Abstract
Background
Establishing whether there is a potential relationship between glucagon-like peptide 1 receptor agonists (GLP-1RAs) and suicidal or self-injurious behaviors (SSIBs) is crucial for public safety. This study investigated the potential association between GLP-1RAs and SSIBs by exploring the FDA Adverse Event Reporting System (FAERS) database.
Methods
A disproportionality analysis was conducted using post-marketing data from the FAERS repository (2018 Q1 to 2022 Q4). SSIB cases associated with GLP-1RAs were identified and analyzed through disproportionality analysis using the information component. The parametric distribution with a goodness-of-fit test was employed to analyze the time-to-onset, and the Ω shrinkage was used to evaluate the potential effect of co-medication on the occurrence of SSIBs.
Results
In total, 204 cases of SSIBs associated with GLP-1RAs, including semaglutide, liraglutide, dulaglutide, exenatide, and albiglutide, were identified in the FAERS database. Time-of-onset analysis revealed no consistent mechanism for the latency of SSIBs in patients receiving GLP-1RAs. The disproportionality analysis did not indicate an association between GLP-1RAs and SSIBs. Co-medication analysis revealed 81 cases with antidepressants, antipsychotics, and benzodiazepines, which may be proxies of mental health comorbidities.
Conclusions
We found no signal of disproportionate reporting of an association between GLP-1RA use and SSIBs. Clinicians need to maintain heightened vigilance on patients premedicated with neuropsychotropic drugs. This contributes to the greater acceptance of GLP-1RAs in patients with type 2 diabetes mellitus or obesity.
Graphical Abstract

Highlights
• To determine whether there is a potential relationship between glucagon-like peptide 1 receptor agonists (GLP-1RAs) and suicidal or self-injurious behaviors (SSIBs).
• Is there a direct association between GLP-1RAs and SSIBs? No evidence reasonably suggests an association between GLP-1RAs and SSIBs based on clinical characteristics, time-onset, disproportionality, and co-medication analysis.
• Clinicians should pay more attention to the psychiatric status of patients with a history of neuropsychotropic drugs, and more comprehensive monitoring is needed to consider their susceptibility to SSIBs carefully.
Similar content being viewed by others
Background
Glucagon-like peptide 1 receptor agonists (GLP-1RAs) are modified derivatives of glucagon-like peptide 1 (GLP-1) that simulate the regulatory effect of GLP-1 on blood glucose levels. The primary advantages of GLP-1RAs lie in glucose reduction, cardiorenal benefits, and amelioration of metabolic syndrome, all of which are substantiated by a plethora of evidence-based studies [1,2,3,4]. Therefore, GLP-1RAs have emerged as one of the recommended pharmacological interventions for type 2 diabetes mellitus, especially for patients with cardiovascular risk factors and coexisting comorbidities (e.g., chronic kidney disease) [5]. Furthermore, GLP-1RAs exhibit substantial weight reduction effects by facilitating glucose uptake and suppressing appetite [6]. According to the Centers for Disease Control and Prevention, diabetes and obesity rank among the top 10 most economically burdensome chronic diseases in the USA. Given the escalating global prevalence of these diseases, there is an unprecedented opportunity to expand the global market for GLP-1RAs.
Since the approval of exenatide for the treatment of type 2 diabetes by the Food and Drug Administration (FDA) in 2005, research on GLP-1 RAs has become a hot topic and new analogs are constantly being introduced to the market. In December 2014, the FDA approved liraglutide as a weight loss drug. Right after this, semaglutide became available with the indication of diabetes in 2017, and then in 2020, its treatment for obesity was also authorized. Global demand for semaglutide and liraglutide exceeds the present supply, which might be related to their off label uses and misuse [7]. Despite the significant potential and advantages of GLP-1RAs, they are inevitably accompanied by a range of possible adverse drug reactions (ADRs), as is the case with any medication. The most prevalent ADRs associated with GLP-1RA therapy encompass gastrointestinal events such as nausea, vomiting, and diarrhea. However, these non-serious ADRs are tolerable in individuals with diabetes and obesity [8,9,10]. What raises concerns are some of the recent reports of serious ADRs associated with GLP-1RAs: (i) Pfizer’s disclosure of elevated aminotransferases in users of lotiglipron (a novel oral GLP-1RA) is indicative of hepatocellular injury [11]; (ii) Studies revealed an elevated risk of thyroid cancer associated and cholecystitis with the use of GLP-1RAs [12, 13]; (iii) The Icelandic Medicines Agency has submitted 150 reports of GLP-1RAs-related suicidal or self-injurious behaviors (SSIBs) to the European Medicines Agency (EMA) [14]. Following the aforementioned incidents, the development of lotiglipron was discontinued, and drug regulatory agencies in several countries classified GLP-1RAs as a potential risk factor for thyroid cancer, gallbladder, and biliary diseases. However, no studies have investigated the association between GLP-1RAs and SSIBs. SSIBs, recognized as significant ADRs, have garnered widespread acknowledgment as critical factors that may jeopardize patient safety [15]. Studies have demonstrated a consistent year-on-year escalation in patient suicides associated with medication use, intensifying concerns among the general public and clinical professionals regarding this phenomenon [16,17,18]. Therefore, in the context of the widespread global utilization of GLP-1RAs, it is imperative to investigate whether a potential relationship exists between GLP-1RAs and SSIBs, which is of paramount importance for public and clinical medication safety.
The FDA Adverse Event Reporting System (FAERS) is a comprehensive database of ADRs specifically designed by the FDA to facilitate postmarketing surveillance of drugs and therapeutic biologics [19]. The database includes all ADRs and medication errors documented by the FDA. It facilitates the identification and quantitative analysis of signals indicating disproportionate reporting of ADRs, thereby aiding in the recognition of associations between specific drugs and particular ADRs [20, 21].
This study aimed to explore the morbidity characteristics of SSIBs associated with GLP-1RAs by mining the FAERS database and measuring the association between GLP-1RAs and SSIBs through metrics such as time of onset, disproportionality analysis, and co-medication analysis. The results of this study will have a positive impact on medication safety for patients with type 2 diabetes or obesity, which offering substantial backing for clinical medication choices.
Methods
Data sources and study design
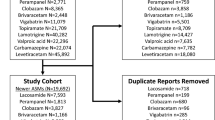
The FAERS, one of the largest publicly accessible databases for ADRs, provides researchers with raw data from the FDA website (https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html). To process the extracted raw data from the FAERS database, we utilized Microsoft SQL Server (version 2019; Microsoft Corporation, Redmond, WA, USA). Considering duplicate or implausible reports can lead to significant errors [22], extensive cleaning, and normalization were conducted to ensure interpretable data (detailed process is provided in Additional file 1: Fig S1[23,24,25]).
The study year was selected on the basis of drug and data availability. At the commencement of this study, the FDA only published data for the first quarter of 2023. Tirzepatide (marketed in September 2022) was excluded due to insufficient data, and semaglutide was the latest drug of interest to be marketed (December 2017). Therefore, we performed a disproportionality analysis of postmarketing data from the FAERS repository to investigate the potential association of SSIBs with GLP-1RAs. Data were selected for each complete year since the latest drug was marketed from 2018 quarter 1 to 2022 quarter 4. Ethical approval was not required as the study was conducted using de-identified publicly available data.
Definition of cases and drugs of interest
In the FAERS database, ADRs are classified according to the Medical Dictionary for Regulatory Activities (MedDRA) terminology in terms of signs and symptoms, which are called preferred terms (PTs). The ADRs of interest include suicidal ideation, self-injurious ideation, suicidal behaviors, and self-injurious behaviors (see Additional file 1: Table S1 for a detailed list), which are homogenously attributed to a high-level group term (HLGT) named suicidal and self-injurious behavior by MedDRA (version 26.0). The drugs of interest included FDA-approved GLP-1RAs [26]: semaglutide, liraglutide, dulaglutide, exenatide, lixisenatide, and albiglutide. In this study, venlafaxine was used as a positive control because it is significantly associated with SSIBs [27]. Orlistat and empagliflozin were selected as negative controls based on their similarity in the population indicated for GLP-1RAs, without any reported evidence of self-harm or suicide potential in the specification or related studies. The current study encompassed all cases in which GLP-1RAs were administered and listed as primary suspect drugs, secondary suspect drugs, or concomitant drugs for SSIBs.
Descriptive analysis
Patient demographics (age, sex, and reporter type) and clinical aspects (latency, outcome, and indication) were documented in reports of SSIBs with semaglutide, liraglutide, dulaglutide, exenatide, lixisenatide, and albiglutide.
Reported timeto-onset analysis
To describe the latency of SSIBs with GLP-1RAs, we performed a time-to-onset (TTO) analysis by selecting the parametric distribution model that demonstrated the best result in the goodness-of-fit test among the Weibull, log-normal, gamma, and exponential distributions. The parametric distribution is characterized by the scale parameter α and shape parameter β [28]. The scale parameter α represents the magnitude of ADRs occurring at the 63.2% quantile within the distribution function. Depending on the value of the shape parameter β, the upper limit of the 95% confidence interval (CI) for β < 1 indicates an initial increase, followed by a decrease in the hazard rate (early-failure type). Conversely, the lower limit of the 95% CI for β > 1 demonstrates an increasing hazard over time (wear-out failure type), whereas the 95% CI includes 1 for β, suggesting a constant hazard rate throughout the exposure period (random failure type). More details about TTO analysis and classification of β can be found in the Additional file 1, sections 4–5.
Disproportionality analysis
A sequential approach was adopted to systematically address major confounders:
-
(1)
An exploratory disproportionality approach comparing GLP-1RAs with all other drugs reported in the FAERS database, using venlafaxine as the positive control and empagliflozin/orlistat as the negative control. The definition of the disproportionality approach can be found in Additional file 1: section 4 [29].
-
(2)
We utilized the Bayesian Information Component (IC) to calculate the lower limit of the 95% CI (IC025). This approach is more precise than relying on the report odds ratio, particularly in situations with limited cases [30]. The IC calculation procedure can be found in Additional file 1: section 5.
-
(3)
False-negative analysis was conducted by artificially augmenting the reported incidence of GLP-1RA-associated SSIBs by 100%, aiming to ascertain whether the absence of positive findings could be attributed to our exclusion of some cases involving the concurrent use of multiple GLP-1RAs. This meticulous examination effectively substantiates the credibility of the negative results.
-
(4)
Given the inherent heterogeneity and potential reporting bias in the FAERS database, we conducted a series of sensitivity analyses. First, we excluded case and non-case reports with gastrointestinal events (all PTs belonged to gastrointestinal disorders in the system organ class) in the dataset. This step aimed to reduce the masking effect of gastrointestinal events to avoid possible competitive bias. Furthermore, the main indications in the included cases were type 2 diabetes mellitus and obesity, which are potential risk factors for SSIBs. Therefore, we narrowed the analysis dataset to subject with type 2 diabetes mellitus or weight loss through the indi_pt field (which represents the indication). Previous studies have shown that restricting the analyzed population can mitigate indication bias [21]. IC025 was calculated using the processed dataset to conduct the above sensitivity analyses.
-
(5)
Considering a low number of expected cases could lead to an insufficient sensitivity to detect disproportionality of relevant strength [31], we reported the sensitivity of a representative IC025 to measure the reliability of negative results. The result was deemed confident when the sensitivity to detect representative IC025>0.8. The calculation procedure can be found in Additional file 1: Fig S2.
Co-medication analysis
A case-by-case analysis was performed by two independent pharmacists to identify the combined medications by searching DRUG and THER files of the included 204 cases. When discrepancies existed, a third pharmacist was introduced to make the final decision. We conducted a co-medication analysis of GLP-1RAs and the top 20 most frequently used drugs in cases of SSIBs associated with GLP-1RAs. Calculation of IC025 for these drugs is consistent with the procedure described in section 2.5. We used the Ω shrinkage to measure drug–drug interactions because a previous study showed that it is the most conservative method among multiple algorithms [32]. The detection criterion is the lower limit of the 95% CI of the Ω (Ω025) > 0. The calculation process of Ω and the list of drugs were described in Additional file 1: Table S2. When at least one neuropsychiatric drug (such as antipsychotics, antidepressants, and anxiolytics) was recorded in the report, the patient was defined to have a medication history.
Global assessment of the evidence
The Modified Bradford Hill Criteria was used to assess the potential relationships among various available evidence [33,34,35]. The biological plausibility can assess whether there is a mechanism to support the potential relationship between ADRs and the studied drug. We also considered the strength of the evidence (the magnitude of observed effects) and the consistency of findings across various studies or sources. Additionally, specificity was utilized to assess whether some events were associated with specific factors, and coherence was to examine the temporal sequence of events that aligned with a potential relationship. Lastly, other similar drugs (empagliflozin and Orlistat) were used as a negative control to support the final conclusion.
Statistical analysis
The disproportionality threshold of the reporting signal was defined as IC025 > 0, and a positive drug-drug interaction was defined as Ω025 > 0. R (version 4.3.1; R Foundation for Statistical Computing, Vienna, Austria) was used for plotting, TTO analysis, and calculation of IC and Ω. The magnified percentage used in the false-negative analysis was 100%, determined based on a step-by-step strategy (Additional file 1: Fig S3, and Table S3).
Results
Descriptive analysis
From 2018 quarter 1 to 2022 quarter 4 of 2018, 57, 74, 51, 20, and 2 reports of SSIBs associated with semaglutide, liraglutide, dulaglutide, exenatide, and albiglutide, respectively, were identified in the FAERS database. Three patients were excluded because of the concomitant use of multiple GLP-1RAs, and no SSIB reports for lixisenatide were detected. The distribution of the reported years exhibited a generally even pattern, with a noticeable upward trend observed in 2022. The majority (54.90%) of the reports on SSIBs utilizing GLP-1RAs were contributed by healthcare professionals. Despite the small amount of missing or unknown data (2.94%), the proportion of reports in females was significantly higher than that in males (64.22 vs. 32.84%, respectively). Among the reports with available data, half of the cases were observed in adults (18–65 years). Type 2 diabetes (34.80%) and weight loss (14.71%) emerged as the most predominant indications, while others accounted for 3.92%, and unknown or missing constituted 46.57% (Table 1).
Reported time-to-onset analysis
A total valid case of 52 was used for TTO analysis (Fig. 1). Among them, three cases reported SSIBs on 1 day, 1 day, and 3 days after the cessation of GLP-1RAs (1 case for liraglutide and 2 cases for semaglutide), which might be related to the delayed ADR caused by the interested drugs.
TTO analysis of SSIBs reported for each GLP-1 RA. Reported TTO analysis and duration of treatment of SSIB associated with a liraglutide, b semaglutide, c dulaglutide, and d exenatide. Black diamonds represent the TTO of SSIBs following the administration of GLP-1RAs, while gray bars indicate the duration of GLP-1 treatment for each case. Due to limitations in data availability, the duration of therapy could only be plotted for a subset of the cases. Goodness-of-fit test of SSIB associated with e liraglutide, f semaglutide, g dulaglutide, and h exenatide. Positioned above the plot is the quantile boxplot. The green bars correspond to the case number of occurrences within the distribution, while the green line represents the fitted curve for the model exhibiting the most optimal outcomes. we adopted log-normal distribution to describe the latency of liraglutide and exenatide, gamma distribution for semaglutide, and Weibull distribution for dulaglutide. The raw data of TTO analysis in the 52 valid cases can be found in Additional file 1: Table S7. TTO, time-to-onset; SSIBs, Suicidal and Self-Injurious Behaviors; GLP-1 RA, GLP-1 receptor agonist
In analysis of TTO based on parameter distributions and the valid cases, the median TTOs (Interquartile range) for SSIBs associated with semaglutide, liraglutide, dulaglutide, and exenatide were 15.5 (0.5–24.25, n = 18), 9.5 (0.5–61.5, n = 19), 35.5 (6.5–60.5, n = 11), and 2.5 (1.5–169.5, n = 4) days, respectively (albiglutide was not included in the TTO analysis due to insufficient data). The results of goodness-of-fit performance test (Additional file 1: Table S4) indicated that a log-normal model was the best one to describe the latency of liraglutide- and exenatide-related SSIBs. A Gamma model was suitable for semaglutide-related SSIBs, and a Weibull model described the latency of dulaglutide-related SSIBs well. Semaglutide and dulaglutide were classified as early failure types, exenatide as a random failure type, and liraglutide as a wear-out failure type (Additional file 1: Table S5 for raw data).
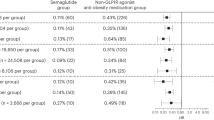
Disproportionality analysis
First, primary analysis was conducted to compare GLP-1RAs with other drugs in the FAERS database. The evaluated GLP-1RAs were semaglutide (IC025 = − 2.13), liraglutide (IC025 = − 1.18), dulaglutide (IC025 = − 3.76), exenatide (IC025 = − 3.52), and albiglutide (IC025 = − 3.91), none of which exhibited a signal of disproportionate reporting. Negative (empagliflozin, IC025 = − 1.66; orlistat, IC025 = − 4.91) and positive (venlafaxine, IC025 = 2.89) controls confirmed the internal validity of the database. We then performed a false-negative analysis in which the results of the disproportionate analysis of all GLP-1 drugs with SSIBs did not satisfy IC025 > 0 after expanding the number of reports by 100%, and the negative and positive control results remained valid (Fig. 2). Finally, IC025 < 0 was also observed in the sensitivity analyses (Fig. 3). The sensitivity to detect this IC025 was > 0.8 for all GLP-1 RAs in primary and false-negative analyses. In some subgroup analyses, there are some sensitivities to detect this IC025 was < 0.8 for albiglutide and exenatide. The raw data for the above analysis can be found in the Additional file 1: Table S8.
IC025 of SSIBs associated with GLP-1 RA in the primary analysis and false negative analysis. When IC025 > 0, a disproportionate reporting signal was detected. FAERS, US Food and Drug Administration Adverse Event Reporting System; IC, information component; SSIBs, Suicidal and Self-Injurious Behaviors; GLP-1 RA, GLP-1 receptor agonist
IC025 of SSIBs associated with GLP-1 RA in the sensitivity analysis. When IC025 >0, a disproportionate reporting signal was detected. FAERS, US Food and Drug Administration Adverse Event Reporting System; IC, information component; SSIBs, Suicidal and Self-Injurious Behaviors; GLP-1 RA, GLP-1 receptor agonist
Co-medication analysis
We conducted a co-medication analysis of the top 20 medications with the highest reported frequency of use for all GLP-1RA-associated SSIBs (considering the same reported cases, 23 medications were included). Multiple neuropsychiatric drugs, including bupropion, quetiapine, and aripiprazole, were identified, and disproportionality analysis with SSIBs yielded a reporting signal. Further examination revealed that 81 patients had a history of neuropsychiatric drugs, and 63 patients used more than one neuropsychiatric drug (Additional file 1: Fig S4). Subsequent Ω shrinkage results indicated no potential for drug–drug interactions between all GLP-1RAs and neuropsychiatric drugs (all Ω025 < 0; refer to Additional file 1: Table S6 for the list of top 20 medications’ IC025, and Ω025).
Causal relationship global assessment
Globally, the Bradford Hill Criteria were not fulfilled, as indicated by the strength of the disproportionality and its consistency throughout the analysis, temporal relationships, and biological plausibility, thus unsupporting a likely causal association between GLP-1RAs (semaglutide, liraglutide, dulaglutide, exenatide, lixisenatide, and albiglutide) and SSIBs (Table 2).
Discussion
The current study conducted a comprehensive analysis comprising four key objectives: first, we characterized the clinical features of SSIB cases related to GLP-1RA by analyzing postmarketing data from the FAERS database; second, we developed a latency model for these cases; third, we concluded the lack of disproportional reporting signals regarding GLP-1RAs and SSIBs; finally, we examined co-administration patterns of GLP-1RAs and potential drug–drug interactions with other medications to explore their impact on the reporting frequency of SSIBs.
Initially, we compared the clinical characteristics of patients treated with GLP-1RAs and SSIBs. Reports from 2018 to 2021 exhibited an overall average distribution. However, an uptrend in both ADR with case and non-case was observed in 2022, possibly reflecting the increased prescription of GLP-1RAs in recent years. Among the available data on adverse events, a significantly higher proportion of females (64.22%) than males (32.84%) reported SSIBs. Adults constituted the primary reporting population, accounting for the majority of all reports (juvenile: 1.47%, adults: 50.00%, and the elderly: 9.80%). The aforementioned sex disparities are also evident in epidemiological investigations of suicide attempts and suicidal ideation, which have demonstrated a higher prevalence of self-harming behaviors among females than among males. Notably, this disparity is particularly pronounced in obese individuals [40, 41]. With regard to age, physicians should exert heightened caution when considering the use of such medications in pediatric and geriatric populations, given their safety profiles [42]. Previous studies have also indicated that adults may exhibit a higher susceptibility to suicidal and self-harming tendencies than other age groups [43], potentially contributing to a higher number of reported cases among adults. Furthermore, between 2018 and 2022, 91,431 cases involving GLP-1RAs were reported, with the proportions of females, males, and unknown being 53.77, 38.79, and 7.44%, respectively. The proportion of children, adults, elderly individuals, and those of unknown age were 0.20, 27.02, 19.29, and 53.48%, respectively. We believe that the higher reporting by females and adults may also be related to the distribution of reports. By analyzing these data patterns and trends, we gained preliminary insights into the potential association between GLP-1RAs and SSIBs.
Next, we delved into the potential association between GLP-1RAs and TTO of SSIBs. Our analysis aimed to determine whether these drugs might influence the development of SSIBs by some common mechanism. GLP-1RAs are a class of drugs used to treat type 2 diabetes that can simulate the regulatory effect of GLP-1 on blood glucose levels. Although these GLP-1RAs differ in molecular structure and duration of action, their pharmacological mechanisms are similar [44, 45]. Therefore, we hypothesized that if GLP-1RAs had potential mechanistic associations with SSIBs, their pathogenic patterns would be similar. However, our results revealed unexpected findings. We observed three different pathogenic models for the drugs in the TTO analysis. For example, semaglutide and dulaglutide were categorized as early-failure types, exenatide was determined to be a random failure type, and liraglutide was classified as a wear-out failure type. This suggests that no single mechanism (tolerance effect/accumulation effect) explains the temporal association of onset between GLP-1RAs and SSIBs. Thus, the diversity of the onset patterns observed for GLP-1RAs appears to challenge the above assumptions, making it difficult to conclude a clear relationship between them.
We then performed an exploratory analysis of GLP-1RAs against all other drugs in the FAERS database using the same methodology used in previous pharmacovigilance studies [20, 36, 47, 48]. These studies provide a comprehensive and accurate biological perspective for a deeper understanding of the association between GLP-1RAs and SSIBs. Our view is beginning to lean toward the idea that the occurrence of SSIBs is more likely to be related to the mental state of the patient rather than GLP-1RAs.
Based on the above results and assessment of available research information, we adopted the adjusted Bradford Hill Criteria from previous publications and assessed the point-by-point link between GLP-1RAs and SSIBs. In general, the current evidence does not fully meet the adjusted Bradford Hill Criteria. Studies have reported liraglutide-associated suicide and semaglutide-associated depression in the coherence criterion [37,38,39]. However, the researchers concluded that liraglutide was not associated with the occurrence of SSIBs. In the randomized controlled trial (RCT) by Kelly et al. [37], a suicide case in the liraglutide group was reported to have a history of attention deficit hyperactivity disorder, which is a potential factor of SSIBs. Meanwhile, one adolescent attempted suicide in each group (the placebo group and the liraglutide group), highlighting that adolescents are a vulnerable population that should be monitored carefully. In another report of semaglutide-associated depression [39], the individual had a long history of depression, making it challenging to rule out the interference of disease recurrence. Furthermore, in the program of Semaglutide Treatment Effect in People with Obesity [49,50,51,52], no SSIBs were reported except for some mild or moderate psychiatric disorders(e.g., insomnia, anxiety) were observed. Through a comprehensive retrospective analysis of the strength of the association, analogy, and consistency metrics of GLP-1RAs and SSIBs, we concluded that there was no evidence reasonably suggesting an association between GLP-1RAs and SSIBs. However, the RCT studies, case reports, and the FAERS database case all highlighted that we should be aware of co-administered neuropsychotropic drugs that may associated with SSIBs. Clinicians should recognize that patients undergoing polypharmacy require heightened vigilance, comprehensive monitoring, and specialized counseling.
Our study has some limitations. First, as a spontaneous reporting system, the FAERS has inherent shortcomings, such as duplicate records with variable information quality. Despite manual corrections and deletions, only a few duplicate cases may exist [53, 54]. Second, due to the limited availability of TTO data, the number of valid cases may be inadequate. Consequently, the conclusions drawn from the TTO analysis should be regarded as low-quality evidence. Third, false-negative analysis is a test that we propose based on the specific situation of this study. However, it is not yet widely used in the field of pharmacovigilance. Therefore, its application warrants careful consideration. Fourth, the SSIBs defined in our study were PTs included for Suicidal and self-injurious behaviors (HLGT level). Given the differences in the MedDRA’s categorization rules, some potential PTs that were not included may exist, e.g., depression suicidal (belonging to HLGT level, depressed mood disorders and disturbances) and intentional overdose (belonging to HLGT level, overdoses, and underdoses NEC).
The FAERS database has become the most widely used ADR database in recent years. By mining and analyzing the FAERS database, this study addressed concerns about the potential association between GLP-1RAs and SSIBs and helped dispel public concerns regarding drug safety. The majority of SSIB cases reported in the current RCT and post-marketing study are not considered to be related to GLP-1 RAs. The disproportionate analyses conducted concurrently with our study, based on the FAERS database with varying year spans, also indicate no direct association between GLP-1RAs and SSIBs [55, 56]. In a retrospective analysis utilizing electronic health records, researchers noted that semaglutide can even reduce the risk of suicide compared to non-GLP-1 RAs anti-obesity medications [57]. However, given the rarity of the occurrence of SSIBs, the size of the RCT, and the limitations of the retrospective studies, higher-quality and larger prospective trials are needed to determine the credibility of the current conclusions.
Conclusions
This study explored the relationship between GLP-1RAs and SSIBs through disproportionality analysis. This study found no evidence reasonably suggesting an association between GLP-1RA and SSIBs based on clinical characteristics, TTO, disproportionality, and co-medication analysis. Comparatively, clinicians should pay more attention to the psychiatric status of patients with a history of neuropsychotropic drugs, and more comprehensive monitoring is needed to consider their susceptibility to SSIBs carefully. The results of this study have a positive impact on medication safety for patients with type 2 diabetes or obesity, which is important in maintaining public health and providing strong support for clinical medication decisions.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the US FAERS database (https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html). The code generated and/or analyzed in the current study is available from the corresponding author on reasonable request.
Abbreviations
- GLP-1RAs:
-
Glucagon-like peptide 1 receptor agonists
- GLP-1:
-
Glucagon-like peptide 1
- ADRs:
-
Adverse drug reactions
- SSIBs:
-
Suicidal or self-injurious behaviors
- EMA:
-
European Medicines Agency
- FDA:
-
The Food and Drug Administration
- FAERS:
-
The Food and Drug Administration Adverse Event Reporting System
- MedDRA:
-
The Medical Dictionary for Regulatory Activities
- TTO:
-
Time-to-onset
- CI:
-
Confidence interval
- IC:
-
Information Component
References
Lingvay I, Leiter LA. Use of GLP-1 RAs in cardiovascular disease prevention: a practical guide. Circulation. 2018;137:2200–2.
Patorno E, Htoo PT, Glynn RJ, Schneeweiss S, Wexler DJ, Pawar A, et al. Sodium-glucose cotransporter-2 inhibitors versus glucagon-like peptide-1 receptor agonists and the risk for cardiovascular outcomes in routine care patients with diabetes across categories of cardiovascular disease. Ann Intern Med. 2021;174:1528–41.
Ma X, Liu Z, Ilyas I, Little PJ, Kamato D, Sahebka A, et al. GLP-1 receptor agonists (GLP-1RAs): cardiovascular actions and therapeutic potential. Int J Biol Sci. 2021;17:2050–68.
Barritt AS, Marshman E, Noureddin M. Review article: role of glucagon-like peptide-1 receptor agonists in non-alcoholic steatohepatitis, obesity and diabetes-what hepatologists need to know. Aliment Pharmacol Ther. 2022;55:944–59.
Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of Hyperglycemia in Type 2 Diabetes, A consensus report by the american diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753–86.
Jastreboff AM, Kushner RF. New frontiers in obesity treatment: GLP-1 and nascent nutrient-stimulated hormone-based therapeutics. Annu Rev Med. 2023;74:125–39.
Bailey CJ, Flatt PR, Conlon JM. An update on peptide-based therapies for type 2 diabetes and obesity. Peptides. 2023;161:170939.
O’Neil PM, Birkenfeld AL, McGowan B, Mosenzon O, Pedersen SD, Wharton S, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet. 2018;392:637–49.
Chadda KR, Cheng TS, Ong KK. GLP-1 agonists for obesity and type 2 diabetes in children: systematic review and meta-analysis. Obes Rev. 2021;22:e13177.
Tan B, Pan X-H, Chew HSJ, Goh RSJ, Lin C, Anand VV, et al. Efficacy and safety of tirzepatide for treatment of overweight or obesity. A systematic review and meta-analysis. Int J Obes (Lond). 2023;47:677–85.
Pfizer Provides Update on GLP-1-RA Clinical Development Program for Adults with Obesity and Type 2 Diabetes Mellitus | Pfizer. https://www.pfizer.com/news/press-release/press-release-detail/pfizer-provides-update-glp-1-ra-clinical-development. Accessed 8 Aug 2023.
Bezin J, Gouverneur A, Pénichon M, Mathieu C, Garrel R, Hillaire-Buys D, et al. GLP-1 receptor agonists and the risk of thyroid cancer. Diabetes Care. 2023;46:384–90.
He L, Wang J, ** F, Yang N, Huang J, Li Y, et al. Association of glucagon-like peptide-1 receptor agonist use with risk of gallbladder and biliary diseases: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2022;182:513–9.
EMA. EMA statement on ongoing review of GLP-1 receptor agonists. European Medicines Agency. 2023. https://www.ema.europa.eu/en/news/ema-statement-ongoing-review-glp-1-receptor-agonists. Accessed 20 Jul 2023.
Fine KL, Rickert ME, O’Reilly LM, Sujan AC, Boersma K, Chang Z, et al. Initiation of opioid prescription and risk of suicidal behavior among youth and young adults. Pediatrics. 2022;149:e2020049750.
Takeuchi T, Takenoshita S, Taka F, Nakao M, Nomura K. The relationship between psychotropic drug use and suicidal behavior in Japan: Japanese adverse drug event report. Pharmacopsychiatry. 2017;50:69–73.
Gonda X, Dome P, Serafini G, Pompili M. How to save a life: From neurobiological underpinnings to psychopharmacotherapies in the prevention of suicide. Pharmacol Ther. 2023;244:108390.
Hughes JL, Horowitz LM, Ackerman JP, Adrian MC, Campo JV, Bridge JA. Suicide in young people: screening, risk assessment, and intervention. BMJ. 2023;381:e070630.
**g Y, Liu J, Ye Y, Pan L, Deng H, Wang Y, et al. Multi-omics prediction of immune-related adverse events during checkpoint immunotherapy. Nat Commun. 2020;11:4946.
Raschi E, Fusaroli M, Giunchi V, Repaci A, Pelusi C, Mollica V, et al. adrenal insufficiency with anticancer tyrosine kinase inhibitors targeting vascular endothelial growth factor receptor: analysis of the FDA adverse event reporting system. Cancers (Basel). 2022;14:4610.
**a S, Gong H, Zhao Y, Guo L, Wang Y, Ma R, et al. Tumor lysis syndrome associated with monoclonal antibodies in patients with multiple myeloma: a pharmacovigilance study based on the FAERS database. Clin Pharmacol Ther. 2023;114:211–9.
Zhou J, Wei Z, Xu B, Liu M, Xu R, Wu X. Pharmacovigilance of triazole antifungal agents: analysis of the FDA adverse event reporting system (FAERS) database. Front Pharmacol. 2022;13:1039867.
Ren W, Wang W, Guo Y. Analysis of adverse reactions of aspirin in prophylaxis medication Based on FAERS database. Comput Math Methods Med. 2022;2022:7882277.
Yu RJ, Krantz MS, Phillips EJ, Stone CA. Emerging causes of drug-induced anaphylaxis: a review of anaphylaxis-associated reports in the fda adverse event reporting system (FAERS). J Allergy Clin Immunol Pract. 2021;9:819–829.e2.
Hu Y, Bai Z, Tang Y, Liu R, Zhao B, Gong J, et al. Fournier gangrene associated with sodium-glucose cotransporter-2 inhibitors: a pharmacovigilance study with data from the U.S. FDA Adverse event reporting system. J Diabetes Res. 2020;2020:3695101.
Liu L, Chen J, Wang L, Chen C, Chen L. Association between different GLP-1 receptor agonists and gastrointestinal adverse reactions: a real-world disproportionality study based on FDA adverse event reporting system database. Front Endocrinol (Lausanne). 2022;13:1043789.
Hetrick SE, McKenzie JE, Bailey AP, Sharma V, Moller CI, Badcock PB, et al. New generation antidepressants for depression in children and adolescents: a network meta-analysis. Cochrane Database Syst Rev. 2021;5:CD013674.
Sauzet O, Carvajal A, Escudero A, Molokhia M, Cornelius VR. Illustration of the weibull shape parameter signal detection tool using electronic healthcare record data. Drug Saf. 2013;36:995–1006.
van Puijenbroek EP, Bate A, Leufkens HGM, Lindquist M, Orre R, Egberts ACG. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol Drug Saf. 2002;11:3–10.
Norén GN, Hopstadius J, Bate A. Shrinkage observed-to-expected ratios for robust and transparent large-scale pattern discovery. Stat Methods Med Res. 2013;22:57–69.
Trillenberg P, Sprenger A, Machner B. Sensitivity and specificity in signal detection with the reporting odds ratio and the information component. Pharmacoepidemiol Drug Saf. 2023;32:910–7.
Noguchi Y, Tachi T, Teramachi H. Comparison of signal detection algorithms based on frequency statistical model for drug-drug interaction using spontaneous reporting systems. Pharm Res. 2020;37:86.
Anderson N, Borlak J. Correlation versus causation? Pharmacovigilance of the analgesic flupirtine exemplifies the need for refined spontaneous ADR reporting. PLoS One. 2011;6:e25221.
Fusaroli M, Raschi E, Giunchi V, Menchetti M, Rimondini Giorgini R, De Ponti F, et al. Impulse control disorders by dopamine partial agonists: a pharmacovigilance-pharmacodynamic assessment through the FDA adverse event reporting system. Int J Neuropsychopharmacol. 2022;25:727–36.
Raschi E, Fusaroli M, Ardizzoni A, Poluzzi E, De Ponti F. Cyclin-dependent kinase 4/6 inhibitors and interstitial lung disease in the FDA adverse event reporting system: a pharmacovigilance assessment. Breast Cancer Res Treat. 2021;186:219–27.
Horska K, Ruda-Kucerova J, Skrede S. GLP-1 agonists: superior for mind and body in antipsychotic-treated patients? Trends Endocrinol Metab. 2022;33:628–38.
Kelly AS, Auerbach P, Barrientos-Perez M, Gies I, Hale PM, Marcus C, et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N Engl J Med. 2020;382:2117–28.
O’Neil PM, Aroda VR, Astrup A, Kushner R, Lau DCW, Wadden TA, et al. Neuropsychiatric safety with liraglutide 3.0 mg for weight management: Results from randomized controlled phase 2 and 3a trials. Diabetes Obes Metab. 2017;19:1529–36.
Li J-R, Cao J, Wei J, Geng W. Case report: Semaglutide-associated depression: a report of two cases. Front Psychiatry. 2023;14:1238353.
Klinitzke G, Steinig J, Blüher M, Kersting A, Wagner B. Obesity and suicide risk in adults–a systematic review. J Affect Disord. 2013;145:277–84.
da Silva Bandeira BE, Dos Santos Júnior A, Dalgalarrondo P, de Azevedo RCS, Celeri EHVR. Nonsuicidal self-injury in undergraduate students: a cross-sectional study and association with suicidal behavior. Psychiatry Res. 2022;318:114917.
Yan Y, Gong Y, Jiang M, Gao Y, Guo S, Huo J, et al. Utilization of glucagon-like peptide-1 receptor agonists in children and adolescents in China: a real-world study. Front Endocrinol (Lausanne). 2023;14:1170127.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Yaribeygi H, Sathyapalan T, Sahebkar A. Molecular mechanisms by which GLP-1 RA and DPP-4i induce insulin sensitivity. Life Sci. 2019;234:116776.
Jespersen MJ, Knop FK, Christensen M. GLP-1 agonists for type 2 diabetes: pharmacokinetic and toxicological considerations. Expert Opin Drug Metab Toxicol. 2013;9:17–29.
Gliatto MF, Rai AK. Evaluation and treatment of patients with suicidal ideation. Am Fam Physician. 1999;59:1500–6.
Battini V, Van Manen RP, Gringeri M, Mosini G, Guarnieri G, Bombelli A, et al. The potential antidepressant effect of antidiabetic agents: New insights from a pharmacovigilance study based on data from the reporting system databases FAERS and VigiBase. Front Pharmacol. 2023;14:1128387.
Darwish AB, El Sayed NS, Salama AAA, Saad MA. Dulaglutide impedes depressive-like behavior persuaded by chronic social defeat stress model in male C57BL/6 mice: Implications on GLP-1R and cAMP/PKA signaling pathway in the hippocampus. Life Sci. 2023;320:121546.
Rubino DM, Greenway FL, Khalid U, O’Neil PM, Rosenstock J, Sørrig R, et al. Effect of weekly subcutaneous semaglutide vs daily liraglutide on body weight in adults with overweight or obesity without diabetes: the STEP 8 randomized clinical trial. JAMA. 2022;327:138–50.
Rubino D, Abrahamsson N, Davies M, Hesse D, Greenway FL, Jensen C, et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the STEP 4 randomized clinical trial. JAMA. 2021;325:1414–25.
Wadden TA, Bailey TS, Billings LK, Davies M, Frias JP, Koroleva A, et al. Effect of subcutaneous semaglutide vs placebo as an adjunct to intensive behavioral therapy on body weight in adults with overweight or obesity: the STEP 3 randomized clinical trial. JAMA. 2021;325:1403–13.
Davies M, Færch L, Jeppesen OK, Pakseresht A, Pedersen SD, Perreault L, et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet. 2021;397:971–84.
Sakaeda T, Tamon A, Kadoyama K, Okuno Y. Data mining of the public version of the FDA adverse event reporting system. Int J Med Sci. 2013;10:796–803.
Khaleel MA, Khan AH, Ghadzi SMS, Adnan AS, Abdallah QM. A Standardized dataset of a spontaneous adverse event reporting system. Healthcare (Basel). 2022;10:420.
McIntyre RS, Mansur RB, Rosenblat JD, Kwan ATH. The association between glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and suicidality: reports to the Food and Drug Administration Adverse Event Reporting System (FAERS). Expert Opin Drug Saf. 2023;1–9. Online ahead of print.
Chen C, Zhou R, Fu F, **ao J. Postmarket safety profile of suicide/self-injury for GLP-1 receptor agonist: a real-world pharmacovigilance analysis. Eur Psychiatry. 2023;66:e99.
Wang W, Volkow ND, Berger NA, Davis PB, Kaelber DC, Xu R. Association of semaglutide with risk of suicidal ideation in a real-world cohort. Nat Med. 2024. https://doi.org/10.1038/s41591-023-02672-2.
Acknowledgements
Thanks to the US FDA for providing a free source of data for the study.
Prior presentation
This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
X.M.W. and M.B.L. designed the study. J.X.Z., Y.Z., and B.H.X. researched data, contributed to the discussion, and wrote the first draft of the manuscript. Y.F.Z. and S.J.L. provide the code of analysis. L.E.Z. and Y.H.L. performed the co-medication analysis. C.L.L. polished the language of the manuscript. X.M.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Authors’ Twitter handles
@JX_ZHOU_FJMU
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was not required as the study was conducted using de-identified publicly available data.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Fig S1. The main steps in the processing of the FAERS database. Fig S2. Summary of the workflow for calculation of the sensitivity. Fig S3. Changes in IC025 values for each GLP-1 RA after gradual expansion of case number. Fig S4. Information on 81 cases with a history of psychotic drug use. Fig S5. Comparison of IC025 for Each GLP-1 RA in Different Age Groups of Adults. Fig S6. Comparison of IC025 for suicide or self-injury. Table S1. List of adverse reactions of SSIBs included in this study. Table S2. The 4 × 2 contingency table for signal detection of drug-drug interaction. Table S3. Cases of monotherapy and polytherapy with GLP-1 RAs. Table S4. The performance test of goodness-of-fit among four parametric distribution models. Table S5. Time-to-onset analysis of SSIBs associated with GLP-1 RA in the FAERS database. Table S6. IC025 and Ω025 of top 23 medications. Table S7. The raw data of time to onset analysis in the 52 valid cases. Table S8. The raw data from primary, false-negative, sensitivity and subgroup analyses in calculate disproportionality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, J., Zheng, Y., Xu, B. et al. Exploration of the potential association between GLP-1 receptor agonists and suicidal or self-injurious behaviors: a pharmacovigilance study based on the FDA Adverse Event Reporting System database. BMC Med 22, 65 (2024). https://doi.org/10.1186/s12916-024-03274-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03274-6