Abstract
Background
Vitamin D status has been hypothesized to protect against development of diabetic retinopathy via its anti-inflammatory and anti-angiogenic properties. Additionally, in vitro and in vivo studies suggest vitamin D favorably influences blood pressure and blood glucose control, strong risk factors for diabetic retinopathy. We examined the association between vitamin D status and prevalent diabetic retinopathy in participants with diabetes from a population-based cohort.
Methods
Among participants in the Atherosclerosis Risk in Communities (ARIC) study with diabetes at visit 3 (1993–1995), 1339 (906 Caucasians, 433 African Americans) had serum 25-hydroxyvitamin (25[OH]D) concentrations assessed at visit 2 (1989–1992) and nonmydriatic retinal photographs taken at visit 3. Dietary intake of vitamin D was assessed at visit 1 (1987–1989). Logistic regression was used to estimate odds ratios (ORs) and 95 % confidence intervals (CIs) for diabetic retinopathy by categories of season-adjusted 25(OH)D (<30 [referent], 30–<50, 50–<75 and ≥75 nmol/L), by quartile of vitamin D intake (IU/day), and use of vitamin D or fish oil supplements (yes/no). P for trend was estimated using continuous 25(OH)D or vitamin D intake. ORs were adjusted for race, and duration of diabetes. We further adjusted for HBA1c and hypertension to examine if 25(OH)D influenced diabetic retinopathy via its effects on either glycemic control or blood pressure.
Results
ORs (95 % CIs) for retinopathy, adjusted for race and duration, were 0.77 (0.45–1.32), 0.64 (0.37–1.10), and 0.39 (0.20–0.75), p for trend = 0.001, for participants with 25(OH)D of 30–<50, 50–<75, and ≥75 nmol/L, respectively. Further adjustment for hypertension minimally influenced results (data not show), but adjustment for HBA1c attenuated the OR among those with 25(OH)D ≥75 (0.47 [0.23–0.96], p for trend = 0.030). No statistically significant association was observed between vitamin D intake from foods or supplements and retinopathy.
Conclusions
25(OH)D concentrations ≥75 nmol/L were associated with lower odds of any retinopathy assessed 3 years later. We speculate this may be due in part to vitamin D’s influence on blood glucose control.
Similar content being viewed by others
Background
Diabetic retinopathy is a leading cause of blindness in adults aged 20–74 years in the United States. Among individuals with diabetes it has direct influences on quality of life and functional independence of aging, affecting ~28.5 % of people with diabetes ≥40 years [1]. Modifiable nutritional factors may influence risk for diabetic retinopathy, but they have been relatively understudied in epidemiologic investigations [2]. Accumulating evidence from some [3–13], but not all [14–23], epidemiologic studies suggest that vitamin D status may be a novel modifiable risk factor for diabetic retinopathy.
Vitamin D status is hypothesized to affect risk for retinopathy [4] due to its immunomodulatory properties [24] as chronic low grade inflammation is hypothesized to promote the development of retinopathy [25]. Vitamin D is also hypothesized to positively regulate hypertension [26] and blood glucose control [27], both of which are strong risk factors for retinopathy [28, 29].
Using data from the prospective, population-based Atherosclerosis Risk in Communities (ARIC) Study, we investigated associations between vitamin D status, assessed with the blood biomarker of serum 25-hydroxyvitamn D (25[OH]D), and prevalent diabetic retinopathy assessed from graded fundus photographs taken 3 years later among Caucasian and African American participants with primarily type 2 diabetes (n = 1339). 25(OH)D reflects vitamin D from all sources (sunlight, diet and supplements). We hypothesized that individuals with higher 25(OH)D concentrations would have lower odds of retinopathy than participants with lower concentrations. We examined the extent to which this association was mediated by blood pressure or blood glucose control. We also explored associations between self-reported intake of vitamin D from foods and the odds of retinopathy.
Methods
Study sample
The ARIC Study, a population-based prospective study [30], recruited participants from Forsyth County, North Carolina; Jackson, Mississippi; the northwestern suburbs of Minneapolis, Minnesota; and Washington County, Maryland. Eligible participants were between 45 and 65 years of age at visit 1 (1987–1989) and intended to remain in the community in which they lived. All participants provided signed informed consent and the study protocol was approved by the institutional review boards at each ARIC study site and complies with the Helsinki Declaration as revised in 1983.
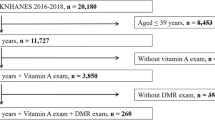
The present analyses use data collected at visits 1 (1987–1989), 2 (1990–1992) and 3 (1993–1995). This study sample consists of Caucasian and African American participants who were classified as having diabetes (fasting blood glucose of 126 mg/dl or non-fasting blood glucose of 200 mg/dl; self-report of a diabetes diagnosis; or use of medication for diabetes in the 2 weeks prior to the visit) at study visit 3, had gradable retinal fundus photos at visit 3 and serum 25(OH)D measures at visit 2. This was a retrospective analysis to examine the association between serum draw at visit 2, but recently (2012–2013) analyzed for 25(OH)D concentrations, and the prevalence of diabetic retinopathy determined 3 years later at visit 3.
There were 15,792 participants enrolled at visit 1, of which 12,887 attended visit 3. We excluded 796 participants who did not consent to use of their data to study outcomes other than cardiovascular disease. Of the remaining 12,091 participants, 1899 were classified as having diabetes of whom 350 were missing data on retinopathy status (301 missing retinal photos and 49 with upgradable photos), 186 were missing serum 25(OH)D, 8 identified as neither African American nor Caucasian, and 16 were missing data on pertinent covariates (glycosylated hemoglobin A1c [HBA1c] or hypertension), providing a sample of 1339 participants. Analyses involving dietary vitamin D data had 1305 participants due to missing data on diet at visit 1.
Retinal photography
Diabetic retinopathy was determined from grading of fundus photographs taken at visit three of one randomly selected eye. Participants sat in a dark room for 5 min to allow for nonpharmocological pupil dilution [31]. One 45-degree nonmydriatic retinal photograph was taken with a Canon CR-45UAF nonmydriatic film camera (Canon USA, Itasca, IL) and was centered to include the optic disc and the macula [31]. Fundus photographs were graded for the presence and severity of retinopathy at the University of Wisconsin Fundus Photograph Reading Center using a standard grading system, the modified Arlie House classification scheme [32]. Twenty-one percent (n = 280 of 1339) of participants had any retinopathy, of which 207 had mild non-proliferative diabetic retinopathy (NPDR), 44 had moderate to severe NPDR, 29 had proliferative diabetic retinopathy (PDR), and 3 had macular edema.
Assessment of 25(OH)D
Vitamin D status was assessed by analyzing participants’ serum from fasting blood drawn at visit 2 for 25(OH)D concentrations (sum of 25[OH]D2 and 25[OH]D3) using liquid chromatography in tandem with high-sensitivity mass spectrometry (LC–MS) (Waters Alliance e2795; Waters, Milford, MA, USA) at the Collaborative Studies Clinical Laboratory at Fairview University Medical Center (Minneapolis, MN), as previously described [33]. Serum samples were stored at −80 °C from 1990–1992 until assessment of 25(OH)D from 2012 to 2013 [33]. The coefficient of variation, representing sample processing and laboratory error was 10.9 %. Differences in 25(OH)D concentrations due to season were accounted for using local regression [34]. 25(OH)D was regressed on day of blood draw and was conducted separately for Caucasians and African Americans. Residuals were added back to the sample mean (60.1 and 47.4 nmol/L for Caucasian and African Americans, respectively) and the season-adjusted values were used in all further mentioned analyses.
Assessment of dietary and supplemental vitamin D intake
Dietary intake of vitamin D was assessed at visit 1 using a reliable and previously validated Willett 66-item semi-quantitative food frequency questionnaire (FFQ) [35, 36]. At visit 3, participants were asked about their use of vitamin D and fish oil supplements, as source of vitamin D. They were asked if they took fish oil (including omega-3 fatty acids, eicosapentaenoic acid [EPA], and cod liver oil), the duration of use, and the dose per week. Participants were also asked whether or not they took vitamin D “on a regular basis,” but no additional information was asked on duration of use or dose. There were 48 participants who reported use of either vitamin D or fish oil at visit 3.
Assessment of additional participant characteristics
At each visit trained study personnel collected information on participants’ demographic factors, health history, family health history, smoking, medication use and other potential risk factors for cardiovascular disease [30]. Blood collected at visit 2 [37] was assessed for serum glucose, HBA1c [38], hematocrit level [37], total plasma cholesterol, plasma triglyceride, low density lipoprotein (LDL), and high density lipoprotein (HDL) cholesterol concentrations [39].
Physical activity was assessed at visit 1 using a modified version [40] of the previously validated [41, 42] Baecke questionnaire from which we created a composite physical activity index score ranging from 0 (low overall physical activity) to 6. Duration of diabetes was defined as <3 years, 3 to <6, and ≥6 years determined using data on self-reported diabetes diagnosis, fasting and non-fasting blood glucose levels, and diabetes medication use collected at visits 1, 2 or 3. 25(OH)D concentrations and other covariate data used in these analyses were assessed at visit 2 with the exception of information on education, diet, physical activity (visit 1), and duration of diabetes (visit 3).
Statistical analysis
Guided by the Institute of Medicine, vitamin D status was defined using 25(OH)D concentrations (nmol/L) as deficient (<30), inadequate (>30 to ≤50), and using two categories within the concentrations considered adequate (>50 to <75 and ≥75) [43]. Participant characteristics and risk factors for retinopathy were examined by vitamin D status, as well as by presence of retinopathy (any versus none), using t-tests, ANOVAs or Chi square tests.
Logistic regression was used to estimate the odds ratios (ORs) and 95 % confidence intervals (95 % CIs) for any prevalent retinopathy (both NPDR and PDR) by vitamin D status with the referent category of deficient status (<30 nmol/L) [43]. We also estimate the odds of having PDR or macular edema (n = 31) among participants with 25(OH)D ≥50 compared to <50 nmol/L. We had to apply the Firth bias-correction method for quasi-complete separation [44] due to the low number of outcomes. The ORs and 95 % CIs for retinopathy per 10 nmol/L difference in 25(OH)D are also presented and p-for trend analyses were conducted using 25(OH)D as a continuous variable.
Age, sex, race, education, duration of diabetes, smoking status, drinking status, ethanol intake, physical activity index score, body mass index (BMI), waist circumference, hematocrit level, LDL, HDL, total cholesterol and triglyceride concentrations were assessed as potential confounders of the vitamin D status and retinopathy association. If these variables were associated with either vitamin D status or prevalent retinopathy at a p value of 0.20 or less, we considered them for inclusion in the multivariable model. Using a forward, stepwise procedure, only potential confounders that changed the ORs ≥10 % were included in the adjusted model. The multivariable model was also adjusted for hypertension status and HBA1c (as a measure of blood glucose control) to examine whether these variables mediated the 25(OH)D and retinopathy association.
A sensitivity analysis was conducted restricting our sample to include only individuals defined as having diabetes at both visits 2 (when 25[OH]D was measured) and 3. We wanted to examine if the association between vitamin D status and retinopathy would change when the sample was limited to those who were diagnosed with diabetes when 25(OH)D measures were assessed. Effect modification of the vitamin D and retinopathy association by age, sex, race, duration of diabetes and blood glucose control was explored by adding an interaction term to our logistic regression models. A p value <0.10 for the interaction term was considered statistically significant.
Variation in 25(OH)D concentrations explained by dietary intake of vitamin D was estimated using linear regression with season-adjusted 25(OH)D concentrations as the dependent variable and dietary vitamin D intake as the independent variable. Adjusted ORs and 95 % CIs for retinopathy in quartiles 2 through 4 (with quartile 1 as the referent) for dietary vitamin D intake (IU/day) and by category of reported frequency of consumption of vitamin D rich foods (never consumers as the referent) were estimated. A p for trend using continuous vitamin D intake or frequency of consumption, respectively, was estimated. We also estimated the odds of retinopathy in those who reported using vitamin D or fish oil supplements.
Results
Seven percent of participants had deficient vitamin D status (25[OH]D < 30 nmol/L) and 59 and 16 % had adequate status with 25(OH)D concentrations ≥50 and ≥75 nmol/L, respectively (Table 1). Participants with adequate (≥75 nmol/L) compared to deficient vitamin D status were less likely to have retinopathy, be women, be from Jackson, MS, and have graduated high school, and they were more likely to be older and Caucasian. There was a greater proportion of former (compared to never or current) smokers with adequate versus deficient status. Individuals with adequate status had greater vitamin D intake, smaller waist circumferences, were less likely to be obese, and more likely to be physical active. On average their systolic blood pressure, HDL, glucose, and HBA1c were lower, and their hematocrit and triglycerides were higher. Those with adequate status were also less likely to have used insulin in the last 2 weeks.
Of the 1339 diabetic participants, 21 % (n = 280) had DR. In crude analyses, individuals with 25(OH)D concentrations 50 to <75 and ≥75 nmol/L had lower odds of retinopathy than deficient individuals (Table 2). Only adjustment for race and duration of diabetes changed the odds ratio greater than 10 % and were included in the multivariable model. Adjustment for age or BMI, a strong predictor of 25(OH)D concentrations, had no additional influence on the model and thus was not adjusted for in these analyses. After adjustment for these covariates there was a significant 61 % lower odds of retinopathy for those with 25(OH)D concentrations ≥75 nmol/L, with a significant p for trend of 0.001 and a 13 % lower odds of retinopathy with each additional 10 nmol/L in serum 25(OH)D concentrations. Further adjustment for HBA1c attenuated the association, but did not remove statistical significance. The odds of participants having proliferative diabetic retinopathy or macular edema among those with 25(OH)D ≥50 nmol/L (19 out of 789 at risk) compared to those with 25(OH)D <50 nmol/L (12 out of 550 at risk) was 1.48 (0.70–3.12) adjusted for race, duration, HBA1c and hypertension status. The adjusted odds ratio per 10 nmol/L difference in 25(OH)D was 1.07 (0.89–1.29), p for trend =0.473.
The observed lower odds of retinopathy among participants with adequate compared to deficient vitamin D status remained regardless of age, sex, race, duration of diabetes and glycemic control, except for observations in the youngest age group (54 years and younger) (Table 3). There were not statistically significant interactions. A sensitivity analysis removing participants who were not classified as having diabetes at visit 2 (n = 336), when 25(OH)D concentrations were measured, did not substantially change the main findings. The odds of retinopathy in participants with 25(OH)D ≥75 compared to <30 nmol/L was 0.43 (0.21–0.88), p for trend = 0.005 after adjustment for race and duration and 0.54 (0.25–1.15), p for trend = 0.055 with further adjustment for HBA1c and hypertension status.
Dietary vitamin D intake of vitamin D from foods accounted for 1 % of the between person variation in 25(OH)D concentrations in this sample. No statistically significant associations were found between vitamin D intake from foods and retinopathy (Additional file 1: Table S1). Intake of 1 serving (3–5 oz) of dark fish >1/week compared to never was associated with a 68 % lower odds of retinopathy with a p for continuous trend of 0.060. Further adjustment by intake of omega-3 polyunsaturated fatty acids (PUFAs) did not attenuate this association (data not shown). The odds of retinopathy among vitamin D and fish oil supplement users compared to nonusers was 0.63 (0.25–1.64) with adjustment for race, duration of diabetes, HBA1c, and hypertension status.
Discussion
We observed a dose–response association between 25(OH)D concentrations and diabetic retinopathy, suggesting that individuals with higher 25(OH)D concentrations have lower odds of prevalent retinopathy, primarily NPDR. No statistically significant association was observed between 25(OH)D and severe disease (PDR or macular edema) although the number of cases was small (n = 31). A protective association with intake of vitamin D from all foods combined was not observed. Assessment of dietary vitamin D intake, as measured, does not likely reflect or enhance vitamin D status as we found vitamin D intake only explained a minimal amount of the between person variation in 25(OH)D concentrations in this sample. We did observe that frequent consumption (>1 time per week) of dark fish compared to never eating this type of fish was associated with a decreased odds for retinopathy. Fish are a rich source of vitamin D as well as omega-3 PUFAs (eicosapentaenoic and docosahexaenoice acid). omega-3 have anti-inflammatory properties [45], but adjustment for intake of omega-3 PUFAs did not confound this association.
Previous research on the association between vitamin D status and diabetic retinopathy has predominantly focused on samples of individuals with type 2 diabetes [3–8, 11–17, 19, 21–23], similar to ARIC, with some research focused on individuals with type 1 diabetes [9, 10, 18, 20]. A number of studies have compared 25(OH)D concentrations between groups of individuals with and without diabetic retinopathy in case–control designs [3, 11, 13, 17, 22] with a protective association of 25(OH)D on prevalent retinopathy found in three studies [3, 11, 13]. The majority of other studies consist of cross-sectional designs recruiting participants from clinical settings [5, 6, 9, 10, 12, 14, 15, 19, 21, 23] with half of these studies supporting a protective association of vitamin D with retinopathy [5, 6, 9, 10, 12]. All noted studies recruited participants with diabetes from clinic settings, perhaps limiting the generalizability of study findings. Other limitations include small sample sizes (n ≤ 300 for samples of individuals with diabetes) [5, 10, 11, 13–15, 17, 23], lack of multivariate adjusted analysis [14, 17], inclusion of strong determinants of 25(OH)D concentrations in multivariable models which may result in overadjustment [20], and assessment of retinopathy status from ophthalmologist examination rather than from standardized grading of retinal fundus photographs [3, 5, 11–15, 17, 19, 21–23].
Results from nationally representative surveys [4, 6] comprised primarily of individuals with type 2 diabetes have supported a protective association between retinopathy status and 25(OH)D concentrations; however a population-based cohort [20] of individuals with type 1 diabetes has not. Strengths of these studies include the use of graded, retinal photographs, adjustment for other confounding factors, and large sample sizes (~500 + participants). These cross-sectional studies cannot establish temporality of the vitamin D and retinopathy association, similar to the present study.
Only three studies to date have examined prospective associations between vitamin D status and risk of retinopathy [8, 16, 18]. No statistically significant association was observed between 25(OH)D concentrations and the 26-year incidence of either background or proliferative retinopathy among 220 patients with type 1 diabetes attending a diabetes center [18] or with the 5-year incidence or progression of retinopathy in the Veterans Affairs Diabetes Trial (n = 955) [16]. A recent study of 9524 participants with type 2 diabetes from the Fenofibrate intervention and Event Lowering Diabetes (FIELD) Trial were followed for development microvascular complications, including retinopathy determined by on-study laser treatment (not fundus photography). [8] They observed a significant 13 % (p = 0.03) lower odds of microvascular complications with each baseline 50 nmol/L difference in 25(OH)D. Further adjustment of the multivariable model for HBA1c, physical activity or seasonal variability attenuated the association and removed its statistical significance. In our study, the association between vitamin D status and retinopathy was also attenuated after adjustment for glycemic control. It is unclear whether adjustment for HBA1c confounds the observed association or results in over adjustment because vitamin D protects against retinopathy via its influence on glycemic control.
Vitamin D is proposed to have a role in ocular health. Expression of the vitamin D receptor (VDR) in the retina [46] and in human cultured retinal endothelial cells [47], support this hypothesis. Further, the enzyme 1-α-hydroxylase, responsible for synthesis of 1,25(OH)2D, is expressed in the retina suggesting a local action of the hormone calcitriol (1,25(OH)2D) in the eye [46].
In vitro studies [48] and animal models of diabetes [49] suggest that chronic low grade inflammation plays a role in the development of diabetic retinopathy; however, evidence of associations between biomarkers of systemic inflammation and diabetic retinopathy in epidemiologic studies still remains inconclusive [50]. High blood glucose is thought to increase adhesion of leukocytes to microvascular endothelial cells leading to cell damage, impaired blood flow [49, 51], and consequential retinopathy lesions [52, 53]. We hypothesize that vitamin D may down-regulate a localized, ocular, pro-inflammatory state by suppressing pro-inflammatory cytokines and other toxic agents [24]. This is supported by a study in cultured endothelial cells showing that vitamin D reduces the damaging effects of advanced glycation end products [54].
The VDR is expressed in human pancreatic beta-cells [55] and the human insulin receptor gene’s promoter has a vitamin D response element [56], suggesting a possible role in blood glucose control. To date, in vitro cell culture and animal model studies of diabetes examining the effect of 1,25(OH)2D on beta cell function, insulin receptor gene expression, and glucose uptake are inconclusive [57]. A recent meta-analysis suggests no association between randomized controlled vitamin D supplementation trials and glucose homeostasis or diabetes prevention; however, this study could not make conclusions with respect to the effect of long-term supplementation and micro- or macro-vascular complications of diabetes [58].
Our study is limited by its cross-sectional design and therefore cannot determine the temporality of this association between vitamin D and retinopathy. We are also limited by the availability of retinal photographs taken of one field from only one eye. There may be misclassification of endpoints ascertained at visit 3. However, as the photographed eye was chosen randomly, we would expect nondifferential misclassification of our endpoint which would bias our observed risk estimates toward the null. We also could not adequately explore the association between vitamin D and proliferative retinopathy due to the small number of participants with this outcome. Vitamin D has been shown to inhibit angiogenesis in an animal model of oxygen-induced ischemic retinopathy [59] and inhibit vascular endothelial growth factor and transforming growth factor-β1 expression in retinal tissues of experimentally induced diabetes in rats [60]. We also did not have data on sunlight exposure, and thus were unable to examine the association between vitamin D and diabetic retinopathy inclusive of all relevant sources contributing to circulating 25(OH)D concentrations.
Our study’s strength include a well-defined population of individuals with diabetes and availability of numerous, measured covariates that we could adjust for as potential confounding factors, although we realize that residual confounding may exist. Our study was population-based and is most generalizable to individuals with type 2 diabetes who comprised the majority of our sample. We were able to examine this association in both Caucasians and African Americans, showing that associations did not vary by race. We had retinal photographs, graded in a standardized fashion, to assess retinopathy and 25(OH)D and assessed using LC–MS, the gold standard for vitamin D assessment [61], with standardized, quality control measures taken. Our study contributes to the body of evidence supporting a protective, association between 25(OH)D and prevalent diabetic retinopathy that is consistent across racial groups.
Conclusions
In conclusion, adequate vitamin D status, 25(OH)D concentrations ≥75 nmol/L, may be associated with reduced odds of diabetic retinopathy. We speculate that the influence of vitamin D on diabetic retinopathy may be, in part, via its influence on blood glucose control.
Abbreviations
- 25[OH]D:
-
25-hydroxy vitamin D
- ARIC:
-
atherosclerosis risk in communities study
- BMI:
-
body mass index
- DR:
-
diabetic retinopathy
- HBA1c :
-
glycosylated hemoglobin A1c
- HDL:
-
high density lipoprotein
- LDL:
-
low density lipoprotein
- NPDR:
-
non-proliferative diabetic retinopathy
- PDR:
-
proliferative diabetic retinopathy
- VDR:
-
vitamin D receptor
References
American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Pattern® Guidelines. Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2014. Available at: www.aao.org/ppp. Accessed 22 Aug 2016.
Mares JA, Millen AE, Meyers KJ. Diet and supplements in the prevention and treatment of eye diseases. In: Coulston AM, Boushey CJ, Ferruzzi MG, editors. Nutrition in the prevention and treatment of disease. Waltham: Elsevier Academic Press; 2013. p. 341–71.
Suzuki A, Kotake M, Ono Y, Kato T, Oda N, Hayakawa N, Hashimoto S, Itoh M. Hypovitaminosis D in type 2 diabetes mellitus: association with microvascular complications and type of treatment. Endocr J. 2006;53(4):503–10.
Patrick PA, Visintainer PF, Shi Q, Weiss IA, Brand DA. Vitamin D and retinopathy in adults with diabetes mellitus. Arch Ophthalmol. 2012;130(6):756–60. doi:10.1001/archophthalmol.2011.2749.
Ahmadieh H, Azar ST, Lakkis N, Arabi A. Hypovitaminosis d in patients with type 2 diabetes mellitus: a relation to disease control and complications. ISRN Endocrinol. 2013;2013:641098. doi:10.1155/2013/641098.
He R, Shen J, Liu F, Zeng H, Li L, Yu H, Lu H, Lu F, Wu Q, Jia W. Vitamin D deficiency increases the risk of retinopathy in Chinese patients with type 2 diabetes. Diabet Med. 2014;31(12):1657–64. doi:10.1111/dme.12581.
Jee D, Han K, Kim EC. Inverse association between high blood 25-hydroxyvitamin D levels and diabetic retinopathy in a representative Korean population. PLoS ONE. 2014;9(12):e115199. doi:10.1371/journal.pone.0115199.
Herrmann M, Sullivan DR, Veillard AS, McCorquodale T, Straub IR, Scott R, Laakso M, Topliss D, Jenkins AJ, Blankenberg S, et al. Serum 25-hydroxyvitamin D: a predictor of macrovascular and microvascular complications in patients with type 2 diabetes. Diabetes Care. 2015;38(3):521–8. doi:10.2337/dc14-0180.
Kaur H, Donaghue KC, Chan AK, Benitez-Aguirre P, Hing S, Lloyd M, Cusumano J, Pryke A, Craig ME. Vitamin D deficiency is associated with retinopathy in children and adolescents with type 1 diabetes. Diabetes Care. 2011;34(6):1400–2. doi:10.2337/dc11-0103.
Shimo N, Yasuda T, Kaneto H, Katakami N, Kuroda A, Sakamoto F, Takahara M, Irie Y, Horikawa K, Miyashita K, et al. Vitamin D deficiency is significantly associated with retinopathy in young Japanese type 1 diabetic patients. Diabetes Res Clin Pract. 2014;106(2):e41–3. doi:10.1016/j.diabres.2014.08.005.
Alcubierre N, Valls J, Rubinat E, Cao G, Esquerda A, Traveset A, Granado-Casas M, Jurjo C, Mauricio D. Vitamin D deficiency is associated with the presence and severity of diabetic retinopathy in type 2 diabetes mellitus. J Diabetes Res. 2015;2015:374178. doi:10.1155/2015/374178.
Zoppini G, Galletti A, Targher G, Brangani C, Pichiri I, Trombetta M, Negri C, De Santi F, Stoico V, Cacciatori V, et al. Lower levels of 25-hydroxyvitamin D3 are associated with a higher prevalence of microvascular complications in patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2015;3(1):e000058. doi:10.1136/bmjdrc-2014-000058.
Reddy GB, Sivaprasad M, Shalini T, Satyanarayana A, Seshacharyulu M, Balakrishna N, Viswanath K, Sahay M. Plasma vitamin D status in patients with type 2 diabetes with and without retinopathy. Nutrition. 2015;31(7–8):959–63. doi:10.1016/j.nut.2015.01.012.
Aksoy H, Akcay F, Kurtul N, Baykal O, Avci B. Serum 1,25 dihydroxy vitamin D (1,25(OH)2D3), 25 hydroxy vitamin D (25(OH)D) and parathormone levels in diabetic retinopathy. Clin Biochem. 2000;33(1):47–51.
Payne JF, Ray R, Watson DG, Delille C, Rimler E, Cleveland J, Lynn MJ, Tangpricha V, Srivastava SK. Vitamin D insufficiency in diabetic retinopathy. Endocr Pract. 2012;18(2):185–93. doi:10.4158/EP11147.OR.
Alele JD, Luttrell LM, Hollis BW, Luttrell DK, Hunt KJ, Group VS. Relationship between vitamin D status and incidence of vascular events in the Veterans Affairs Diabetes Trial. Atherosclerosis. 2013;228(2):502–7. doi:10.1016/j.atherosclerosis.2013.03.024.
Bajaj S, Singh RP, Dwivedi NC, Singh K, Gupta A, Mathur M. Vitamin D levels and microvascular complications in type 2 diabetes. Int J Endocrinol Metab. 2014;18(4):537–41. doi:10.4103/2230-8210.137512.
Joergensen C, Hovind P, Schmedes A, Parving HH, Rossing P. Vitamin d levels, microvascular complications, and mortality in type 1 diabetes. Diabetes Care. 2011;34(5):1081–5.
Bonakdaran S, Shoeibi N. Is there any correlation between vitamin D insufficiency and diabetic retinopathy? Int J Ophthalmol. 2015;8(2):326–31. doi:10.3980/j.issn.2222-3959.2015.02.20.
Engelen L, Schalkwijk CG, Eussen SJ, Scheijen JL, Soedamah-Muthu SS, Chaturvedi N, Fuller JH, Stehouwer CD. Low 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 levels are independently associated with macroalbuminuria, but not with retinopathy and macrovascular disease in type 1 diabetes: the EURODIAB prospective complications study. Cardiovasc Diabetol. 2015;14:67. doi:10.1186/s12933-015-0231-2.
Alam U, Amjad Y, Chan AW, Asghar O, Petropoulos IN, Malik RA. Vitamin D deficiency is not associated with diabetic retinopathy or maculopathy. J Diabetes Res. 2016;2016:6156217. doi:10.1155/2016/6156217.
Usluogullari CA, Balkan F, Caner S, Ucler R, Kaya C, Ersoy R, Cakir B. The relationship between microvascular complications and vitamin D deficiency in type 2 diabetes mellitus. BMC Endocr Disord. 2015;15:33. doi:10.1186/s12902-015-0029-y.
Jung CH, Kim KJ, Kim BY, Kim CH, Kang SK, Mok JO. Relationship between vitamin D status and vascular complications in patients with type 2 diabetes mellitus. Nutr Res. 2016;36(2):117–24. doi:10.1016/j.nutres.2015.11.008.
Mora JR, Iwata M, von Andrian UH. Vitamin effects on the immune system: vitamins A and D take centre stage. Nat Rev Immunol. 2008;8(9):685–98. doi:10.1038/nri2378.
Kern TS. Contributions of inflammatory processes to the development of the early stages of diabetic retinopathy. Exp Diabetes Res. 2007;2007:95103.
Feneis JF, Arora RR. Role of vitamin D in blood pressure homeostasis. Am J Ther. 2010;17(6):e221–9. doi:10.1097/MJT.0b013e3181d16999.
Mitri J, Pittas AG. Vitamin D and diabetes. Endocrinol Metab Clin North Am. 2014;43(1):205–32. doi:10.1016/j.ecl.2013.09.010.
Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus: UKPDS 69. Arch Ophthalmol. 2004;122(11):1631–40.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
The Atherosclerosis Risk in Communities. (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687–702.
Klein R, Clegg L, Cooper LS, Hubbard LD, Klein BE, King WN, Folsom AR. Prevalence of age-related maculopathy in the atherosclerosis risk in communities study. Arch Ophthalmol. 1999;117(9):1203–10.
Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98(5):786–806.
Folsom AR, Roetker NS, Rosamond WD, Heckbert SR, Basu S, Cushman M, Lutsey PL. Serum 25-hydroxyvitamin D and risk of venous thromboembolism: the atherosclerosis risk in communities (ARIC) study. J Thromb Haemost. 2014;12(9):1455–60. doi:10.1111/jth.12665.
SAS Institute Inc. SAS/STAT® 9.2 User’s Guide. The LOESS Procedure (Book Excerpt). Cary, NC: SAS Institute Inc. 2008. http://support.sas.com/documentation/cdl/en/statugloess/61801/PDF/default/statugloess.pdf. Accessed 7 Jan 2015.
Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65.
Stevens J, Metcalf P, Dennis B, Tell G, Shimakawa T, Folsom AR. Reliability of a food frequency questionnaire by ethnicity, gender, age and education. Nutrition Res. 1996;16(5):735–45.
Atherosclerosis Risk in Communities (ARIC) Study Research Group. Manual 7 Blood Collection. Chapell Hill, NC: Atherosclerosis Risk in Communities (ARIC) Study Research Group; 1990.
Selvin E, Steffes MW, Gregg E, Brancati FL, Coresh J. Performance of A1C for the classification and prediction of diabetes. Diabetes Care. 2011;34(1):84–9. doi:10.2337/dc10-1235.
Atherosclerosis Risk in Communities (ARIC) Study Research Group. Manual 8 Lipid and Lipoprotein Determinations. Chapell Hill, NC: Atherosclerosis Risk in Communities (ARIC) Study Research Group; 1991.
Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutrition. 1982;36(5):936–42.
Pols MA, Peeters PH, Bueno-De-Mesquita HB, Ocke MC, Wentink CA, Kemper HC, Collette HJ. Validity and repeatability of a modified Baecke questionnaire on physical activity. Int J Epidemiol. 1995;24(2):381–8.
Richardson MT, Ainsworth BE, Wu HC, Jacobs DR Jr, Leon AS. Ability of the atherosclerosis risk in communities (ARIC)/Baecke questionnaire to assess leisure-time physical activity. Int J Epidemiol. 1995;24(4):685–93.
IOM (Institute of Medicine). Summary. In: Dietary Reference Intakes for Calcium and Vitamin D. Washington DC: The National Academy Press; 2011. p. 1–14.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21(16):2409–19. doi:10.1002/sim.1047.
Chapkin RS, Kim W, Lupton JR, McMurray DN. Dietary docosahexaenoic and eicosapentaenoic acid: emerging mediators of inflammation. Prostaglandins Leukot Essent Fatty Acids. 2009;81(2–3):187–91. doi:10.1016/j.plefa.2009.05.010.
Alsalem JA, Patel D, Susarla R, Coca-Prados M, Bland R, Walker EA, Rauz S, Wallace GR. Characterization of vitamin D production by human ocular barrier cells. Invest Ophthalmol Vis Sci. 2014;55(4):2140–7. doi:10.1167/iovs.13-13019.
Choi D, Appukuttan B, Binek SJ, Planck SR, Stout JT, Rosenbaum JT, Smith JR. Prediction of Cis-Regulatory Elements Controlling Genes Differentially Expressed by Retinal and Choroidal Vascular Endothelial Cells. J Ocul Biol Dis Infor. 2008;1(1):37–45.
Moore TC, Moore JE, Kaji Y, Frizzell N, Usui T, Poulaki V, Campbell IL, Stitt AW, Gardiner TA, Archer DB, et al. The role of advanced glycation end products in retinal microvascular leukostasis. Invest Ophthalmol Vis Sci. 2003;44(10):4457–64.
Schroder S, Palinski W, Schmid-Schonbein GW. Activated monocytes and granulocytes, capillary nonperfusion, and neovascularization in diabetic retinopathy. Am J Pathol. 1991;139(1):81–100.
Rajab HA, Baker NL, Hunt KJ, Klein R, Cleary PA, Lachin J, Virella G, Lopes-Virella MF. Investigators DEGo. The predictive role of markers of Inflammation and endothelial dysfunction on the course of diabetic retinopathy in type 1 diabetes. J Diabetes Complications. 2015;29(1):108–14. doi:10.1016/j.jdiacomp.2014.08.004.
Chibber R, Ben-Mahmud BM, Chibber S, Kohner EM. Leukocytes in diabetic retinopathy. Curr Diabetes Rev. 2007;3(1):3–14.
Stitt AW. AGEs and diabetic retinopathy. Invest Ophthalmol Vis Sci. 2011;51(10):4867–74.
Yamagishi S, Ueda S, Matsui T, Nakamura K, Okuda S. Role of advanced glycation end products (AGEs) and oxidative stress in diabetic retinopathy. Curr Pharm Des. 2008;14(10):962–8.
Talmor Y, Golan E, Benchetrit S, Bernheim J, Klein O, Green J, Rashid G. Calcitriol blunts the deleterious impact of advanced glycation end products on endothelial cells. Am J Physiol. 2008;294(5):F1059–64.
Johnson JA, Grande JP, Roche PC, Kumar R. Immunohistochemical localization of the 1,25(OH)2D3 receptor and calbindin D28 k in human and rat pancreas. Am J Physiol. 1994;267(3 Pt 1):E356–60.
Maestro B, Davila N, Carranza MC, Calle C. Identification of a Vitamin D response element in the human insulin receptor gene promoter. J Steroid Biochem Mol Biol. 2003;84(2–3):223–30.
Mathieu C. Vitamin D and diabetes: where do we stand? Diabetes Res Clin Pract. 2015;108(2):201–9. doi:10.1016/j.diabres.2015.01.036.
Seida JC, Mitri J, Colmers IN, Majumdar SR, Davidson MB, Edwards AL, Hanley DA, Pittas AG, Tjosvold L, Johnson JA. Clinical review: effect of vitamin D3 supplementation on improving glucose homeostasis and preventing diabetes: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2014;99(10):3551–60. doi:10.1210/jc.2014-2136.
Albert DM, Scheef EA, Wang S, Mehraein F, Darjatmoko SR, Sorenson CM, Sheibani N. Calcitriol is a potent inhibitor of retinal neovascularization. Invest Ophthalmol Vis Sci. 2007;48(5):2327–34.
Ren Z, Li W, Zhao Q, Ma L, Zhu J. The impact of 1,25-dihydroxy vitamin D3 on the expressions of vascular endothelial growth factor and transforming growth factor-beta(1) in the retinas of rats with diabetes. Diabetes Res Clin Pract. 2012;98(3):474–80. doi:10.1016/j.diabres.2012.09.028.
Ziegler TE, Kapoor A, Hedman CJ, Binkley N, Kemnitz JW. Measurement of 25-hydroxyvitamin D(2&3) and 1,25-dihydroxyvitamin D(2&3) by tandem mass spectrometry: a primate multispecies comparison. Am J Primatol. 2015;77(7):801–10. doi:10.1002/ajp.22403.
Authors’ contributions
AEM had full access to all of the data in the study and takes primary responsibility for the final content of this manuscript. Contribution of authors: AEM, MJL, PLL, JAM, BEKK, KJM, CAA, RK designed the research study. AEM directed analyses with MWS and JN conducting the analyses and aiding in data interpretation. AEM and MWS wrote the primary manuscript, with all co-authors aiding in the interpretation of the data analysis and drafting of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to acknowledge Elizabeth Selvin, PhD at Johns Hopkins Bloomberg School of Public Health for providing data on HbA1c.
Competing interests
Kristin Meyers’ affiliation was with the University of Wisconsin during her efforts on this manuscript. As of February 2015, she has been an employee of Eli Lilly and Company and her efforts on this manuscript have been limited to critical review. Other co-authors had not conflicts of interest to disclose.
Availability of data and material
The ARIC Study website for “ARIC investigators, researchers, participants, and the scientific community” is found at https://www2.cscc.unc.edu/aric/desc (Accessed July 19, 2016). This site contains information on how to propose to use the existing data in a manuscript or ancillary study.
Consent for publication
Participants provided consent for research and publication of aggregate data.
Ethics approval and consent to participate
All participants provided signed informed consent and the study protocol was approved by the institutional review boards at each ARIC study site and complies with the Helsinki Declaration as revised in 1983.
Funding
This research is supported by the NIH National Institute on Aging Grant number R01 AG041776, NIH National Heart, Lung, and Blood Institute Grant number R01 HL103706, and the NIH Office of Dietary Supplements Grant number R01 HL103706-S1. The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). The authors thank the staff and participants of the ARIC study for their important contributions.
Reference to prior publication of the study in abstract form
This work was previously presented as a poster at the 74th American Diabetes Association Conference in 2013, San Francisco, CA, June 13–17, 2014.
Author information
Authors and Affiliations
Corresponding author
Additional file
12933_2016_434_MOESM1_ESM.doc
Additional file 1: Table S1. Adjusted* ORs and 95 % CI for diabetic retinopathy by reported quartile (Q) of dietary vitamin D intake from foods (IU/day) and by frequency of consumption of vitamin D rich foods at visit 1 (1987–1989) among Caucasian and African American ARIC study participants classified as having diabetes and having gradable eye photos at visit 3 (1993–95) and dietary data at visit 1 (N = 1305†).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Millen, A.E., Sahli, M.W., Nie, J. et al. Adequate vitamin D status is associated with the reduced odds of prevalent diabetic retinopathy in African Americans and Caucasians. Cardiovasc Diabetol 15, 128 (2016). https://doi.org/10.1186/s12933-016-0434-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-016-0434-1