Abstract
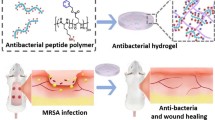
The advancement of biomaterials with antimicrobial and wound healing properties continues to present challenges. Macrophages are recognized for their significant role in the repair of infection-related wounds. However, the interaction between biomaterials and macrophages remains complex and requires further investigation. In this research, we propose a new sequential immunomodulation method to enhance and expedite wound healing by leveraging the immune properties of bacteria-related wounds, utilizing a novel mixed hydrogel dressing. The hydrogel matrix is derived from porcine acellular dermal matrix (PADM) and is loaded with a new type of bioactive glass nanoparticles (MBG) doped with magnesium (Mg-MBG) and loaded with Curcumin (Cur). This hybrid hydrogel demonstrates controlled release of Cur, effectively eradicating bacterial infection in the early stage of wound infection, and the subsequent release of Mg ions (Mg2+) synergistically inhibits the activation of inflammation-related pathways (such as MAPK pathway, NF-κB pathway, TNF-α pathway, etc.), suppressing the inflammatory response caused by infection. Therefore, this innovative hydrogel can safely and effectively expedite wound healing during infection. Our design strategy explores novel immunomodulatory biomaterials, offering a fresh approach to tackle current clinical challenges associated with wound infection treatment.
Similar content being viewed by others
Introduction
The largest organ of the human body, the skin, plays a primary defensive role against external environmental threats [1]. Infections that permeate this barrier through wounds may cause severe inflammation, adversely affecting healing and potentially leading to life-threatening conditions [2]. Thus, it is crucial to develop innovative, multifunctional bioactive materials that can eradicate infections and enhance wound healing and tissue regeneration. Various types of dressing materials, such as nanofiber films and hydrogels, have been designed for this purpose [3, 4]. Hydrogels are known for their high permeability, biocompatibility and moisturizing qualities, positioning them as promising materials for treating infectious wounds [5, 6]. However, traditional hydrogel dressings often lack inherent antibacterial properties, limiting their use to conjunction with antibiotics [7, 8]. Regrettably, long-term use of antibiotics may yield bacterial resistance and provoke adverse hepatic or renal side effects, impeding the wound healing process [9, 10]. Therefore, there is an urgent need to develop new types of hydrogel dressings capable of taking effect without relying on antibiotics.
Infectious wounds render a host of complications owed to particular inflammatory conditions which obstruct the physiological sequence of wound healing and considerably challenge macrophages’ polarization from pro-inflammatory (M1) to anti-inflammatory (M2) phenotypes [11]. A surfeit of M1 macrophages accumulates within the wound, excreting pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and producing reactive oxygen species [12]. This action consecutively induces oxidative stress and a cellular damage microenvironment within the wound, resulting persistent inflammation and vascular alterations. This sequence culminates in impeded wound healing, amplified inflammatory mediators and a perpetuated detrimental cycle [13,14,15]. Consequently, manipulating the immune microenvironment and fostering angiogenesis are crucial for healing infectious wounds. Immune modulation triggers the expression of transforming and proliferative cytokines, renowned for their angiogenesis promoting attributes [6d). In a similar vein, the mean nodule formation experienced a surge of 7.72, 7.46, and 7.28 times relative to the control, PADM, and PADM@Mg aggregates, accordingly (Fig. 6d).
Studies have indicated that administering curcumin by gavage can enhance neovascularization and wound healing in mice with diabetic foot ulcers. Additionally, the local application of 1% turmeric extract gel has been found to have a beneficial impact on angiogenesis [48]. Furthermore, there is no substantial variance in the effects of various administration routes of curcumin on wound healing. The results of this investigation indicated that the rates of cell migration and angiogenesis were significantly enhanced in cells treated with PADM@MgC, which is advantageous for the healing of wounds, although the exact mechanism requires further exploration.
In vitro cell migration and angiogenesis behavior of various PADM-based hydrogels. (a) Different migration abilities of HUVECs after coculturing with the extract of various PADM-based hydrogels. Scale bar: 100 μm. (b) Quantification of gap closure ratio of different groups. Scale bar: 100 μm. (c) Fluorescence images of tube formation experiment via coculturing HUVECs with the extract of various PADM-based hydrogels. (d) Quantifications of junctions and tube length in each group. Results are presented as mean ± SD (N = 3). ****P < 0.0001
In vitro biocompatibility
The biocompatibility of hydrogels is a vital parameter for their adoption in clinical settings as wound dressings. To this end, cell viability assays were conducted after culturing cells on various hydrogel compositions for a 24-hour period followed by live/dead staining procedures. Live cells exhibited green fluorescence, while the nuclei of nonviable cells emitted red fluorescence. Observations indicated a predominance of viable cells post-incubation on hydrogels-control, PADM, PADM@Mg, and PADM@MgC (Fig. 7a-b). Subsequent quantification via the CCK-8 assay reaffirmed the absence of significant cytotoxicity attributed to the hydrogels (Fig. 7c). SEM imaging further corroborated these findings by displaying cells in a state of healthy morphology upon hydrogel substrates (Fig. 7d).
The cytocompatibility of different PADM-based hydrogels in vitro. (a) Confocal microscopy images of a live/dead assay of cells co-cultured with several PADM-based hydrogels for 24 h. Scale bar: 200 μm. (b) Quantitative analysis of rusults from (a). (c) Cell proliferation of PADM-based hydrogels. (d) SEM results of RAW 264.7 co-cultured with PADM-based hydrogels for 24 h
In vivo investigation on PADM@MgC for Infected Wound Healing
Prolonged non-healing of wounds may increase the risk of bacterial infection. Furthermore, this type of infection may compromise the immune function, thereby adversely affecting wound healing and ultimately leading to systemic infection. Therefore, expediting wound healing is imperative for preventing and treating infections. Next, we will utilize a murine excisional skin infection model to determine the impact of PADM@MgC hydrogel on wound healing (Fig. 8a).
With the progression of time, the infected wounds in each treatment group gradually underwent healing (Fig. 8b-c). However, significant variations were observed in the infection severity and rate of healing. Four days ago, the wounds of the control group, PADM group, and PADM@Mg group all exhibited evident infection, tissue necrosis, and discharge of pus. In contrast, the wounds of the PADM@MgC group remained consistently clean and dry throughout the entire observation period, showing no signs of obvious infection or suppuration. Furthermore, the mice in the PADM@MgC group demonstrated quicker wound healing (Fig. 8d), with only 17.1 ± 2.5% of the wounds remaining unhealed on the 10th day, followed by the PADM@Mg group (33.2% ± 1.6%), PADM group (42.5% ± 2.6%), and the control group (44.1% ± 2.1%). Additionally, on the 4th day, spreading plate method (SPM) was employed to evaluate the bacterial survival rate on the wounds after different treatments, showing a significant decrease in the bacterial survival rate following treatment with PADM@MgC hydrogel (Fig. 8e).
PADM@MgC demonstrates increased effectiveness in facilitating the healing of infected wounds in vivo. (a) Illustration of the model for mouse excisional wound infection and the experimental methods. (b) Representative photographic images of wounds in different groups after 0, 1, 4, 7, or 10 days of treatment. (c) Day 0 (blue), day 1 (orange), day 4 (purple), day 7 (yellow), and day 10 (green) explanatory photos of the wounds, as well as superimposed photos of treatment with various PADM-based hydrogels. (d) Area of unhealed wounds in each group at different time periods. (e) Bacterial counts in the wounds of the different treatment groups. Results are presented as mean ± SD (N = 3). **P < 0.01; ***P < 0.001; ****P < 0.0001
Histological evaluations were undertaken through HE staining (Fig. 9a), with findings aligning with the statistical patterns observed in wound surface diminution. Moreover, the extent of granulation tissue formation among the mouse cohorts was quantified (Fig. 9b). Notably, the PADM@MgC-treated group exhibited accelerated wound closure, a trend that was most evident during the initial healing phases. Quantitative assessment of the granulation tissue thickness indicated a superior contraction rate in the PADM@MgC group relative to its counterparts. Effective wound repair is contingent upon vascularization to supply essential nutrients and oxygen. Consequently, angiogenic sufficiency is a critical component of the healing process. To gauge angiogenic activity, we assessed the expression levels of endothelial cell marker, cell adhesion molecule 1 (CD31), within the wound beds (Fig. S2). Comparative analysis indicated a heightened presence of CD31 in the wound tissues treated with PADM@MgC hydrogel. Collectively, these data point towards the notable wound-healing capabilities of PADM@MgC hydrogel. Further immunofluorescence analysis revealed that the PADM@MgC group had the lowest proportion of M1 macrophages (iNOS) (Fig. 9d and e) and the highest proportion of M2 macrophages (CD206) (Fig. 9d and f), confirming the in vitro results. These findings suggest that PADM@MgC triggers macrophage polarization towards an M2 phenotype, inducing an anti-inflammatory microenvironment, thereby promoting wound healing.
PADM@MgC hydrogel-induced acceleration of the wound repair. (a) Images of HE and Masson’s trichromatic staining of the infectious wounds of different groups on day 10. (b) Corresponding quantitative analysis of the granulation tissue width on Day 10. (c) Images of Giemsa staining of the infectious wounds of different groups on day 10. (d) Immunofluorescence staining for iNOS (M1-labelled) and CD206 (M2-labelled) was performed on tissue sections at the wound site on days 4 post-infection e, (f) Statistical analyses regarding the proportion of (e) iNOS- and (f) CD206-positive macrophages. Results are presented as mean ± SD (N = 3). ****P < 0.0001
Conclusion
Here, we developed a PADM@MgC hydrogel to enhance post-infectious wound healing by sequentially releasing Cur and Mg2+. The therapeutic effectiveness of PADM@MgC was optimized through (i) improved stability and bioavailability of Cur; (ii) anti-inflammatory, antimicrobial, and cell proliferation-promoting effects of Cur; (iii) Mg2+ improving cell migration and angiogenesis; (iv) Mg2+ and curcumin synergistically promote repolarization of M2 macrophages; (v) the hybridized hydrogel forming a physical barrier to prevent secondary damage; and (vi) the hybridized hydrogel achieving exudate absorption and antimicrobial PADM@MgC. Various functions of PADM@MgC have been demonstrated in vivo and in vitro. However, our study did not comprehensively examine the mobilization and function of other immune cells (e.g. DC cells, T cells, NK cells, etc.) in addition to macrophages during the initial stages of infected wound healing. Additionally, the molecular mechanisms of these processes have not been explored. In the next phase of our research, we will focus on these aspects in order to better understand the factors that promote infected wound healing through the use of biomaterials. Nevertheless, this novel diachronic bidirectional immunomodulatory hydrogel has good antimicrobial and wound healing effects and can be used to design and synthesize biomaterials that modulate immune responses according to the immune profile of the target disease.
Materials and methods
Synthesis of PADM@MgC hydrogel
The preparation protocol for Mg-MBG and Mg-MBG@Cur is comprehensively outlined in the Supporting Information. The porcine skin tissue, after a 3-hour rinse in sterile water, underwent multiple freeze/thaw cycles using liquid nitrogen. This was followed by agitation at 120 rpm and 25 °C to facilitate the removal of subcutaneous layers. The tissue samples were then treated with 0.1% Triton X-100 for 12 h and subsequently with 0.1% sodium dodecyl sulfate for 6 h. The final steps involved lyophilization, grinding into a fine powder, and digestion with pepsin in an acidic milieu (pH 2–3) for 10 min. Mg@C nanoparticles were introduced and rapidly mixed into the solution. The resulting gel was refrigerated at 4 °C and enzymatically digested over a 2-hour period until it achieved a translucent, viscous consistency. Subsequent steps included the addition of PBS to regulate osmotic pressure, followed by pH normalization to 7–8 using chilled 10 M NaOH. PADM@MgC hydrogels were then synthesized by incubating these gels at 37 °C for 20 min, followed by freeze-drying and compression. The final PADM@MgC hydrogels, with concentrations of 1%, 5%, and 10%, were determined based on the mass differential between the added nanoparticles and the freeze-dried hydrogel powder. In parallel, PADM@Mg hydrogels were synthesized using an identical process, except Mg-MBG were used in place of Mg@C nanoparticles for PADM@Mg preparation.
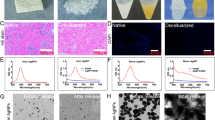
Characterization of PADM@MgC hydrogels
Initially, Hematoxylin and Eosin (HE) and DAPI staining were conducted to evaluate the removal of cellular and nuclear debris. The DNA content of each set of skin tissue samples was analyzed using a DNA extraction kit, following the instructions in the manual. The DNA content of each set was measured using a UV spectrophotometer. Following this, the samples underwent dehydration through a critical point drying process. The structural characteristics of the hydrogels were then examined via scanning electron microscopy. Subsequently, the chemical composition of these materials was investigated using X-ray Photoelectron Spectroscopy (XPS), X-ray Diffraction (XRD), and Fourier-Transform Infrared (FTIR) spectroscopy.
Water retention
The hydrogels PADM, PADM@Mg, and PADM@MgC were incubated at 37 °C, and their masses were periodically recorded until a stable mass was noted. The water retention capacity of these hydrogels was determined using the formula:
Here, W2 denotes the hydrogel’s weight at each measured time point, while W1 represents its initial weight.
Biodegradability
The biodegradability of PADM, PADM@Mg, and PADM@MgC hydrogels was determined under different conditions. The hydrogels were solidified in PBS and then incubated at 37 °C with or without trypsin. The solution was removed from the centrifuge tube, and the hydrogels were washed with PBS daily. Finally, the samples were dried and weighed.
Hygroscopic properties
To investigate the hygroscopic properties of the hydrogel, 1 mL of the synthesized hydrogel was divided into thirds and subjected to lyophilization to obtain the initial dry weight (W0). Subsequently, the hydrogel was immersed in a 10 mL PBS solution and incubated at 37 °C for different time intervals (10 min, 30 min, 30 min, 30 min, and 30 min). At each time point, the hydrogel was removed, and its weight (Wt) was measured. The swelling ratio was then calculated using the formula:
Ion release assessment
The investigation of ion release from PADM@MgC hydrogels involved placing an equal mass of hydrogel in 10 mL of simulated body fluid (SBF, PH1820, China). The medium was entirely replaced daily with fresh SBF to maintain consistent conditions. Copper and zinc ion concentrations were quantified using an inductively coupled plasma atomic emission spectrometer (X Series 2, Thermo Fisher Scientific, USA). For comparative analysis, control hydrogels PADM and PADM@Mg were subjected to identical testing procedures.
Cells and bacteria
This study utilized mouse-derived macrophages (RAW264.7) and human umbilical vein vascular endothelial cells (HUVEC), both acquired from the Shanghai Institute of Cell Biology. These cells were cultured in DMEM medium, enriched with 10% fetal bovine serum (FBS) and 1% penicillin/streptomycin. Additionally, Methicillin-resistant Staphylococcus aureus (MRSA, ATCC 43,300) was procured from the American Type Culture Collection and propagated in tryptic soy broth (TSB; Hopebio).
Preparation of sample extracts
The PADM, PADM@Mg, and PADM@MgC hydrogels were sectioned into 10 × 10 × 5 mm dimensions and submerged in DMEM supplemented with 10% FBS and 1% penicillin/streptomycin. The cultures were incubated at 37 °C for 24 h, after which the extracts were obtained and preserved at 4 °C for subsequent analysis.
In vitro antibacterial tests
Frozen MRSA cultures were revived and incubated overnight in TSB at 37 °C on a shaker. This was followed by a dilution step at a 1:10,000 ratio, leading to further incubation until the cultures reached the logarithmic growth phase. Subsequently, bacterial suspensions with a concentration of 1 × 106 CFU/mL, in a volume of 500 µL, were introduced to a variety of hydrogels for incubation. The influence of these hydrogels on bacterial growth was evaluated through growth curve assays. These experiments were conducted in triplicate and replicated thrice to ensure the robustness of the data. Following this, the bacteria were co-cultured with the different hydrogels for 24 h. Post-incubation, SPM and colony-forming unit (CFU) quantification were carried out on agar plates to further assess the interaction between the bacteria and the hydrogels. Additionally, we analyzed the antibacterial activity by live/dead staining. Briefly, we added 500 µL of combined dye (Syto9 and PI) in different samples and cultured them for 15 min. Bacteria were collected on glass slides and visualized under a fluorescence microscope.
Membrane damage and leakage assessment
To detect membrane damage and leakage, bacteria and hydrogels were co-cultured for 24 h. Post-co-culture, SEM was employed to examine the morphological characteristics of the bacteria. In addition, the samples were stained with Propidium Iodide (PI) at a concentration of 2.5 µg/mL for 30 min. The fluorescence intensity of these stained samples was then measured at an excitation/emission wavelength of 535 nm/615 nm using a microplate reader. Subsequently, cell content leakage under various treatment conditions was evaluated. This involved centrifuging the bacterial supernatant post-co-culture at 8000 × g for 10 min, followed by measuring the absorbance at 260 nm for nucleic acids (A260) and 280 nm for proteins (A280) using a spectrophotometer. All experiments were conducted in triplicate to ensure consistency and accuracy.
In vitro immunomodulatory evaluation
Immunofluorescence
Briefly, RAW264.7 cells were incubated with PADM, PADM@Mg, or PADM@MgC hydrogels for one day. Subsequently, the cells were collected, fixed, and blocked before staining with antibodies against iNOS (ab210823) and CD206 (ab64693). Next, cells were incubated with corresponding secondary antibodies and counterstained with DAPI for 1 h. The cells were observed and photographed using CLSM.
Flow cytometry assay
Flow cytometry, employing antibodies against CD86 and CD206, was utilized to assess the ratios of M1 and M2 macrophages. Macrophages were initially cultured with various hydrogels for a 24-hour period. This was followed by a 40-minute blocking phase and staining with allophycocyanin (APC)-conjugated CD206 and phycoerythrin (PE)/Cy7-conjugated CD86. The final steps involved washing the cells, resuspending them in 400 µL of PBS, and their subsequent evaluation using flow cytometry.
Gene expression
To investigate gene expression profiles in macrophages, we undertook transcriptome sequencing analyses. RAW 264.7 cells, initially inoculated at 5 × 105 cells per well, were subjected to a 24-hour incubation with diverse hydrogels in an LPS-enriched environment. Following this, total cellular RNA was meticulously extracted using TRIzol reagent, in strict accordance with the manufacturer’s instructions. The subsequent RNA-sequencing and bioinformatics analyses were proficiently conducted by Novel Biotech, Shanghai. This process facilitated the examination of differentially expressed genes (DEGs) for their involvement in KEGG pathways and gene ontology enrichment.
RT-PCR and ELISA
RAW 264.7 cells were cultivated following the above outlined method and harvested after a 24-hour period. Total RNA was then meticulously extracted utilizing TRIzol. For accuracy in gene expression analysis, normalization was conducted against the housekee** gene ACTB. Details of the primer sequences used are comprehensively listed in the Supplementary Information (Table S1). Furthermore, culture supernatants were harvested from macrophages post-incubation with various hydrogels. The concentrations of cytokines IL-1β, TNF-α, IL-6, and IL-10 in these supernatants were quantitatively assessed employing Enzyme-Linked Immunosorbent Assay (ELISA).
Cell viability analysis
Cellular cytotoxicity was evaluated using a live/dead staining kit, applied as per the manufacturer’s guidelines. Additionally, to ascertain the biocompatibility of the hydrogels, a Cell Counting Kit-8 (CCK-8) assay was conducted. In this process, cells were co-cultured with different hydrogels at a density of 2 × 104 cells per well. After 24 h, for live cell staining, cells were rinsed and incubated with calcein and PI for dead cells, for 30 min. Fluorescence microscopy was utilized to capture images of the stained cells. Concurrently, at designated intervals (24 and 48 h), the culture supernatant was removed, and 500 µL of prepared CCK-8 solution was added. Following an additional 2-hour incubation, absorbance readings at 450 nm were taken using a BioTek microplate reader. This procedure was replicated thrice for each experimental group to ensure consistency of results. Moreover, post-incubation with hydrogels, cells were harvested, centrifuged at 1500 rpm for 5 min, and subsequently fixed in 2.5% glutaraldehyde at 4°C overnight. The samples then underwent a meticulous dehydration process through a graded ethanol series (30%, 50%, 70%, 80%, 90%, and 100%), followed by freeze-drying. After being sputter-coated with platinum to enhance conductivity, the morphological characteristics of the cells were meticulously examined using scanning electron microscopy.
In vitro migration study
Initially, HUVEC cells were seeded into 6-well plates and allowed to incubate for 24 h. Following this period, a precise line was drawn through each well’s center, after which the wells were gently washed twice with PBS. The cells were then exposed to extracts of PADM@MgC, PADM@Mg, and PADM, as well as complete medium for comparative purposes. To monitor cellular migration, images were captured at the outset and again after 12 h of treatment.
Tube formation assay
Initially, each well of a 96-well plate was prepped with 50 µL of growth factor-reduced Matrigel, followed by a 30-minute incubation to ensure proper solidification of the Matrigel. Subsequently, 2 × 104 HUVECs were carefully inoculated into each well containing the solidified Matrigel substrate. These wells were then divided and co-cultured with high-glucose DMEM infused with extracts from PADM@MgC, PADM@Mg, and PADM, alongside a complete medium serving as the control. Twelve hours post-incubation, the cells were stained using a calcein staining kit. Representative images capturing the tube formation were taken 6 h after treatment to document the cellular responses.
Mouse wound model and treatment procedures
The Animal Ethics and Welfare Committee of Chang Zheng Hospital granted approval for all the animal experiments involved in this study, as documented by approval number 2023 − 564. All surgical interventions were meticulously executed in alignment with the established animal care guidelines. Male ICR mice, aged between 4 and 5 weeks and weighing approximately 18–20 g, were selected to establish a model for wound infection research. The procedure initiated with the careful removal of fur from the mice’s backs. This was followed by the creation of an 8 mm diameter wound on each mouse, which was subsequently inoculated with 10 µL of a bacterial solution at a concentration of 2 × 108 CFU/mL. On the second day post-wounding, the mice were systematically categorized into four experimental groups: control (Ctrl), PADM, PADM@Mg, and PADM@MgC, with each group comprising eight mice. In brief, MRSA-infected wounds were administered a single treatment of either control (PBS), PADM, PADM@Mg, or PADM@MgC during the entire experimental period. The mice were provided unrestricted access to food and water. They were housed in microinsulators under regulated conditions of humidity, temperature, and a 12-hour light-dark cycle. Daily digital photographs of the wounds were captured, and the wound area was quantitatively assessed using Image J software. The percentage of wound closure was calculated using the following formula:
Microbiological and histological examination
Upon euthanization of the mice on day 4 post-surgery, the infected tissues were meticulously harvested and homogenized in 5 mL of PBS for bacterial load assessment, with bacterial quantification executed as previously described. Subsequently, both wound and adjacent tissues were procured for comprehensive histological analysis. This included the application of Hematoxylin and Eosin (HE) staining and Giemsa staining to evaluate tissue morphology and infection status. Additionally, immunofluorescence techniques were employed to ascertain the expression levels of endogenous markers iNOS and CD206, providing insights into the inflammatory and vascular responses within the tissue.
Statistical analysis
Quantitative data were presented as the mean ± standard deviation (SD), except where noted differently. For the comparison between two distinct groups, a two-tailed Student’s t-test was employed. In cases involving multiple groups, analyses were performed using one-way analysis of variance (ANOVA), complemented by Tukey’s post hoc test for in-depth comparisons. All data calculations and statistical analyses were meticulously conducted using Excel 2016 and GraphPad Prism 9. The threshold for statistical significance was established at P < 0.05.
Data availability
No datasets were generated or analysed during the current study.
References
Lee SY, Jeon S, Kwon YW, Kwon M, Kang MS, Seong KY, Park TE, Yang SY, Han DW, Hong SW, Kim KS. Combinatorial wound healing therapy using adhesive nanofibrous membrane equipped with wearable LED patches for photobiomodulation. Sci Adv. 2022;8(15):eabn1646.
Yu R, Chen H, He J, Zhang Z, Zhou J, Zheng Q, Fu Z, Lu C, Lin Z, Caruso F, Zhang X. Engineering Antimicrobial Metal-Phenolic Network nanoparticles with High Biocompatibility for Wound Healing. Adv Mater 2023, e2307680.
Kamoun EA, Loutfy SA, Hussein Y, Kenawy ES. Recent advances in PVA-polysaccharide based hydrogels and electrospun nanofibers in biomedical applications: a review. Int J Biol Macromol. 2021;187:755–68.
Meftahi A, Samyn P, Geravand SA, Khajavi R, Alibkhshi S, Bechelany M, Barhoum A. Nanocelluloses as skin biocompatible materials for skincare, cosmetics, and healthcare: formulations, regulations, and emerging applications. Carbohydr Polym. 2022;278:118956.
Feng W, Wang Z. Tailoring the swelling-shrinkable behavior of hydrogels for Biomedical Applications. Adv Sci (Weinh) 2023, 10 (28), e2303326.
Lee J, Dutta SD, Acharya R, Park H, Kim H, Randhawa A, Patil TV, Ganguly K, Luthfikasari R, Lim KT. Stimuli-responsive 3D printable conductive hydrogel: a step toward regulating macrophage polarization and Wound Healing. Adv Healthc Mater 2023, e2302394.
Wang S, Wu S, Yang Y, Zhang J, Wang Y, Zhang R, Yang L. Versatile hydrogel Dressings that dynamically regulate the Healing of Infected Deep burn wounds. Adv Healthc Mater 2023, 12 (30), e2301224.
Xu A, Zhang N, Su S, Shi H, Lu D, Li X, Zhang X, Feng X, Wen Z, Ma G, Huang M, Huang C, Hu Y, Yuan H, Liu Q, Guan D, Wang J, Duan C. A highly stretchable, adhesive, and antibacterial hydrogel with chitosan and tobramycin as dynamic cross-linkers for treating the infected diabetic wound. Carbohydr Polym. 2024;324:121543.
Mu Z, ** T, Chu T, Lu H, Chen Y, Li S, Zeng B, Huang C, Lei K, Cai X, Deng H, Hu R. Functionalized MoS2-nanosheets with NIR-Triggered nitric oxide delivery and photothermal activities for synergistic antibacterial and regeneration-promoting therapy. J Nanobiotechnol. 2023;21(1):463.
Nie B, Huo S, Qu X, Guo J, Liu X, Hong Q, Wang Y, Yang J, Yue B. Bone infection site targeting nanoparticle-antibiotics delivery vehicle to enhance treatment efficacy of orthopedic implant related infection. Bioact Mater. 2022;16:134–48.
Li L, Wang Y, Huang Z, Xu Z, Cao R, Li J, Wu B, Lu JR, Zhu H. An additive-free multifunctional β-glucan-peptide hydrogel participates in the whole process of bacterial-infected wound healing. J Control Release. 2023;362:577–90.
Deng QS, Gao Y, Rui BY, Li XR, Liu PL, Han ZY, Wei ZY, Zhang CR, Wang F, Dawes H, Zhu TH, Tao SC, Guo SC. Double-network hydrogel enhanced by SS31-loaded mesoporous polydopamine nanoparticles: Symphonic collaboration of near-infrared photothermal antibacterial effect and mitochondrial maintenance for full-thickness wound healing in diabetes mellitus. Bioact Mater. 2023;27:409–28.
Liu W, Gao R, Yang C, Feng Z, Ou-Yang W, Pan X, Huang P, Zhang C, Kong D, Wang W. ECM-mimetic immunomodulatory hydrogel for methicillin-resistant Staphylococcus aureus-infected chronic skin wound healing. Sci Adv. 2022;8(27):eabn7006.
Wei Q, ** Z, Zhang W, Zhao Y, Wang Y, Wei Y, He X, Ma G, Guo Y, Jiang Y, Hu Z. Honokiol@PF127 crosslinked hyaluronate-based hydrogel for promoting wound healing by regulating macrophage polarization. Carbohydr Polym. 2023;303:120469.
Yu Q, Sun H, Yue Z, Yu C, Jiang L, Dong X, Yao M, Shi M, Liang L, Wan Y, Zhang H, Yao F, Li J. Zwitterionic Polysaccharide-based hydrogel dressing as a stem cell carrier to accelerate burn Wound Healing. Adv Healthc Mater 2022, e2202309.
**a L, Wu T, Chen L, Mei P, Liu L, Li R, Shu M, Huan Z, Wu C, Fang B. Silicon-based Biomaterials Modulate the adaptive Immune response of T lymphocytes to promote Osteogenesis/angiogenesis via epigenetic regulation. Adv Healthc Mater 2023, e2302054.
Bian J, Cai F, Chen H, Tang Z, ** K, Tang J, Wu L, Xu Y, Deng L, Gu Y, Cui W, Chen L. Modulation of local overactive inflammation via Injectable Hydrogel Microspheres. Nano Lett. 2021;21(6):2690–8.
Gui S, Tang W, Huang Z, Wang X, Gui S, Gao X, **ao D, Tao L, Jiang Z, Wang X. Ultrasmall Coordination Polymer Nanodots Fe-Quer Nanozymes for preventing and delaying the Development and Progression of Diabetic Retinopathy. Adv Funct Mater. 2023;33(36):2300261.
Yuan R, Li Y, Han S, Chen X, Chen J, He J, Gao H, Yang Y, Yang S, Yang Y. Fe-Curcumin nanozyme-mediated reactive oxygen species scavenging and anti-inflammation for Acute Lung Injury. ACS Cent Sci. 2022;8(1):10–21.
Hatcher H, Planalp R, Cho J, Torti FM, Torti SV. Curcumin: from ancient medicine to current clinical trials. Cell Mol Life Sci. 2008;65(11):1631–52.
Lopresti AL. The Problem of Curcumin and its bioavailability: could its gastrointestinal influence contribute to its overall Health-Enhancing effects? Adv Nutr. 2018;9(1):41–50.
Lv G-P, Hu D-J, Zhou Y-Q, Zhang Q-W, Zhao J, Li S-P. Preparation and application of standardized typical Volatile Components Fraction from Turmeric (Curcuma longa L.) by supercritical fluid extraction and step molecular distillation. Molecules. 2018;23(7):1831.
Sun T, Jiang D, Rosenkrans ZT, Ehlerding EB, Ni D, Qi C, Kutyreff CJ, Barnhart TE, Engle JW, Huang P, Cai W. A melanin-based natural antioxidant Defense Nanosystem for Theranostic Application in Acute kidney Injury. Adv Funct Mater. 2019;29(48):1904833.
Bagheri H, Ghasemi F, Barreto GE, Rafiee R, Sathyapalan T, Sahebkar A. Effects of curcumin on mitochondria in neurodegenerative diseases. BioFactors. 2020;46(1):5–20.
Wei H, Jiang D, Yu B, Ni D, Li M, Long Y, Ellison PA, Siamof CM, Cheng L, Barnhart TE, Im HJ, Yu F, Lan X, Zhu X, He Q, Cai W. Nanostructured polyvinylpyrrolidone-curcumin conjugates allowed for kidney-targeted treatment of cisplatin induced acute kidney injury. Bioact Mater. 2023;19:282–91.
Cao F, Gui S-Y, Gao X, Zhang W, Fu Z-Y, Tao L-M, Jiang Z-X, Chen X, Qian H, Wang X. Research progress of natural product-based nanomaterials for the treatment of inflammation-related diseases. Mater Design. 2022;218:110686.
Zhou Z, Gong F, Zhang P, Wang X, Zhang R, **a W, Gao X, Zhou X, Cheng L. Natural product curcumin-based coordination nanoparticles for treating osteoarthritis via targeting Nrf2 and blocking NLRP3 inflammasome. Nano Res. 2022;15(4):3338–45.
Chen S, Yu Y, **e S, Liang D, Shi W, Chen S, Li G, Tang W, Liu C, He Q. Local H2 release remodels senescence microenvironment for improved repair of injured bone. Nat Commun. 2023;14(1):7783.
Liu C, Liu W, Qi B, Fan L, Liu S, Yang Q, Yang Y, Yang S, Zhang Y, Wei X, Zhu L. Bone homeostasis modulating Orthopedic Adhesive for the closed-Loop management of osteoporotic fractures. Small 2023, 19 (48), e2302704.
Zhu S, Li M, Wang Z, Feng Q, Gao H, Li Q, Chen X, Cao X. Bioactive glasses-based Nanozymes Composite Macroporous Cryogel with Antioxidative, Antibacterial, and Pro-healing Properties for Diabetic infected Wound Repair. Adv Healthc Mater 2023, 12 (29), e2302073.
Huo S, Liu S, Liu Q, **e E, Miao L, Meng X, Xu Z, Zhou C, Liu X, Xu G. Copper–Zinc-Doped Bilayer Bioactive Glasses Loaded Hydrogel with Spatiotemporal Immunomodulation Supports MRSA-Infected Wound Healing. Advanced Science n/a (n/a), 2302674.
Richter RF, Vater C, Korn M, Ahlfeld T, Rauner M, Pradel W, Stadlinger B, Gelinsky M, Lode A, Korn P. Treatment of critical bone defects using calcium phosphate cement and mesoporous bioactive glass providing spatiotemporal drug delivery. Bioact Mater. 2023;28:402–19.
Huo S, Wang F, Lyu Z, Hong Q, Nie Be, Wei J, Wang Y, Zhang J, Yue B. Dual-functional polyetheretherketone surface modification for regulating immunity and bone metabolism. Chem Eng J. 2021;426:130806.
Su X, Lyu Z, Wu Y, Gu Y-H, Huo S, Zhou C. Strontium-doped bioactive glass/PDA functionalized polyetheretherketone with immunomodulatory property for enhancing photothermal clearance of Staphylococcus aureus. Mater Design. 2023;225:111552.
Haidari H, Kopecki Z, Sutton AT, Garg S, Cowin AJ, Vasilev K. pH-Responsive smart hydrogel for controlled delivery of silver nanoparticles to infected wounds. Antibiot (Basel) 2021, 10 (1).
Zhang M, Wang D, Ji N, Lee S, Wang G, Zheng Y, Zhang X, Yang L, Qin Z, Yang Y. Bioinspired Design of Sericin/Chitosan/Ag@MOF/GO hydrogels for efficiently combating resistant Bacteria, Rapid Hemostasis, and Wound Healing. Polym (Basel). 2021;13:16.
Li Y, Li G, Sha X, Li L, Zhang K, Liu D, Hao Y, Cui X, Wang L, Wang H. An intelligent Vancomycin release system for preventing surgical site infections of bone tissues. Biomater Sci. 2020;8(11):3202–11.
Cai D, Chen S, Wu B, Chen J, Tao D, Li Z, Dong Q, Zou Y, Chen Y, Bi C, Zu D, Lu L, Fang B. Construction of multifunctional porcine acellular dermal matrix hydrogel blended with Vancomycin for hemorrhage control, antibacterial action, and tissue repair in infected trauma wounds. Mater Today Bio. 2021;12:100127.
Haidari H, Kopecki Z, Bright R, Cowin AJ, Garg S, Goswami N, Vasilev K. Ultrasmall AgNP-Impregnated biocompatible hydrogel with highly effective Biofilm Elimination properties. ACS Appl Mater Interfaces. 2020;12(37):41011–25.
Naahidi S, Jafari M, Logan M, Wang Y, Yuan Y, Bae H, Dixon B, Chen P. Biocompatibility of hydrogel-based scaffolds for tissue engineering applications. Biotechnol Adv. 2017;35(5):530–44.
Huo S, Liu S, Liu Q, **e E, Miao L, Meng X, Xu Z, Zhou C, Liu X, Xu G. Copper-zinc-doped Bilayer Bioactive glasses Loaded Hydrogel with Spatiotemporal Immunomodulation supports MRSA-Infected Wound Healing. Adv Sci (Weinh) 2023, e2302674.
Dong Q, Zu D, Kong L, Chen S, Yao J, Lin J, Lu L, Wu B, Fang B. Construction of antibacterial nano-silver embedded bioactive hydrogel to repair infectious skin defects. Biomater Res. 2022;26(1):36.
Chen Y, Dan N, Dan W, Liu X, Cong L. A novel antibacterial acellular porcine dermal matrix cross-linked with oxidized chitosan oligosaccharide and modified by in situ synthesis of silver nanoparticles for wound healing applications. Mater Sci Eng C Mater Biol Appl. 2019;94:1020–36.
Zhang Y, Chen Y, Zhao B, Gao J, **a L, **ng F, Kong Y, Li Y, Zhang G. Detection of type I and III collagen in porcine acellular matrix using HPLC–MS. Regenerative Biomaterials. 2020;7(6):577–82.
Kim H, Wang SY, Kwak G, Yang Y, Kwon IC, Kim SH. Exosome-guided phenotypic switch of M1 to M2 macrophages for Cutaneous Wound Healing. Adv Sci (Weinh). 2019;6(20):1900513.
Spiller KL, Nassiri S, Witherel CE, Anfang RR, Ng J, Nakazawa KR, Yu T, Vunjak-Novakovic G. Sequential delivery of immunomodulatory cytokines to facilitate the M1-to-M2 transition of macrophages and enhance vascularization of bone scaffolds. Biomaterials. 2015;37:194–207.
Brauneck F, Fischer B, Witt M, Muschhammer J, Oelrich J, da Costa Avelar PH, Tsoka S, Bullinger L, Seubert E, Smit DJ. TIGIT blockade repolarizes AML-associated TIGIT + M2 macrophages to an M1 phenotype and increases CD47-mediated phagocytosis. J Immunother Cancer. 2022;10:12.
Berbudi A, Anugerah Ramadhan MT, Atik N. REPORT-Effect of topical Curcuma longa extract gel on incision wound angiogenesis in Balb/C mice. Pak J Pharm Sci. 2021;34(3):1023–9.
Acknowledgements
This work was supported by a research grant from the Shanghai Sailing Program (Grant No. 21YF1458200) and the National Natural Foundation of China (Grant No. 82272533, 81972076).
Author information
Authors and Affiliations
Contributions
**aogang Bao, Shicheng Huo, and Zhenhua Wang designed the experiments. Shengyan Yang and Lingyun Dou performed the synthesis and characterization of the materials. Yifei Liu and Jian Huang performed the in vitro experiments. Jian Huang, Chang Cai, and Shicheng Huo participated in the in vivo experiments. **aogang Bao, Bin Fang, and Guohua Xu contributed to data analysis. **aogang Bao, Shicheng Huo, and Guohua Xu contributed to the manuscript preparation. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bao, X., Huo, S., Wang, Z. et al. Multifunctional biomimetic hydrogel dressing provides anti-infection treatment and improves immunotherapy by reprogramming the infection-related wound microenvironment. J Nanobiotechnol 22, 80 (2024). https://doi.org/10.1186/s12951-024-02337-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-024-02337-3