Abstract
Background
Bladder cancer is having a gradually increasing incidence in China. Except for the traditional chemotherapy drugs, there are no emerging new drugs for almost 30 years in bladder cancer. New potential therapeutic targets and biomarkers are urgently needed.
Methods
BORA is the activator of kinase Aurora A and plays an important role in cell cycle progression. To investigate the function of BORA in BCa, we established BORA knockdown and overexpression cell models for in vitro studies, xenograft and pulmonary metastasis mouse models for in vivo studies.
Results
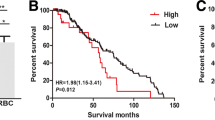
Our results indicated that BORA was upregulated in human bladder cancer (BCa) compared to the normal bladder and paracancerous tissues at transcriptional and translational levels. We found that BORA was positively related to BCa cell proliferation. Furthermore, BORA knockdown induced cell cycle arrest in G2/M phase while BORA overexpression decreased the proportion of cells in G2/M, associated with PLK1–CDC25C–CDK1 alteration. Interestingly, we observed that knockdown of BORA inhibited BCa cell migration and invasion, accompanied with alterations of epithelial–mesenchymal transition (EMT) pathway related proteins. In vivo studies confirmed the inhibition effect of BORA knockdown on BCa cell growth and migration.
Conclusions
Our study indicates that BORA regulates BCa cell cycle and growth, meanwhile influences cell motility by EMT, and could be a novel biomarker and potential therapeutic target in BCa.
Similar content being viewed by others
Background
As the ninth most common cancer worldwide [1], bladder cancer (BCa) is having a gradually increasing incidence in China [2]. Most of the newly diagnosed cases are non-muscle invasive BCa. Even with transurethral resection of tumor, BCa still has a very high recurrence rate [3]. Chemotherapy based on cisplatin has improved the outcome modestly. For cisplatin-ineligible patients, T-cell checkpoint inhibitors have presented some benefits to those having high PD-L1 expression in some trials [4,5,6]. Except for the traditional chemotherapy drugs, there are no emerging new drugs for almost 30 years in BCa [7]. Therefore, to enhance the targeted and personalized therapy, molecular analysis to find more new specific markers and therapeutic targets is of great urgent.
BORA encoded protein activates kinase Aurora A, and is very important in spindle assembly, centrosome maturation and the process of mitosis. BORA was identified as a cell cycle co-factor protein of Aurora A in the first place [8]. Binding with pole-like kinase 1 (PLK1), BORA forms a PLK1/BORA complex and recruits Aurora A to the T-loop of PLK1 T210 phosphorylation site to activate PLK1, thus promote mitotic entry [9]. PLK1 and Aurora A are critical regulators of cell cycle, which has a fundamental role in cell proliferation, and related to the checkpoint recovery when DNA damage appears in cells where it leads to DNA repair or progress to apoptosis [10, 11]. A variety of cell cycle related regulators have been explored as therapeutic targets and biomarkers [35]. However, some studies also showed that PLK1 and Aurora A conversely had an influence on BORA activity through posttranslational modifications [8, 36]. Recent studies demonstrated that CDK1 regulated the activation of BORA by phosphorylating 3 conserved sites located at the N-terminal part of BORA, which are Cyclin docking sites [20, 37]. Once mutated the three phosphorylation sites of BORA, PLK1 could not be activated by Aurora A at T210 on the T-loop. During DNA damage recovery, it is important for cells to maintain the G2 checkpoint, which provides cells with time for DNA repair or progress to apoptosis. Cairns et al. reported that BORA was significantly related to radiosensitivity by regulating DNA repair and MDC1, and BORA affected irradiation response via a different pathway from PLK1 [19]. We detected the expression of cell cycle proteins and found that PLK1 and CDC25C were upregulated, while CDK1 and CDK2 were downregulated after knockdown of BORA. Moreover, the protein changes were reversed after BORA overexpression in BCa cells (Fig. 3). GSK3β activation was reported to be important for BORA [38]. We noticed a downregulation of GSK3β after BORA knockdown in UM-UC-3 cells (data not shown). However, the exact mechanism of how BORA regulates and be regulated in the feedback loops still needs to be further explored.
Interestingly, after knockdown of BORA, we noticed that BCa cell migration and invasion were inhibited, which has not been reported anywhere else (Fig. 4). We observed upregulated epithelial marker E-cadherin in BORA knockdown cells and downregulated N-cadherin, Vimentin and other proteins associated with EMT pathway, which has been verified to play a critical role in migration and invasion of cancer cells [39]. But how reduced BORA exactly regulates EMT still needs further detections. To confirm our in vitro results, we established stable cell lines of BORA knockdown through lentiviral packaging. Xenografts and pulmonary metastasis mice model were established by subcutaneously and intravenously injecting BCa cells, respectively. In vivo, we also found reduced BCa cell growth and migration after knockdown of BORA (Fig. 5).
Recently, a large number of Aurora A and PLK1 inhibitors were reported to be evaluated in clinical trials as anticancer drugs but showed modest effect against solid tumors [40]. BORA, as the key intermediate protein of Aurora A and PLK1, was reported to be a potential biomarker for prognosis in lung, breast, and gastric adenocarcinomas [18]. Our results also showed that BORA knockdown could suppress BCa cell growth and migration both in vitro and in vivo. Researches about the effect of BORA in cancers are still too less. And how PLK1 and Aurora A inhibitors affect solid tumors after blockading BORA needs to be further investigated. As a signaling node of the BORA–PLK1–CDC25–CDK1 feedback loop and Aurora A-BORA-PLK1 axis, BORA is likely to have exciting prospects as a potential target.
Conclusions
In conclusion, our study revealed that BORA positively associated with BCa cell growth and regulated cell cycle. For the first time, we found that BORA knockdown could suppress BCa cell migration and invasion possibly through EMT pathway. BORA has the potential to become a new biomarker and possible therapeutic target in BCa.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- BCa:
-
Bladder cancer
- EMT:
-
Epithelial–mesenchymal transition
- GEPIA:
-
Gene Expression Profiling Interactive Analysis
- H&E:
-
Hematoxylin and eosin
- IF:
-
Immunofluorescence
- IHC:
-
Immunohistochemistry
- PLK1:
-
Pole-like kinase 1
- WB:
-
Western blot
References
Antoni S, Ferlay J, Soerjomataram I, Znaor A, Jemal A, Bray F. Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol. 2017;71(1):96–108.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Prasad SM, Decastro GJ, Steinberg GD. Medscape: urothelial carcinoma of the bladder: definition, treatment and future efforts. Nat Rev Urol. 2011;8(11):631–42.
Balar AV, Galsky MD, Rosenberg JE, Powles T, Petrylak DP, Bellmunt J, Loriot Y, Necchi A, Hoffman-Censits J, Perez-Gracia JL, et al. Atezolizumab as first-line treatment in cisplatin-ineligible patients with locally advanced and metastatic urothelial carcinoma: a single-arm, multicentre, phase 2 trial. Lancet. 2017;389(10064):67–76.
Bellmunt J, de Wit R, Vaughn DJ, Fradet Y, Lee JL, Fong L, Vogelzang NJ, Climent MA, Petrylak DP, Choueiri TK, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015–26.
Sonpavde G. PD-1 and PD-L1 inhibitors as salvage therapy for urothelial carcinoma. N Engl J Med. 2017;376(11):1073–4.
Zhang Z, Zhang G, Kong C. Targeted inhibition of Polo-like kinase 1 by a novel small-molecule inhibitor induces mitotic catastrophe and apoptosis in human bladder cancer cells. J Cell Mol Med. 2017;21(4):758–67.
Hutterer A, Berdnik D, Wirtz-Peitz F, Zigman M, Schleiffer A, Knoblich JA. Mitotic activation of the kinase Aurora-A requires its binding partner Bora. Dev Cell. 2006;11(2):147–57.
Bruinsma W, Aprelia M, Garcia-Santisteban I, Kool J, Xu YJ, Medema RH. Inhibition of Polo-like kinase 1 during the DNA damage response is mediated through loss of Aurora A recruitment by Bora. Oncogene. 2017;36(13):1840–8.
van Vugt MA, Bras A, Medema RH. Polo-like kinase-1 controls recovery from a G2 DNA damage-induced arrest in mammalian cells. Mol Cell. 2004;15(5):799–811.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Ju LG, Zhu Y, Long QY, Li XJ, Lin X, Tang SB, Yin L, **ao Y, Wang XH, Li L, et al. SPOP suppresses prostate cancer through regulation of CYCLIN E1 stability. Cell Death Differ. 2019;26(6):1156–68.
Zhou N, Singh K, Mir MC, Parker Y, Lindner D, Dreicer R, Ecsedy JA, Zhang Z, Teh BT, Almasan A, et al. The investigational Aurora kinase A inhibitor MLN8237 induces defects in cell viability and cell-cycle progression in malignant bladder cancer cells in vitro and in vivo. Clin Cancer Res. 2013;19(7):1717–28.
Gjertsen BT, Schoffski P. Discovery and development of the Polo-like kinase inhibitor volasertib in cancer therapy. Leukemia. 2015;29(1):11–9.
Graff JN, Higano CS, Hahn NM, Taylor MH, Zhang B, Zhou X, Venkatakrishnan K, Leonard EJ, Sarantopoulos J. Open-label, multicenter, phase 1 study of alisertib (MLN8237), an aurora A kinase inhibitor, with docetaxel in patients with solid tumors. Cancer. 2016;122(16):2524–33.
Pujade-Lauraine E, Selle F, Weber B, Ray-Coquard IL, Vergote I, Sufliarsky J, Del Campo JM, Lortholary A, Lesoin A, Follana P, et al. Volasertib Versus chemotherapy in platinum-resistant or -refractory ovarian cancer: a randomized phase II Groupe des Investigateurs Nationaux pour l’Etude des Cancers de l’Ovaire Study. J Clin Oncol. 2016;34(7):706–13.
Cirillo L, Thomas Y, Pintard L, Gotta M. BORA-dependent PLK1 regulation: a new weapon for cancer therapy? Mol Cell Oncol. 2016;3(5):e1199265.
Zhang QX, Gao R, **ang J, Yuan ZY, Qian YM, Yan M, Wang ZF, Liu Q, Zhao HD, Liu CH. Cell cycle protein Bora serves as a novel poor prognostic factor in multiple adenocarcinomas. Oncotarget. 2017;8(27):43838–52.
Cairns J, Peng Y, Yee VC, Lou Z, Wang L. Bora downregulation results in radioresistance by promoting repair of double strand breaks. PLoS ONE. 2015;10(3):e0119208.
Parrilla A, Cirillo L, Thomas Y, Gotta M, Pintard L, Santamaria A. Mitotic entry: the interplay between Cdk1, Plk1 and Bora. Cell Cycle. 2016;15(23):3177–82.
Wang G, Cao R, Wang Y, Qian G, Dan HC, Jiang W, Ju L, Wu M, **ao Y, Wang X. Simvastatin induces cell cycle arrest and inhibits proliferation of bladder cancer cells via PPARgamma signalling pathway. Sci Rep. 2016;6:35783.
Cheng S, Wang G, Wang Y, Cai L, Qian K, Ju L, Liu X, **ao Y, Wang X. Fatty acid oxidation inhibitor etomoxir suppresses tumor progression and induces cell cycle arrest via PPARgamma-mediated pathway in bladder cancer. Clin Sci (Lond). 2019;133(15):1745–58.
Cao R, Wang G, Qian K, Chen L, Ju L, Qian G, Wu CL, Dan HC, Jiang W, Wu M, et al. TM4SF1 regulates apoptosis, cell cycle and ROS metabolism via the PPARgamma-SIRT1 feedback loop in human bladder cancer cells. Cancer Lett. 2018;414:278–93.
Lu M, Ge Q, Wang G, Luo Y, Wang X, Jiang W, Liu X, Wu CL, **ao Y, Wang X. CIRBP is a novel oncogene in human bladder cancer inducing expression of HIF-1alpha. Cell Death Dis. 2018;9(10):1046.
Cheng S, Qian K, Wang Y, Wang G, Liu X, **ao Y, Wang X. PPARgamma inhibition regulates the cell cycle, proliferation and motility of bladder cancer cells. J Cell Mol Med. 2019;23(5):3724–36.
Zhou Q, Chen S, Lu M, Luo Y, Wang G, **ao Y, Ju L, Wang X. EFEMP2 suppresses epithelial-mesenchymal transition via Wnt/beta-catenin signaling pathway in human bladder cancer. Int J Biol Sci. 2019;15(10):2139–55.
Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45(W1):W98–102.
Cuylen S, Blaukopf C, Politi AZ, Muller-Reichert T, Neumann B, Poser I, Ellenberg J, Hyman AA, Gerlich DW. Ki-67 acts as a biological surfactant to disperse mitotic chromosomes. Nature. 2016;535(7611):308–12.
Zaidi SK, Young DW, Montecino MA, Lian JB, van Wijnen AJ, Stein JL, Stein GS. Mitotic bookmarking of genes: a novel dimension to epigenetic control. Nat Rev Genet. 2010;11(8):583–9.
Kumagai A, Dunphy WG. Purification and molecular cloning of Plx1, a Cdc25-regulatory kinase from Xenopus egg extracts. Science. 1996;273(5280):1377–80.
Abbas T, Dutta A. p21 in cancer: intricate networks and multiple activities. Nat Rev Cancer. 2009;9(6):400–14.
Brabletz T, Kalluri R, Nieto MA, Weinberg RA. EMT in cancer. Nat Rev Cancer. 2018;18(2):128–34.
Macurek L, Lindqvist A, Lim D, Lampson MA, Klompmaker R, Freire R, Clouin C, Taylor SS, Yaffe MB, Medema RH. Polo-like kinase-1 is activated by aurora A to promote checkpoint recovery. Nature. 2008;455(7209):119–23.
Jang YJ, Ma S, Terada Y, Erikson RL. Phosphorylation of threonine 210 and the role of serine 137 in the regulation of mammalian polo-like kinase. J Biol Chem. 2002;277(46):44115–20.
Seki A, Cop**er JA, Jang CY, Yates JR, Fang G. Bora and the kinase Aurora a cooperatively activate the kinase Plk1 and control mitotic entry. Science. 2008;320(5883):1655–8.
Chan EH, Santamaria A, Sillje HH, Nigg EA. Plk1 regulates mitotic Aurora A function through betaTrCP-dependent degradation of hBora. Chromosoma. 2008;117(5):457–69.
Thomas Y, Cirillo L, Panbianco C, Martino L, Tavernier N, Schwager F, Van Hove L, Joly N, Santamaria A, Pintard L, et al. Cdk1 phosphorylates SPAT-1/Bora to promote Plk1 activation in C. elegans and human cells. Cell Rep. 2016;15(3):510–8.
Lee YC, Liao PC, Liou YC, Hsiao M, Huang CY, Lu PJ. Glycogen synthase kinase 3 beta activity is required for hBora/Aurora A-mediated mitotic entry. Cell Cycle. 2013;12(6):953–60.
Dongre A, Weinberg RA. New insights into the mechanisms of epithelial-mesenchymal transition and implications for cancer. Nat Rev Mol Cell Biol. 2019;20(2):69–84.
Lens SM, Voest EE, Medema RH. Shared and separate functions of polo-like kinases and aurora kinases in cancer. Nat Rev Cancer. 2010;10(12):825–41.
Acknowledgements
We appreciate the great help of technical assistance from Ms. Yuan Zhu, Ms. Yayun Fang and Ms. Danni Shan.
Funding
We are grateful for the tremendous support from China Scholarship Council.
Author information
Authors and Affiliations
Contributions
SC, TP and LJ designed and conducted the experiment. SC, XZ, FZ and GW collected data and analyzed. LJ, SC, XL, YX and XW wrote and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Bladder tissues were collected from the surgery of patients at Zhongnan Hospital of Wuhan University, and the normal tissues were from donors with accidental death. Tissues were obtained and stored following the protocol of Zhongnan Hospital Biobank. The study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects and legally authorized representatives, and the approval of bladder tissues use was obtained from the Ethics Committee of Zhongnan Hospital (approval no. 2015029).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
Validation of BORA knockdown and overexpression. Knockdown efficiency of BORA-siRNA in (A) UM-UC-3 and (B) 5637 cells. (C) WB confirmed the knockdown of BORA. (D) BORA overexpression was verified by qPCR and (E) WB assay. (F) Apoptosis analysis of BORA knockdown. ** p < 0.01, *** p < 0.001, n.s. means no significance. Table S1. List of primary antibodies. Table S2. List of secondary antibodies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, S., Peng, T., Zhu, X. et al. BORA regulates cell proliferation and migration in bladder cancer. Cancer Cell Int 20, 290 (2020). https://doi.org/10.1186/s12935-020-01392-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-020-01392-8