Abstract
Background
Depression and anxiety are highly prevalent, but often unrecognized in adults with vision impairment (VI) or blindness. The purpose of this study was to explore visually impaired and blind adults’ views on facilitators and barriers in recognizing and discussing mental health problems.
Methods
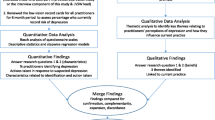
Semi-structured interviews, based on the Integrated Model for Change, were conducted with 16 visually impaired or blind adults receiving support from three Dutch low vision service organizations. Interview data was analyzed using the framework approach.
Results
Participants perceived their focus on practical support with regard to their VI, lack of mental health literacy, and misattribution of symptoms of depression or anxiety as barriers for recognizing mental health problems. With regard to discussing mental health problems, they perceived difficulties in acknowledging their VI and mental health problems due to feelings of vulnerability and inequality. Participants mentioned that their social support system and healthcare providers (could) facilitate them in recognizing and discussing mental health problems. However, participants thought that healthcare providers currently often lacked the knowledge, skills and attitude to recognize and discuss this topic with their clients.
Conclusion
Our findings suggest that visually impaired and blind adults may experience several barriers to recognize, acknowledge and discuss mental health. Healthcare providers and social support systems seem essential for them in reducing these barriers. However, there might be a mismatch between the needs of visually impaired and blind adults and healthcare providers’ knowledge, skills and attitude. Training healthcare providers may improve detection of depression and anxiety in adults with VI or blindness, and enhance clinician-patient communication on mental health.
Similar content being viewed by others
Introduction
Current estimates of people who are blind or have moderate or severe vision impairment, are around 338 million, and are expected to increase to 535 million people by the year 2050 [1]. Vision impairment (VI) and blindness may have a direct effect on physical dysfunction and limitations in daily life activities, and may lead to increased symptoms of depression and anxiety. About 5 % of adults with VI or blindness has a major depressive disorder and about 7 % has an anxiety disorder [2]. Moreover, one in three experience subthreshold symptoms of depression and/or anxiety [2,3,4,5], indicating clinically significant symptoms but no actual disorder. Based on these prevalence estimates, approximately 100,000 visually impaired or blind adults living in the Netherlands experience subthreshold depression and/or anxiety [6, 7]. These prevalence estimates are significantly higher compared to the general population [2]. In visually impaired and blind adults, having (subthreshold) depression can lead to decreased health-related and vision-related quality of life and visual functioning [8]. Less is known about the effects of (subthreshold) anxiety in adults with VI or blindness [9]. However, they more often experience anxiety related to specific places or situations and social situations compared to normally sighted peers [2]. An early treatment approach is recommended to reduce negative influences on quality of life and to prevent development of a full blown disorder.
Despite effective mental health treatments available for people with VI or blindness [10], more than half do not receive any mental health support for depression or anxiety [11,12,13]. Different barriers for receiving treatment are expressed by visually impaired and blind adults. A former study showed that they often experience a lack of knowledge about symptoms and treatment possibilities, followed by not wanting to rely on others [11]. Symptoms of depression and anxiety seem to be systematically overlooked by visually impaired and blind adults themselves, but also by others.
Healthcare providers, i.e. eye care practitioners and low vision service workers, often do not recognize depression in visually impaired and blind adults. From the perspective of healthcare providers, this may be due to their focus on physical health instead of psychological health [14]. A lack of confidence in eye care practitioners’ knowledge and skills seems to limit them in recognizing symptoms of depression in adults with VI or blindness [15]. Other examples of barriers experienced by eye care practitioners and low vision service workers are lack of training in recognizing depression, absence of standard procedures within their organizations to detect depression, limited time and high workload [14, 16]. Moreover, many eye care practitioners believe visually impaired and blind adults themselves create barriers: denial and a defensive attitude are the most common barriers mentioned [14]. Healthcare providers believe reluctance to discuss depression might be due to difficulties in communication, social stigma related to depression, or perceived negative consequences of acknowledging depression [14, 15].
While a few studies investigated barriers from the healthcare providers’ perspective, so far, no in-depth research has been performed to explore the perspective of visually impaired and blind adults. In addition, previous research focused on detection of depression, leaving anxiety underexposed, while prevalence estimates of anxiety are high as well [2]. Therefore, this study aimed to explore the process of recognizing and discussing depression and anxiety in visually impaired and blind adults. Barriers and facilitators that contribute to the identification and discussion were explored, with special attention on the healthcare provider’s role.
Methods
Study design and participants
Visually impaired and blind adults who experienced depression or anxiety were recruited to participate in this qualitative study. The following eligibility criteria were used: (1) 18 years and older; (2) current or history of (subthreshold) depression and/or anxiety; (3) moderate visual impairment, severe visual impairment or blindness according to the World Health Organization (WHO) criteria [17]. Adults with severely impaired cognitive abilities or minimal understanding of the Dutch language were excluded from participation. The six-item screener, a short version of the Mini Mental State Examination, was used to measure participants’ cognitive abilities with scores lower than three indicating severely impaired cognitive abilities [18].
Participants were purposively recruited from three Dutch low vision service organizations. These low vision service organizations provide multidisciplinary services to support people in dealing with their vision impairment and blindness. Mostly outpatient services are provided, such as prescribing low vision aids, mobility training and counseling, but also long and short term inpatient care is provided. Psychologists working at the low vision service organizations were asked to select eligible participants based on the clients’ medical history, approach them by telephone or during face-to-face meetings, offer them a written information letter and informed consent form, and answer questions if applicable. All participants provided written consent. One participant who consented to participate dropped out due to declining mental health.
Data collection
Semi-structured face-to-face interviews with individual participants were performed by the first author (EvM), who worked as a researcher at one of the low vision service organizations, but had no prior relationship with the participants. Interviews were conducted at the participant’s home, except for two interviews that were conducted at the low vision service organization. Participants were allowed to bring a trusted person to the interview, which occurred during two interviews. Interviews lasted between 27 and 85 min (mean = 64 min), were audio-recorded and transcribed verbatim. Immediately after each interview field notes were completed and recorded emotions expressed by the participant, descriptions of concrete situations provided, statements about difficulty remembering, reflections on own experiences, general perspectives, and experiences of the interviewer.
Theoretical framework
The Integrated Change model of de Vries et al. (e.g. the I-Change model) was used as a theoretical framework to develop the interview guide (see Additional file 1), and to analyze barriers and facilitators for the detection and discussion of depression and anxiety [19]. The I-Change model is an integrative model using several scientific models about social cognition, and explains motivational and behavioral change. I-Change is used in research about healthcare utilization from both healthcare provider and client perspective [20, 21]. According to the I-Change model, behavior is determined by someone’s intention, which is influenced by motivational factors (i.e. attitude, social influence and self-efficacy). In turn, these motivational factors are determined by awareness factors (i.e. knowledge, cues to action and risk perception) and predisposing factors. In these predisposing factors, personal factors and sociocultural factors can be determined [19].
Analyses
Thematic analysis of the interview data was performed to describe and understand barriers and facilitators. I-Change model determinants were used as the coding framework [22]. All analyses were performed by two researchers (EvM, HvdA) using Atlas.ti8 software. The first step of analyzing the interview data involved open coding to help the researchers get familiar with the data. Several interviews were coded and consensus was reached, based on which the codebook was developed. Second, the codebook was used to analyze all interviews. Third, codes were clustered into subthemes. It was concluded that the last interview lacked new subthemes indicating that data saturation may have been reached. Subsequently, subthemes were summarized into main themes and assigned to domains based on consensus between the two researchers. Finally, field notes were checked to determine the degree of incompleteness due to lack of reflective ability or the ability of participants to look at their own situation from a distance, in a more general perspective.
Results
Sixteen adults with VI or blindness (44 % male) participated in this study. Mean age was 60 years and ranged between 33 and 91 years. Participants’ medical files showed different diagnoses as cause of their VI (Table 1). In six participants comorbidities, such as hearing loss, autism spectrum disorder or physical complaints, were present.
Barriers and facilitators
Main themes and subthemes identified through the inductive process were mapped to domains within the I-Change model. These were: (1) predisposing factors, (2) environmental factors, (3) awareness related factors, and (4) motivational factors. Two domains were added based on the input that was gathered: (5) social support system and (6) healthcare provider’s role. Table 2 represents all facilitators and barriers gathered within these domains, their themes and sub-themes.
Predisposing factors
Participants used various ways to cope with their mental health problems. More than half of them mentioned a passive or ineffective co** strategy, such as denial and overcompensation by wanting to show others that their VI had no or a minimal effect on their life. Active problem solving was addressed as an often used co** strategy by a few participants. Some of them tried to solve their problems relying on their own resources, while others took the initiative to ask for help, most often from their general practitioner (GP). “My husband cannot fix this. A guide dog cannot solve this. I am the only one who can solve this, but I have to act now. Therefore, I went to my general practitioner (female, aged 49, blind).”
Environmental factors
A few participants mentioned that receiving care from low vision service organizations increased their likelihood of discussing depression or anxiety, in any stage of the symptoms, just because they had access to a low vision service worker. In addition, having a VI changed some participants’ perspectives on social inclusion due to perceived stigma and an experienced lack of equality. They felt that their VI made them different, vulnerable and unequal to others, and that discussing mental health problems would increase those feelings. One participant mentioned: “I feel like they are looking down on me, because I am already different from everyone else. (…) If I can just participate in society in a normal way or if everyone sees me as a normal person, that is already so different. Then mental health problems become less uncomfortable and more negotiable (female, aged 41, blind).”
Awareness
In the beginning almost all participants focused on the practical implications of their VI, and therefore failed to acknowledge its impact on their mental health. In addition, half of the participants mentioned misattribution of symptoms limited their recognition. They thought symptoms such as having low energy, physical complaints and having less interest in activities were related to their old age, their personality, medicines they used, a previous accident or their VI instead of acknowledging them as mental health problems.
Whenever I feel like something is wrong with me, I blame it on the car accident I had 34 years ago. I do not know if that makes sense. I mean, old age comes with deficiencies (female, aged 58, low vision).
Later on in the co** process, participants became aware of the significant impact of the VI on their mental health. They often believed that feelings of vulnerability and inequality that they experienced based on their VI aggravated their mental health problems. They also linked co** with permanent loss, or future losses in progressive eye diseases, to depression and anxiety. One participant explained: “Vision loss is bigger than just losing your sight. There is so much more you cannot do anymore, which makes you feel worthless and changes you as a person (female, aged 49, blind).”
Being unaware of possibilities for receiving mental health support was often mentioned as a barrier for discussing symptoms, especially within low vision service organizations. Two participants still lacked knowledge about where to find appropriate care. Some participants explained that their reduced ability to collect visual information may have caused this lack of knowledge: “The general practitioner’s waiting room is full of posters. If you are a good sighted person waiting, you can look around and can be triggered to investigate a subject further on the internet. As a blind person you just happen to hear it or need to think of it yourself (female, aged 41, blind).” Because of the decreased ability to receive and collect information, participants stressed the importance of healthcare providers, i.e. eye care practitioners, general practitioners and low vision service workers, to provide appropriate information. This information should be about the increased risk of depression and anxiety in people with VI and blindness, and about possibilities for support.
Motivation
Both advantages and disadvantages of discussing feelings of depression and anxiety with a healthcare provider emerged. The prospect of receiving support was mentioned as an advantage. Participants felt that tailored support could help them comprehend and improve their situation, and help them feel in control again. Disadvantages included fear of further deterioration of mental health by discussing it, fear of potential changes in daily life, and the need to acknowledge their VI. One participant explained: “The moment I was going to discuss it with a psychologist, I had to admit something was wrong. I miss something (vision) and I have to adjust my life accordingly. I wasn’t ready until last year (female, aged 47, blind).”
Participants often considered their VI made discussing mental health with a healthcare provider more difficult. Several of them indicated that their VI made it difficult to open up about their mental health problems, because they had to acknowledge their disability and deal with its consequences. Also, they had to open up about two subjects that made them feel vulnerable. One participant mentioned VI could also decrease trust in others, because it limits interpretation of body language. Another participant referred to having depression as an extra burden on top of his VI: “People without vision loss do not struggle with a visual impairment. Therefore, they have the capacity and time to put energy in other things, like feelings of depression (male, aged 33, blind).”
Social support system
Informal emotional support was indicated as a significant facilitator in recognizing and discussing depression and anxiety. More than half of the participants felt guided by a loved one, who helped them to recognize the symptoms of depression or anxiety, and encouraged them to discuss it with a healthcare provider. However, some participants lacked informal support or received more practical solutions, e.g. write feelings down or get a guide dog. Some of them also expressed their loved ones’ incomprehension of the impact of VI on mental health: “It was the beginning of us growing apart. She (partner) literally shrugged her shoulders and said ‘You’ll get over it.’ As if it was a common cold (male, aged 56, blind).” One participant mentioned that VI could limit the size of a person’s social network due to loss of daily activities (e.g. losing their job or decrease in social activities), and therefore might leave them with fewer people that are able to provide informal support.
Healthcare providers
Participants expressed the importance of the healthcare provider’s role in their recognition and willingness to discuss symptoms. They mentioned that eye care practitioners and GPs not often linked the VI with mental health problems and almost never discussed mental health. Nevertheless, participants were positive about their referrals to low vision service organizations, because they expected healthcare providers with knowledge of VI would understand their situation. However, only half of the participants mentioned a low vision service worker discussed mental health after referral, and if discussed, always by social workers or counsellors. In addition, low vision service workers often focused too much on the practical side of low vision rehabilitation and had little attention for the impact of VI on mental health. “VI definitely has an impact. Actually, there are institutions that can help you deal with using an iPad or they tell you that you can no longer drive a car. But in that case your state of mind is ignored (male, aged 80, low vision).”
Participants mentioned that healthcare providers should have a constant focus on possible mental health problems in people with VI, from the first diagnosis until the end of rehabilitation, and anticipate on mental difficulties in the future. “In retrospect, I think it makes sense that healthcare providers confronted me with the fact that my vision is deteriorating and I was probably unable to drive a car in the future. (…) Also acknowledge that it can hurt and make you feel anxious (female, aged 77, low vision).” Eye care practitioners and GPs should be aware of both the physical and emotional impact of VI, and the opportunities for support. Participants stressed the importance of follow-up care to check upon adults with VI or blindness, and referrals to low vision service organizations in an early stage. “I think when ophthalmologists diagnose permanent vision loss, it should trigger them to start providing care (male, aged 64 blind).” Participants recommended that healthcare providers invite them to talk about mental health problems and transfer their knowledge about different aspects of depression and anxiety in relation to the VI, such as prevalence rates, possible symptoms that may be experienced and opportunities for receiving support.
However, participants thought that healthcare providers, especially GPs, often lacked knowledge, confidence, skills, expertise and the proper attitude to detect and discuss depression and anxiety. They mentioned some healthcare providers lacked skills in empathizing with visually impaired and blind adults concerning these symptoms. GPs and eye care practitioners seemed to be unaware of the impact of VI on mental health, and have difficulty referring adults with VI or blindness to the appropriate care, and low vision service workers tended to have difficulty linking the impact of VI with mental health problems as well. Moreover, participants assumed a lack of critical attitude in low vision service workers because they often focused on practical solutions regarding VI, and occasionally trusted participants’ statements about having a good mental health too easily. Participants proposed that healthcare providers consider complaints as an aspect of depression or anxiety, and integrate mental health in their routine care, for example by using a screening instrument. “A general practitioner should check some things in adults with VI by default, such as energy, activities and mood. Ask how everything is going and if necessary: provide a referral (male, aged 33, blind).” Finally, participants indicated a longer, persistent, equal and trustworthy relationship with their healthcare provider as facilitating. According to participants, healthcare providers can establish this by sharing personal stories and considering themselves equal to visually impaired and blind adults.
Discussion
The aim of this study was to explore facilitators and barriers in the detection and discussion of depression and anxiety in visually impaired and blind adults. This study uncovered several important facilitators and barriers in recognizing, acknowledging and discussing mental health that might be specific for visually impaired and blind adults. Their social support system and healthcare providers seemed important facilitators in this process. Our findings may help healthcare providers, low vision service organizations, hospitals, GP practices and policy makers to understand the needs of visually impaired and blind adults, and adjust current care accordingly.
Participants seemed to experience difficulties in recognizing their mental health problems. Some indicated this was due to limited knowledge about the impact of VI on mental health and treatment possibilities. Limited knowledge on mental health (care) is more often reported as a barrier for help-seeking in adults with VI or blindness than in the general population [11, 23, 24]. This may be caused by the limited abilities of people with VI or blindness to obtain processable information, which can lead to low health literacy [25, 26], i.e. the ability to “obtain, process and understand basic health-related information and services to make appropriate health decisions” [27]. Health literacy seems an important facilitator in help-seeking for mental health problems [28]. People with VI or blindness might face specific barriers in obtaining health-related information because it is inaccessible (e.g. posters in a waiting room or information on a website). This emphasizes the importance of using accessible and tailored ways of informing people with VI or blindness on mental health problems and treatment possibilities, e.g. during contacts with an experienced healthcare provider or via audio recordings on a website. Another important reason for difficulty in recognizing mental health problems may be a misattribution of symptoms. Some symptoms of depression and anxiety, such as loss of daily activities, poorer self-care and fatigue, are often seen in people with VI or blindness [29,30,31], but can also be symptoms of mental health problems as they are highly prevalent in this population. It is warranted to educate visually impaired and blind adults about their increased risk of mental health problems, symptoms to recognize depression and anxiety and possibilities for support, also called psychoeducation, at the start of the eye disease and again if they qualify for low vision services.
Participants acknowledged that depression and anxiety are highly prevalent in people with VI or blindness. However, they seemed to encounter difficulties in being open about their mental health problems. Previous studies in adults with VI or blindness confirm this and sometimes even find that they tend to deny psychological distress [32, 33]. Some participants indicated that visually impaired and blind adults need to acknowledge VI or blindness before they can initiate discussing mental health. Nevertheless, mental health problems often occur when someone refuses to acknowledge their disability. People with VI or blindness can be recurrently confronted with their loss, because new situations and new problems keep redefining their loss [34], for instance not being able to see a newborn grandchild can result in another confrontation with being visually impaired or blind. This suggests that adults with VI or blindness need to adapt to and acknowledge their VI repeatedly during their lives. Healthcare providers should be aware of these reoccurring confrontations with loss of vision that may lead to mental health problems. Moreover, feelings of vulnerability, inequality and decreased trust in others seems to limit visually impaired and blind adults to discuss mental health. Many visually impaired and blind adults experience self-stigma on both VI and mental health problems, which may exacerbate these difficulties. Self-stigmatization is the result of internalizing negative stereotypes and may prevent them from seeking help and receiving treatment [35,36,37]. Psychoeducation can potentially reduce self-stigma [38], which emphasizes the importance of healthcare providers to provide information about the link between mental health problems and VI to help visually impaired and blind adults to open up about mental health problems.
Participants often mentioned that support helped them to recognize and discuss mental health problems. Our findings showed that an active problem solving co** strategy seemed to assist visually impaired and blind adults in being able to discuss symptoms with a healthcare provider. However, literature showed that they often report a loss of control, low self-esteem and increased dependency on others for many daily activities [39,40,41]. Especially, adults with VI or blindness with an avoidant co** style seem to experience mental health problems [42] and people with mental health problems seem to have more difficulty in using adaptive co** strategies [43]. Therefore, support seems to be important in visually impaired and blind adults. Support consists of instrumental support (e.g. assisting with tasks of daily living) and emotional support (e.g. affective support) [44]. Strong informal emotional support is associated with help-seeking in mental health problems [45]. However, adults with VI or blindness more often receive instrumental support than emotional support, and most often responsibilities for providing support lies with their family members [46]. Participants experienced different levels of emotional support, that may be explained by adaptation to vision loss. Vision loss is associated with possible isolation from the family, changes in roles and responsibilities between family members, and burden within family members [47,48,49]. Therefore, some social support networks might have focused on providing instrumental support or had limited resources to provide emotional support.
Healthcare providers, i.e. eye care practitioners, general practitioners and low vision service workers, could help visually impaired and blind adults to recognize and discuss mental health problems as well. It seems important that healthcare providers understand the impact of VI on mental health, start a conversation about mental health and share knowledge about prevalence and symptoms of mental health problems. A previous study in women with VI confirms healthcare providers’ importance in achieving health literacy [25]. However, healthcare providers often seem to focus on VI, which is consistent with previous studies [14]. Participants also expressed the need of receiving information about the impact of VI on mental health and sometimes questioned the expertise (e.g. knowledge, skills and attitude) of healthcare providers. Nevertheless, only a quarter of ophthalmic and low vision service workers provides education and information for suspected depression [16]. In addition, they often report a lack of confidence in knowledge and skills as barriers to depression management in adults with VI or blindness [15, 16]. These barriers may have limited healthcare providers in providing information about mental health and treatment options, but also in starting a conversation about depression or anxiety. A possible explanation for the lack of critical attitude might be that healthcare providers think visually impaired and blind adults are often reluctant to discuss mental health [14, 15]. Therefore, there might be a mismatch between the needs of visually impaired and blind adults and healthcare providers’ abilities, resulting in underrecognition of mental health problems.
Strengths and limitations
As far as we know, this study is the first to explore potential barriers and facilitators in recognizing and discussing mental health from the perspective of visually impaired and blind adults. The qualitative design allows us to understand the actual experiences of this fragile population in discussing this highly prevalent problem. Use of the I-Change model to create a comprehensive interview guide adds robustness to our methods and increased reliability of the results. Including a heterogeneous group from different gender, age groups and with various ophthalmic diagnosis and comorbidities contributes to exploring a broad picture of experienced barriers and facilitators.
Despite possible generalizability to adults who do not receive support from a low vision service organization, the results might lack generalizability due to a small sample size, and the lack of diversity in for instance cultural differences, cognitive abilities and (in)experience in discussing mental health problems. The retrospective design of the study allowed participants to share their experiences throughout the process of recognizing and discussing mental health problems. However, it could also have resulted in inaccuracy or incompleteness of recollection, also called recall bias [50]. In addition, some participants showed difficulties to indicate in concrete terms what helped or limited them to recognize, acknowledge and discuss mental health problems. In two interviews a trusted person was present, which could have influenced the results, for instance because the participant did not feel free to answer all questions honestly. Moreover, participants’ psychiatric or physical comorbidities may have aggravated the experienced barriers related to stigma, health literacy and motivation to discuss mental health, but have not been explored since this was not the main focus of this study. Future case studies might take these limitations into account to expand the insights acquired within this study.
Clinical implications
An important implication for clinical practice is that healthcare providers, i.e. ophthalmologists, general practitioners and low vision service workers, should be aware of potential limitations adults with VI or blindness experience in recognizing and discussing mental health problems. In addition, they should understand their influence on the acknowledgement of and willingness to discuss mental health issues in visually impaired and blind adults. GPs’ knowledge on VI and overall healthcare providers’ knowledge on the impact of VI on mental health should be increased. Moreover, standard procedures could be introduced, with a screening instrument as a routine part of care. This might facilitate healthcare providers to start a conversation about the impact of VI on mental health. Finally, healthcare providers could actively provide information about depression and anxiety (psychoeducation), in a way that is suitable for visually impaired and blind adults (verbally, digitally or in Braille) to increase health literacy and reduce self-stigma.
Conclusions
This study has revealed important factors related to the detection and discussion of depression and anxiety in visually impaired and blind adults. The results suggest that an increased vulnerability of adults with VI or blindness, concerning difficulty acknowledging both their VI and mental health problems, low health literacy, difficulty of attributing symptoms to the right impairment and reluctance to discuss symptoms, complicates recognizing and discussing mental health problems. Both the social support system and healthcare providers can play an important role in eliminating these barriers. Insights from this study could facilitate training for healthcare providers to improve detection and clinician-patient communication about depression and anxiety in adults with VI or blindness. Ultimately, this might improve quality of care and subsequently the quality of life of visually impaired and blind adults.
Availability of data and materials
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of research participants. Interview guide is included as supplementary material.
Abbreviations
- GP:
-
General practitioner.
- SD:
-
Standard deviation.
- VI:
-
Visual impairment.
References
Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9(2):e130-e43.
van der Aa HPA, Comijs HC, Penninx BWJH, van Rens GHMB, van Nispen RMA. Major depressive and anxiety disorders in visually impaired older adults. Invest Ophthalmol Vis Sci. 2015;56(2):849–54.
Horowitz A, Reinhardt JP, Kennedy GJ. Major and subthreshold depression among older adults seeking vision rehabilitation services. Am J Geriatr Psychiatry. 2005;13(3):180–7.
Augustin A, Sahel JA, Bandello F, Dardennes R, Maurel F, Negrini C, et al. Anxiety and depression prevalence rates in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2007;48(4):1498–503.
Evans JR, Fletcher AE, Wormald RP. Depression and anxiety in visually impaired older people. Ophthalmology. 2007;114(2):283–8.
Keunen JEE, Verezen CA, Imhof S, van Rens GHMB, Asselbergs MB, Limburg JJH. Toename in de vraag naar oogzorg in Nederland 2010–2020. Ned Tijdschr Geneeskd. 2011;155(41):1828–33.
Limburg H, Keunen JEE. Blindness and low vision in The Netherlands from 2000 to 2020-modeling as a tool for focused intervention. Ophthalmic Epidemiol. 2009;16(6):362–9.
Renaud J, Bedard E. Depression in the elderly with visual impairment and its association with quality of life. Clin Interv Aging. 2013;8:931–43.
Demmin DL, Silverstein SM. Visual Impairment and Mental Health: Unmet Needs and Treatment Options. Clin Ophthalmol. 2020;14:4229–51.
van der Aa HP, Margrain TH, van Rens GH, Heymans MW, van Nispen RM. Psychosocial interventions to improve mental health in adults with vision impairment: systematic review and meta-analysis. Ophthalmic Physiol Opt. 2016;36(5):584–606.
van der Aa HP, Hoeben M, Rainey L, van Rens GH, Vreeken HL, van Nispen RM. Why visually impaired older adults often do not receive mental health services: the patient’s perspective. Qual Life Res. 2015;24(4):969–78.
Nollett CL, Bray N, Bunce C, Casten RJ, Edwards RT, Hegel MT, et al. High prevalence of untreated depression in patients accessing low-vision services. Ophthalmology. 2016;123(2):440–1.
Holloway EE, Sturrock BA, Lamoureux EL, Keeffe JE, Rees G. Depression screening among older adults attending low-vision rehabilitation and eye-care services: Characteristics of those who screen positive and client acceptability of screening. Australas J Ageing. 2015;34(4):229–34.
Fenwick EK, Lamoureux EL, Keeffe JE, Mellor D, Rees G. Detection and management of depression in patients with vision impairment. Optom Vis Sci. 2009;86(8):948–54.
Nollett C, Bartlett R, Man R, Pickles T, Ryan B, Acton JH. How do community-based eye care practitioners approach depression in patients with low vision? A mixed methods study. BMC Psychiatry. 2019;19(1):426.
Rees G, Fenwick EK, Keeffe JE, Mellor D, Lamoureux EL. Detection of depression in patients with low vision. Optom Vis Sci. 2009;86(12):1328–36.
Organization WH. Change the definition of blindness (unpublished document). 2016.
Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–81.
de Vries H, Mudde A, Leijs I, Charlton A, Vartiainen E, Buijs G, et al. The European Smoking Prevention Framework Approach (EFSA): an example of integral prevention. Health Educ Res. 2003;18(5):611–26.
Knops-Dullens T, de Vries N, de Vries H. Reasons for non-attendance in cervical cancer screening programmes: an application of the Integrated Model for Behavioural Change. Eur J Cancer Prev. 2007;16(5):436–45.
Segaar D, Bolman C, Willemsen M, De Vries H. Identifying determinants of protocol adoption by midwives: a comprehensive approach. Health Educ Res. 2007;22(1):14–26.
Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–6.
Prins MA, Verhaak PF, Bensing JM, van der Meer K. Health beliefs and perceived need for mental health care of anxiety and depression–the patients’ perspective explored. Clin Psychol Rev. 2008;28(6):1038–58.
van Beljouw I, Verhaak P, Prins M, Cuijpers P, Penninx B, Bensing J. Reasons and determinants for not receiving treatment for common mental disorders. Psychiatr Serv. 2010;61(3):250–7.
Harrison TC, Mackert M, Watkins C. Health literacy issues among women with visual impairments. Res Gerontol Nurs. 2010;3(1):49–60.
Warren M, DeCarlo DK, Dreer LE. Health Literacy in Older Adults With and Without Low Vision. Am J Occup Ther. 2016;70(3):7003270010.
Ratzan S, Parker R, Selden C, Zorn M. National library of medicine current bibliographies in medicine: health literacy. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services. 2000.
O’Connor M, Casey L. The Mental Health Literacy Scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Res. 2015;229(1–2):511–6.
Lamoureux EL, Hassell JB, Keeffe JE. The determinants of participation in activities of daily living in people with impaired vision. Am J Ophthalmol. 2004;137(2):265–70.
O’Conor R, Smith SG, Curtis LM, Benavente JY, Vicencio DP, Wolf MS. Mild Visual Impairment and Its Impact on Self-Care Among Older Adults. J Aging Health. 2018;30(3):327–41.
Schakel W, Bode C, Elsman EBM, van der Aa HPA, de Vries R, van Rens G, et al. The association between visual impairment and fatigue: a systematic review and meta-analysis of observational studies. Ophthalmic Physiol Opt. 2019;39(6):399–413.
Verhaak PF, Prins MA, Spreeuwenberg P, Draisma S, van Balkom TJ, Bensing JM, et al. Receiving treatment for common mental disorders. Gen Hosp Psychiatry. 2009;31(1):46–55.
Wittkampf KA, van Zwieten M, Smits FT, Schene AH, Huyser J, van Weert HC. Patients’ view on screening for depression in general practice. Fam Pract. 2008;25(6):438–44.
Lindgren CL, Burke ML, Hainsworth MA, Eakes GG. Chronic sorrow: a lifespan concept. Sch Inq Nurs Pract. 1992;6(1):27–40; discussion 1–2.
Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry. 2017;210(4):261–8.
Southall K, Wittich W. Barriers to Low Vision Rehabilitation: A Qualitative Approach. Journal of Visual Impairment & Blindness. 2012;106(5):261–74.
Corrigan PW, Larson JE, Kuwabara SA. Social psychology of the stigma of mental illness: Public and self-stigma models. Social psychological foundations of clinical psychology. New York: The Guilford Press; 2010. p. 51–68.
Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW. Empirical Studies of Self-Stigma Reduction Strategies: A Critical Review of the Literature. Psychiatr Serv. 2012;63(10):974–81.
Cimarolli VR, Boerner K, Reinhardt JP, Horowitz A, Wahl HW, Schilling O, et al. A population study of correlates of social participation in older adults with age-related vision loss. Clin Rehabil. 2017;31(1):115–25.
Papadopoulos K, Montgomery AJ, Chronopoulou E. The impact of visual impairments in self-esteem and locus of control. Res Dev Disabil. 2013;34(12):4565–70.
Maaswinkel IM, van der Aa HPA, van Rens G, Beekman ATF, Twisk JWR, van Nispen RMA. Mastery and self-esteem mediate the association between visual acuity and mental health: a population-based longitudinal cohort study. BMC Psychiatry. 2020;20(1):461.
Sturrock BA, ** on Vision-Related Quality of Life in Patients With Low Vision: A Prospective Longitudinal Study. Invest Ophthalmol Vis Sci. 2015;56(4):2416–22.
Aldwin CM, Revenson TA. Does co** help? A reexamination of the relation between co** and mental health. J Pers Soc Psychol. 1987;53(2):337–48.
Kahn RL, Antonucci TC. Convoys over the life course: Attachment, roles, and social support. In: Baltes PB, Brim O, eds. Life-span development and behavior. 3. New York: Academic Press; 1980:253–86.
Polacsek M, Boardman GH, McCann TV. Help-seeking experiences of older adults with a diagnosis of moderate depression. Int J Ment Health Nurs. 2019;28(1):278–87.
Cimarolli VR, Boerner K. Social Support and Well-being in Adults who are Visually Impaired. J Visual Impair Blind. 2005;99(9):521–34.
Percival J, Hanson J. ’I’m Like a Tree a Million Miles from the Water’s Edge’: Social Care and Inclusion of Older People with Visual Impairment. Br J Soc Work. 2005;35(2):189–205.
Goodman CR, Shippy RA. Is it contagious? Affect similarity among spouses. Aging Ment Health. 2002;6(3):266–74.
Braich PS, Jackson M, Knohl SJ, Bhoiwala D, Gandham SB, Almeida D. Burden and Depression in Caregivers of Blind Patients in New York State. Ophthalmic Epidemiol. 2016;23(3):162–70.
Porta M, Last JM, eds. A Dictionary of Public Health. 2 ed. Oxford University Press; 2018. Available at https://www.oxfordreference.com/view/10.1093/acref/9780191844386.001.0001/acref-9780191844386. Accessed 25 Mar 2021.
Acknowledgements
We would like to thank all participating adults and the ‘Programmaraad’ for making this study possible.
Funding
This work was supported by the ‘Programmaraad’; a Dutch funding group from the low vision service organizations Royal Dutch Visio, Bartiméus and the Robert Coppes Foundation. The sponsor had no role in the design and conduct of this study or in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
HvdA, PV and RvN were involved in funding acquisition and contributed to the study conception and design. EvM and HvdA developed the interview scheme. Data collection was performed by EvM and analysis were performed by EvM and HvdA. The first draft of the manuscript was written by EvM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Medical Ethics Committee (METc) of Amsterdam University Medical Centers (UMC), location VUmc, the Netherlands. The METc VUmc issues nationally valid judgements. The study was performed according the standards of the Declaration of Helsinki (1964) and its later amendments. Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Interview guideline.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
van Munster, E.P.J., van der Aa, H.P.A., Verstraten, P. et al. Barriers and facilitators to recognize and discuss depression and anxiety experienced by adults with vision impairment or blindness: a qualitative study. BMC Health Serv Res 21, 749 (2021). https://doi.org/10.1186/s12913-021-06682-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06682-z