Abstract
Background
Health care funding reforms are being used worldwide to improve system performance but may invoke unintended consequences. We assessed the effects of introducing a targeted hospital funding model, based on fixed price and volume, for hip fractures. We hypothesized the policy change was associated with reduction in wait times for hip fracture surgery, increase in wait times for non-hip fracture surgery, and increase in the incidence of after-hours hip fracture surgery.
Methods
This was a population-based, interrupted time series analysis of 49,097 surgeries for hip fractures, 10,474 for ankle fractures, 1,594 for tibial plateau fractures, and 40,898 for appendectomy at all hospitals in Ontario, Canada between April 2012 and March 2017. We used segmented regression analysis of interrupted monthly time series data to evaluate the impact of funding reform enacted April 1, 2014 on wait time for hip fracture repair (from hospital presentation to surgery) and after-hours provision of surgery (occurring between 1700 and 0700 h). To assess potential adverse consequences of the reform, we also evaluated two control procedures, ankle and tibial plateau fracture surgery. Appendectomy served as a non-orthopedic tracer for assessment of secular trends.
Results
The difference (95 % confidence interval) between the actual mean wait time and the predicted rate had the policy change not occurred was − 0.46 h (-3.94 h, 3.03 h) for hip fractures, 1.46 h (-3.58 h, 6.50 h) for ankle fractures, -3.22 h (-39.39 h, 32.95 h) for tibial plateau fractures, and 0.33 h (-0.57 h, 1.24 h) for appendectomy (Figure 1; Table 3). The difference (95 % confidence interval) between the actual and predicted percentage of surgeries performed after-hours − 0.90 % (-3.91 %, 2.11 %) for hip fractures, -3.54 % (-11.25 %, 4.16 %) for ankle fractures, 7.09 % (-7.97 %, 22.14 %) for tibial plateau fractures, and 1.07 % (-2.45 %, 4.59 %) for appendectomy.
Conclusions
We found no significant effects of a targeted hospital funding model based on fixed price and volume on wait times or the provision of after-hours surgery. Other approaches for improving hip fracture wait times may be worth pursuing instead of funding reform.
Similar content being viewed by others
Background
Health care funding reforms are occurring worldwide in an attempt to improve patient outcomes and decrease medical costs [1, 2]. Among the 37 OECD member countries, for example, total health expenditures as a percent of GDP ranged in 2019 from 4.4 % in Turkey to 17.0 % in the United States, with Canada at 10.8 % [3]. Similarly, evidence shows that the everyday practice of medicine is “characterised by wide variations that have no basis in clinical science”, leading to variability in patient outcomes [4].
These reforms include “Quality-Based Procedures (QBPs)”, a hospital funding initiative implemented in Ontario, Canada. QBPs, a novel variant of activity-based funding (ABF) [5], are a procedure- and diagnosis-specific approach to funding hospitals. They involve a pre-set price per episode of care, coupled with a best practice clinical pathway for each of the pre-specified diagnoses and procedures. QBPs replaced part of each hospital’s global budget—the annual operating revenue—with a prospectively determined amount targeted at those procedures and diagnoses [6, 7]. The funding for QBPs was carved out of each hospital’s global budget, and then reallocated back as a fixed price for a fixed volume of targeted care.
Hip fracture surgery was among the procedures selected for targeted funding through the QBP mechanism because of its relatively high mortality rate, [8] cost to the health care system, [9, 10] and variation in care associated with these injuries [11]. In parallel with the QBP funding change, handbooks outlining best practice clinical pathways for each QBP, including hip fracture surgery, were developed and disseminated to encourage standardization of care. [12] The clinical pathway was intended to encourage reduced wait times for surgery [1, 2] because delays for hip fracture surgery are associated with increased complications, [13,14,15] medical costs, [10] and length of stay [10]. The theory was that because longer waits for hip fracture repair increases complications and costs, targeted QBPs funding would encourage reduced waiting times. Prior research has examined this program theory and the rationale underpinning QBPs [1, 2].
To date, whether targeted hospital funding reform has had its intended effect of reducing hip fracture surgery wait times has not been assessed. The aim of this study was to determine whether implementation of the QBP funding reform, along with dissemination of best practice clinical pathways, in a large population-based cohort from Ontario, Canada (2018 population ≈ 14.5 million) was associated with (1) decreased wait times for hip fracture surgery without the unintended consequences of; (2) increased wait times for other extremity fracture surgeries not funded through the QBP mechanism [16]; and/or (3) increased after-hours provision of hip fracture surgery[17]. We hypothesized that implementing targeted QBP funding for hip fracture surgery was associated with reductions in wait times for hip fracture surgery, increases in wait times for non-hip fracture surgery, and increases in the incidence of after-hours hip fracture surgery. We independently evaluated wait times for hip and non-hip fracture surgeries, and incidence of after hours hip fracture surgeries. Our hypothesis was informed by the government’s stated intent to optimize patient outcomes through QBPs, including by reducing wait times [12]. We reasoned that because QBP funding designated for hip fracture surgeries could only be used for that purpose, and because the clinical pathway was intended to help streamline care, hospitals would be incentivized to enable increased hip fracture surgery volumes including after-hours, thereby crowding out non-QBP-funded extremity fractures.
Methods
Study Design and Setting
We conducted an aggregate, population-based, interrupted time series (ITS) analysis of administrative health data from Ontario, Canada, where all medically necessary hospital and physician services are publicly-funded by a single provincial health insurance program.
Data Sources
We used multiple population-wide administrative health databases linked with encoded identifiers to identify study patients and ascertain outcomes. Ontario’s ICES Data Repository consists of record-level, coded, linkable, health data sets, encompassing much of the publicly-funded administrative health services records for the population of Ontario. From this repository, we relied on aspects of the following data: patient demographic information, vital statistics, hospital discharge diagnosis, ICD-10 surgical procedures, and emergency department encounters. Patient demographic information and vital status were obtained from the Ontario Health Insurance Plan (OHIP) Registered Persons Database. The Canadian Institute for Health Information (CIHI) Discharge Abstract Database (CIHI-DAD) contains hospital discharge diagnoses that are coded using International Classification of Diseases 10th revision (ICD-10) and surgical procedures that are identified using Canadian Classification of Health Intervention (CCI) codes. The OHIP Claims History Database contains physician service claims with both diagnosis and procedure codes. Emergency department (ED) encounters were captured using the CIHI National Ambulatory Care Reporting System (NACRS). These datasets are held securely in a linked coded form and were analyzed at ICES in Toronto, Canada (www.ices.on.ca).
Exposure
QBP funding for hip fracture surgery was implemented jurisdiction-wide on April 1, 2014, at the start of the fiscal year. On that date, the Ministry of Health switched funding for hip fracture surgeries from global budget to QBP.
Identification of Patients
We identified all patients in Ontario, Canada undergoing surgery for hip fractures, ankle fractures, tibial plateau fractures, and appendectomy between April 1, 2012 and February 28, 2017. Codes used to identify patients in this study are available in the Table in the supplement. Surgeries for ankle and tibial plateau fractures served as control orthopaedic procedures, since they were not funded by QBPs, enabling us to assess effects on QBP- vs. non-QBP-funded surgeries. Appendectomy served as a non-orthopedic negative control because we did not expect this procedure to be influenced by the QBP funding reform, thereby allowing us to assess secular trends in the overall health care system. All three of these control procedures are funded under each hospital’s global budget, rather than from the targeted QBP funding envelope. Within each of these four cohorts, we excluded non-residents, those under 18 years of age, and patients with missing age, sex, or Ontario health card number. To avoid misclassification, we also excluded patients coded with elective procedures, patients waiting greater than 14 days for surgery, and repeat surgeries occurring within 30 days of hospital admission. Open fractures also were excluded as they are rare and unlikely to be influenced by funding reforms because they are managed urgently ahead of almost all other orthopaedic cases.
Covariates
We reported age, sex, urban or rural location (defined by postal codes), and neighbourhood income quintile (derived from census data). Comorbidity was ascertained using the Deyo-Charlson Co-morbidity Index [21] and hospital encounter data over the 3 years preceding the index surgical admission. We also recorded each patient’s (1) health service utilization (emergency department encounters and hospitalizations) in the year prior to surgery, (2) prior place of residence (long-term care or not), and 3) treating hospital type (teaching versus community).
Outcomes
We measured the mean (± standard deviation [SD]) from time of first presentation at hospital to time the surgical procedure began in hours. Percentage of surgeries performed within 24 h (a clinically relevant time threshold) was also assessed. Time of first presentation was defined as time of ED registration or hospital admittance (for admissions that bypassed an ED). Percentage of surgeries performed after-hours (defined as surgery beginning between 1700 and 0700 h) was also assessed. Timing of (1) first presentation at hospital and (2) start of surgery have been recorded in CIHI-DAD since 2009 (before our study period began) and have previously been used to calculate exact wait times for after-hours provision of surgery [10, 11, 13, 17, 18].
Statistical Analysis
We described patient characteristics stratified by surgical procedure and outcomes annually for each year in the study period. Segmented regression analysis was used to evaluate the statistical significance of changes in wait times and the percentage of after-hours cases for these procedures from before to after the funding policy change. The unit of time for the analysis was one month, with 24 monthly data points pre-policy and 36 monthly data points post-policy. Although QBP funding for all Ontario hospitals performing hip fracture surgeries began simultaneously on April 1, 2014, we excluded from analyses a priori the three months of data immediately following the start of the funding change (one fiscal quarter) to account for a policy “transition” period [19]. We reasoned that by censuring those first three months of observation after the start of the intervention, we could be confident that any observed changes from then on could be attributed to the funding policy change. An automatic fitting procedure in the R statistical software package was used to account for seasonality and determine the number of autocorrelation lags to include in the analysis [20]. We calculated the difference (and 95 % confidence intervals [CIs] for the difference) between the observed rate post-implementation and the predicted rate that would have occurred had QBPs been not implemented [21]. All analyses were performed at ICES using R version 3.4.4 and a two-sided type-I error probability of 0.05. Use of data in this study was authorized under Sec. 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a Research Ethics Board.
Results
Our study included 49,097 patients with hip fracture surgery, 10,474 with ankle fracture surgery, 1,594 with tibial plateau fracture surgery, and 40,898 with appendectomy (Supplementary Table). Table 1 presents the patient characteristics for each cohort at time of surgery. Patients with hip fractures had a mean (SD) age of 80.4 [12] years, which was older than patients within the control fracture and appendectomy cohorts. More females experienced hip and ankle fractures, whereas males and females were equally likely to undergo surgeries for tibial plateau fractures and appendectomy. Patients undergoing hip fracture surgery also had more comorbidities, ED visits, and days in hospital within the year leading up to their fracture. A higher percentage of patients with hip fractures resided in long term care residences (15 %) (compared to ≤1 % of patients in each of the 3 comparator cohorts). Most patients (> 80 % for all groups) were admitted to hospital from the ED. Within the fracture cohorts, the annual mean and median wait times from ED or hospitalization to surgery were shortest for surgeries for ankle fractures, followed by hip fractures, and longest for tibial plateau fractures (Table 2). Within the fracture cohorts, after hours surgery was commonly performed for hip fractures (in 36–39 % of cases) and ankle fractures (in 35–38 %) and only slightly less frequent for tibial plateau fractures (25–26 %).
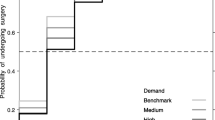
With the implementation of funding reform, there were no significant changes in wait times or provision of after-hours surgery for hip, ankle, or tibial plateau repair or appendectomy (Figs. 1 and 2; Table 3). The difference (95 % CI) between the actual mean wait time post-implementation and the predicted rate had QBPs not been implemented was − 0.46 h (-3.94 h, 3.03 h) for hip fractures, 1.46 h (-3.58 h, 6.50 h) for ankle fractures, -3.22 h (-39.39 h, 32.95 h) for tibial plateau fractures, and 0.33 h (-0.57 h, 1.24 h) for appendectomy (Fig. 1; Table 3). The difference (95 % CI) between the actual percentage of surgeries performed after-hours post-implementation and the predicted rate was − 0.90 % (-3.91 %, 2.11 %) for hip fractures, -3.54 % (-11.25 %, 4.16 %) for ankle fractures, 7.09 % (-7.97 %, 22.14 %) for tibial plateau fractures, and 1.07 % (-2.45 %, 4.59 %) for appendectomy (Fig. 2; Table 3). The percentage of hip fracture surgeries occurring within 24 h was also unchanged after implementation of funding reform [-0.13 % (-6.08 %, 5.82 %)].
Monthly mean wait time (in hours) from hospital presentation to surgery over the study period. For A, B, C, and D, the interrupted time series analysis is displayed on the right. Red solid line represents the fitted model calculated by segmented regression. The red dashed line represents the counterfactual (i.e. if no policy change occurred). The grey vertical dashed line represents the date of policy change. The grey shaded area represents the 3-month “transition” period allowed for policy implementation. There was no statistically significant difference between the fitted model and counterfactual scenario for any surgery type (Table 3).
Percentage of surgeries (1700 – 0700 hours) performed after hours over the study period. For A, B, C, and D, the interrupted time series analysis is displayed on the right. Red solid line represents the fitted model calculated by segmented regression. The red dashed line represents the counterfactual (i.e. if no policy change occurred). The grey shaded area represents the 3-month “transition” period allowed for policy implementation. The grey shaded area represents the “transition” period. There was no statistically significant difference between the fitted model and counterfactual scenario for any surgery type (Table 3).
Discussion
We evaluated the effects of a new hospital funding model on surgical care in this population-based cohort study in Ontario, Canada. We found no significant effects of this policy change on mean hip fracture surgery wait times. The policy change also did not significantly increase wait times for selected non-hip fracture surgeries or the frequency of after-hours surgeries performed. Our findings have important implications for health care system reform as policymakers worldwide experiment with new funding models.
First, other approaches for improving health system performance may be worth pursuing alongside, or instead of, funding reform. Like all “patient focused” variants of activity-based funding, QBPs established a prospective payment rate based on service type and volume. Funding was carved out of hospitals’ global budgets and then reallocated to hospitals at the start of the relevant fiscal year as a fixed price and fixed volume, targeted at each QBP procedure or diagnosis. QBPs may have failed to reduce wait times for hip fracture surgery or standardize care because: (i) QBPs specifically, and funding reform generally, were not the right “tool for the job”; or (ii) the way in which they were implemented compromised their success; or (iii) there were other unexamined contextual factors that may have explained the lack of effect and which may have influenced the circumstances in which QBPs might have produced the desired effects. QBPs differ from most typical ABF reforms in that funding applies only to a very limited set of diagnoses and procedures, and they rely on the voluntary use of handbooks to encourage incorporation of best practices. There is no mechanism in place to enforce (or systematically measure) adherence to the clinical pathways; hospitals are paid via QBPs whether they follow the pathways or not, but the intent was that following the pathways would enable hospitals to deliver care for the amount paid by QBPs. Indeed, prior qualitative work has indicated that QBPs coupled with dissemination of clinical handbooks were not effective at establishing consistent standards of practice [2].
Funding reform also may not be the best way to incentivize changes needed to decrease length of stay and increase patient throughput, especially if existing pressures to make these changes are already strong and/or if the performance levels achieved in this area are already near-optimal given existing constraints [22]. On the one hand, this apparent lack of effect is disappointing given that an excess of 66 % of hip fracture patients in Ontario do not receive surgery within the safe time frame of 24 h [11]. On the other hand, Ontario already out-performs the Canadian averages at present: in a 2018 nationwide study, 77 % of Canadians do not undergo hip fracture surgery within 24 h [14]. Previous qualitative analyses identified delays and others challenges in implementing QBPs in hospitals, which altered the trajectory of this funding reform [2]. Within orthopedic surgery, health care leaders’ early implementation experiences with the QBP for hip and knee replacements, which predated the QBP for hip fractures, identified lack of organisational preparedness as a major barrier [23].
This study has several strengths. Interrupted time series analyses provide a robust quasi-experimental design for inferring causality between health policy interventions and outcomes in the absence of a randomized controlled trial [24]. ITS was ideal given that a difference-in-difference approach was not appropriate since matched controls were not available from the Ontario data. Additional strengths of our study include the single-payer nature of Canada’s publicly-funded health care system, which captures all acute non-elective hip fracture surgeries performed across publicly-funded hospitals in Ontario, and the ability to assess wait times and timing of procedures through standardized data available from a single repository at ICES. The use of control procedures further strengthens our study and suggest a lack of other health system changes targeted at wait times concurrent with the implementation of QBPs. The study was powered to pick up differences, should they have existed, with 24 monthly data points pre-policy and 36 monthly data points post-policy. Excluding open fractures, elective procedures and very long delays avoided misclassification that would have also biased towards finding no differences with policy change.
Some limitations merit emphasis. First, our analyses were confined to health administrative data which lack clinical details to accurately identify more complex patients who are predisposed to both complications and longer wait times to optimize medical status prior to surgery. Second, our study did not assess the effects of other earlier health system interventions impacting wait times, such as the public reporting of wait time performance benchmarks which began in 2009, or the earlier dissemination of hip fracture surgery recommendations in 2005 [25]. However, unless coding practices, clinical care, or patient characteristics changed suddenly close to the time of QBP implementation, which we have no evidence of, any background/secular trends are accounted for in our analysis and pose no threat to the validity of study. Third, patient reported outcome and experience measures (PROMs and PREMs) were not available to us, and it is unknown whether the best practice clinical pathways disseminated for the hip fracture QBP [12] led to improvements in such outcomes. Future research to inform reform efforts could include evaluation of PROMS and PREMS, analysis of the extent to which clinicians voluntarily comply with clinical pathways and/or digital QBP clinical order sets, and investigation of the degree to which funding reform aligns with the intrinsic factors that motivate behaviour in clinicians and health care leaders [26].
Conclusions
The implementation of a novel funding model for hospitals, based on fixed price and volume for targeted procedures and diagnoses, resulted in no significant system-wide effects on hip fracture surgery wait times. The policy change also did not appear to have negative consequences on wait times for other fracture surgeries or in frequency of after-hours surgery. Our findings suggest that other approaches for improving health system performance may be worth pursuing alongside, or instead of, funding reform.
Availability of data and materials
We used population-wide administrative health databases linked at Ontario’s Institute for Clinical Evaluative Sciences (ICES; https://www.ices.on.ca/). Public access to these databases are closed and use of data in this study was authorized under Sec. 45 of Ontario’s Personal Health Information Protection Act.
Abbreviations
- QBPs:
-
Quality-Based Procedures
- ABF:
-
Activity-based funding
- ITS:
-
Interrupted time series
- PROMs and PREMs:
-
Patient reported outcome and experience measures
References
Palmer KS, Brown AD, Evans JM, Marani H, Russell KK, Martin D, et al. Qualitative analysis of the dynamics of policy design and implementation in hospital funding reform. PLoS ONE. 2018;13(1):e0191996.
Palmer KS, Brown AD, Evans JM, Marani H, Russell KK, Martin D, et al. Standardising costs or standardising care? Qualitative evaluation of the implementation and impact of a hospital funding reform in Ontario, Canada. Health Res Policy Syst. 2018;16(1):74.
OECD. Health expenditure and financing. https://stats.oecd.org/Index.aspx?DataSetCode=SHA.
Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ. 2002;325(7370):961–4.
Palmer KS, Agoritsas T, Martin D, Scott T, Mulla SM, Miller AP, et al. Activity-based funding of hospitals and its impact on mortality, readmission, discharge destination, severity of illness, and volume of care: A systematic review and meta-analysis. PLoS ONE. 2014;9(10).
Lave JR, Jacobs P, Markel F. Transitional funding: changing Ontario’s global budgeting system. Health Care Financ Rev. 1992;13(3):77–84.
Wolfe PR, Moran DW. Global budgeting in the OECD countries. Health Care Financ Rev. 1993;14(3):55–76.
Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med. 2017;377(21):2053–62.
Nikitovic M, Wodchis WP, Krahn MD, Cadarette SM. Direct health-care costs attributed to hip fractures among seniors: A matched cohort study. Osteoporos Int. 2013;24(2):659.
Pincus D, Wasserstein D, Ravi B, Huang A, Paterson JM, Jenkinson RJ, et al. Medical Costs of Delayed Hip Fracture Surgery. J Bone Joint Surg Am. 2018;100(16):1387–96.
Pincus D, Wasserstein D, Ravi B, Byrne JP, Huang A, Paterson JM, et al. Reporting and evaluating wait times for urgent hip fracture surgery in Ontario, Canada. CMAJ. 2018;190(23):E702-E9.
Quality-Based Procedures. Clinical Handbook for Hip Fracture. Toronto: Health Quality Ontario; 2013.
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, et al. Association Between Wait Time and 30-Day Mortality in Adults Undergoing Hip Fracture Surgery. JAMA. 2017;318(20):1994–2003.
Sobolev B, Guy P, Sheehan KJ, Kuramoto L, Sutherland JM, Levy AR, et al. Mortality effects of timing alternatives for hip fracture surgery. Cmaj. 2018;190(31):E923-E32.
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90.
McIsaac DI, Abdulla K, Yang H, Sundaresan S, Doering P, Vaswani SG, et al. Association of delay of urgent or emergency surgery with mortality and use of health care resources: a propensity score-matched observational cohort study. Cmaj. 2017;189(27):E905-E12.
Pincus DMa, Desai SJ, Md MF, Wasserstein DMMF, Ravi BMPF, Paterson J, et al. Outcomes of After-Hours Hip Fracture Surgery. [Article]. Journal of Bone Joint Surgery - American Volume June 7. 2017;99(11):914–22.
Ravi B, Pincus D, Wasserstein D, Govindarajan A, Huang A, Austin PC, et al. Association of Overlap** Surgery With Increased Risk for Complications Following Hip Surgery. JAMA Internal Medicine. 2017.
Taljaard M, McKenzie JE, Ramsay CR, Grimshaw JM. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement Sci. 9. England2014. p. 77.
Jebb AT, Tay L, Wang W, Huang Q. Time series analysis for psychological research: examining and forecasting change. Front Psychol. 2015;6:727.
Zhang F, Wagner AK, Soumerai SB, Ross-Degnan D. Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J Clin Epidemiol. 2009;62(2):143–8.
Mathes T, Pieper D, Morche J, Polus S, Jaschinski T, Eikermann M. Pay for performance for hospitals. Cochrane Database of Systematic Reviews. 2019(7).
Baxter P, Cleghorn L, Alvarado K, Cummings G, Kennedy D, McKey C, et al. Quality-based procedures in Ontario: exploring health-care leaders’ responses. J Nurs Manag. 2016;24(1):50–8.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55.
Canadian Institute for Health Information. Wait Times for Priority Procedures in Canada, 2017. Ottawa: CIHI; 2017. [Available from: www.boneandjointcanada.com.
Ivers N, Palmer K. Best Laid Plans: When a Pandemic Complicates Hospital Funding Reform. Insights (Essays). 2020.
Acknowledgements
Not applicable.
Funding
This work was funded through an Ontario Strategy for Patient Oriented Research Support Unit (OSSU) Impact Award, which was, in turn, funded by the Canadian Institutes of Health Research and the Government of Ontario. This study was supported by ICES (www.ices.on.ca), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Parts of this material are based on data and/or information compiled and provided by Canadian Institutes of Health Information (CIHI). The funders and data providers had no role in study design, data analysis, decision to publish, or preparation of the manuscript. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the data providers and funders.
Author information
Authors and Affiliations
Contributions
DP and NMI conceived the study. DP, JW, KSP, and NMI wrote the manuscript. DP, JW, KSP, JMP, NMI and MT created the statistical analysis plan and interpreted the analysis. AL and AH performed the statistical analysis. DW, LLS, AB, and MT participated in drafting and revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Use of data in this study was authorized under Sec. 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a Research Ethics Board.
Consent for publication
Not applicable.
Competing interests
There are no relevant conflicts of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table Description of the Derivation of Each Cohort
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pincus, D., Widdifield, J., Palmer, K.S. et al. Effects of hospital funding reform on wait times for hip fracture surgery: a population-based interrupted time-series analysis. BMC Health Serv Res 21, 576 (2021). https://doi.org/10.1186/s12913-021-06601-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06601-2