. Use of a combined ex vivo/in vivo population approach for screening of human genes involved in the human immunodeficiency virus type 1 life cycle for variants influencing disease progression. J Virol. 2005;79(20):12674–80.
von Hahn T, Ciesek S. Cyclophilin polymorphism and virus infection. Curr Opin Virol. 2015;14:47–9.
Vinitha A, Kutty VR, Vivekanand A, Reshmi G, Divya G, Sumi S, et al. PPIA rs6850: a > G single-nucleotide polymorphism is associated with raised plasma cyclophilin A levels in patients with coronary artery disease. Mol Cell Biochem. 2016;412(1–2):259–68.
Rath D, von Ungern-Sternberg S, Heinzmann D, Sigle M, Monzien M, Horstmann K, et al. Platelet surface expression of cyclophilin A is associated with increased mortality in patients with symptomatic coronary artery disease. J Thromb Haemost. 2020;18(1):234–42.
Vigneault F, Woods M, Buzon MJ, Li C, Pereyra F, Crosby SD, et al. Transcriptional profiling of CD4 T cells identifies distinct subgroups of HIV-1 elite controllers. J Virol. 2011;85(6):3015–9.
Braaten D, Luban J. Cyclophilin A regulates HIV-1 infectivity, as demonstrated by gene targeting in human T cells. EMBO J. 2001;20(6):1300–9.
Matsuoka S, Dam E, Lecossier D, Clavel F, Hance AJ. Modulation of HIV-1 infectivity and cyclophilin A-dependence by Gag sequence and target cell type. Retrovirology. 2009;6(1):21.
Singh H, Samani D, Ghate MV, Gangakhedkar RR. Impact of cellular restriction gene (TRIM5α, BST-2) polymorphisms on the acquisition of HIV-1 and disease progression. J Gene Med. 2018;20(2–3):e3004.
An P, Wang LH, Hutcheson-Dilks H, Nelson G, Donfield S, Goedert JJ, et al. Regulatory polymorphisms in the cyclophilin A gene, PPIA, accelerate progression to AIDS. PLoS Pathog. 2007;3(6):e88.
Acknowledgements
We would like to extend our sincere gratitude to Dr. David Patrick Ketete, Head of Department Immunology and Molecular Biology for his technical guidance during the research as well as Ms. Geraldine Nalwadda, Department of Immunology and Molecular Biology for her administrative support. We thank the staff of Immunology and molecular laboratories at Makerere University as well as the Center for AIDS Research laboratories at the Joint Clinical Research Center, Kampala Uganda for their technical input during the research.
Funding
This work was done as partial fulfillment for the award of a degree of Master of Science in Immunology and Clinical Microbiology to SBA. SBA is a MITHU fellow and the research was funded by NIH Fogarty, Grant No. D43TW010319 (MITHU PI: Henry Boom). Part of the work was funded by the African Centre of Cxcellence in Materials, Product development, and Nanotechnology (ACE_MAPRONANO) Project ID: P151847/IDA 5797-UG. OJS is a NURTURE fellow under NIH grant D43TW010132 (PI: Nelson Sewankambo).
Author information
Authors and Affiliations
Contributions
There are 13 authors in this manuscript namely; SBA, BN, FW, BO, RN, EN, AFK, RN, AB,AK, GM, MW, and OJS. SBA conceived the concept and developed it under the supervision of MW and OJS. SBA, BN,FW, AK, BO,RN, AB, RN and OJS conducted the cell isolation, culture and flow cytometry experiments of the study. SBA, BN, EN, AFK, GM, and MW conducted the DNA sequencing and RNA expression experiments and contributed to bioinformatics analysis. SBA made the final draft of the manuscript and all authors proofread and approved for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Makerere University School of Biomedical Sciences Research and Ethics Committee. A waiver of consent was obtained before samples were used.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amanya, S.B., Nyiro, B., Waswa, F. et al. Variations in Trim5α and Cyclophilin A genes among HIV-1 elite controllers and non controllers in Uganda: a laboratory-based cross-sectional study. Retrovirology 17, 19 (2020). https://doi.org/10.1186/s12977-020-00527-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12977-020-00527-z