Abstract
Background
Pharmacists are recognized as one of the most accessible healthcare providers and are licensed to advise patients on drugs and health products including dietary and herbal supplements (DHSs). The objective of this study was to identify barriers, knowledge, and training that pharmacists report related to DHSs counselling.
Methods
MEDLINE, EMBASE, AMED and CINAHL were systematically searched from database inception to May 8th, 2020. Eligible articles contained qualitative data with a specific focus on pharmacists’ perceived knowledge, training, and barriers to DHSs counselling. Relevant data were extracted, and a thematic analysis was conducted.
Results
Nineteen articles met the inclusion criteria. The following three main themes were identified: challenges to pharmacists obtaining DHSs education, postgraduate workplace challenges surrounding DHSs, and pharmacists’ perceived role and importance on DHSs. Low knowledge of DHSs and the limited regulations surrounding DHSs acting as a barrier to counselling were common findings supported by the eligible articles.
Conclusions
A lack of pharmacists’ knowledge and awareness of DHSs stems from a variety of factors including a lack of education and training in the field, limited regulations surrounding DHSs, and inadequate availability of DHS information resources in the pharmacy. Pharmacists were unable to confidently counsel patients due to these aforementioned factors in addition to reporting that they lacked time. Further research that reviews pharmacy education and workplace training, and improving DHS regulations are warranted future directions.
Similar content being viewed by others
Background
The use of dietary and herbal supplements (DHSs) is highly prevalent worldwide. In countries including the United States, United Kingdom, and Denmark, it has been found that 35–60% of adults use DHSs [1, 2]. In 2016, the Natural Health Product Survey among Consumers conducted in Canada found that 56% of respondents had taken DHSs such as vitamins and minerals at least once per week [3]. From the same survey, 56% of the respondents considered themselves to have poor knowledge about the safety of DHSs [3]. In certain clinic populations, the prevalence of use is even higher; almost all (99%) patients used DHSs, with 46% using DHSs concurrently with prescription medications in a large Canadian naturopathic medicine clinic population, however, 42% of the DHS users had not disclosed this information to their primary care provider [4]. In 1999, a survey conducted in the United States identified that 53% of DHS users believed that DHSs were completely safe to use and rarely ever caused harm [5]. As DHSs are available without a prescription, consumers may self-medicate and suffer the potential risks of drug-DHS interactions. According to a study led by the Mayo Clinic in 2002–2003, 34% of DHS users were at risk of suffering potential herb-drug interactions [5]. A number of studies have identified DHS-drug interactions leading to adverse events [6, 7], which is of great concern as many patients often do not consult with their healthcare provider(s) before using DHSs.
The regulatory environment related to DHSs varies across many different countries. Two categories of regulations exist for DHSs: premarket and postmarket regulations [8,9,10]. Effective premarket regulations require evidence on safety and efficacy to be provided through scientific literature [8]. Additionally, the manufacturing process, quality, and labelling of ingredients must uphold good standards as set by regulatory authorities in each country [8]. Postmarket DHSs regulations usually consist of market surveillance surrounding the products’ quality, efficacy, safety, and adverse events as reported by consumers [8]. If a DHS is found to be adulterated, misbranded, or harmful to consumer health, regulatory authorities will take appropriate action and may remove the product from the market [8]. Ideally, DHSs have both premarket and postmarket regulations, as is the case in countries such as Canada [11], while in countries such as the United States, only the latter exists [12]. In countries such as New Zealand, the United Kingdom, Japan, and Australia, only DHSs with therapeutic claims must adhere to both premarket and postmarket regulations, while those with non-therapeutic claims are only assessed through postmarket regulations [13,14,15,16].
Regardless of how DHSs are regulated, pharmacists are in a unique position to educate patients about the use, efficacy, side effects, and potential interactions with prescription medications associated with such products. An Australian survey found that 87–92% of consumers expected pharmacists to be able to provide adequate and reliable information about the safety and efficacy of DHSs [17]. Furthermore, a systematic review identified that pharmacists believe that they have the professional responsibility to counsel patients on the safe use of DHSs [18], and in some jurisdictions, pharmacists are already providing recommendations about DHSs to their patients frequently. A survey found that 40% of US pharmacists and 28.6% of UK pharmacists recommended multivitamins more than five times a week [19].
Knowing that pharmacists frequently offer DHSs advice to patients for a wide range of health conditions, it is critical for pharmacists to have a reasonable degree of knowledge about these products. Despite this necessity, multiple surveys have indicated that pharmacists have low knowledge of and confidence in the safety and efficacy of DHSs and drug-DHSs interactions [20, 21]. A preliminary literature search on this topic suggested that a need existed to explore the complexity of pharmacists’ experiences with DHSs and assess the context in which findings related to their practice in this area are situated. Therefore, the objective of this review was to identify the barriers, knowledge, and training that pharmacists report related to counselling on DHSs.
Methods
Approach
A qualitative systematic review was conducted to examine pharmacists’ knowledge of DHSs using standard methods [22] and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria [23]. A qualitative systematic review seeks to combine findings across multiple studies to understand the complexities of individuals’ experiences and perceptions, rather than assessing the effectiveness of an intervention [24, 25]. A protocol was not registered.
Eligibility criteria
Eligible studies reported qualitative data (e.g. qualitative surveys, interviews, focus groups, and observational studies) on pharmacists’ perceptions of their knowledge, training, and barriers related to counselling on DHSs. Mixed-methods studies that contained a qualitative component were also eligible, however, studies that contained solely quantitative data were ineligible. For the purpose of this study, we defined DHSs to include vitamins and minerals, herbal remedies, homeopathic medicines, traditional medicines such as traditional Chinese medicines, probiotics, amino acids, and essential fatty acids, which was based on published definitions of DHSs, similar products, or their synonyms [26,27,28,29]. Only English-language articles were included, and all studies not meeting the aforementioned eligibility criteria were excluded.
Searching and screening
MEDLINE, EMBASE, AMED and CINAHL were searched on May 11th, 2020 from inception to May 8th, 2020. JYN designed the search strategy (Table 1) to encompass both keywords and indexed headings related to DHSs, pharmacists, and qualitative research methods. UT and SD independently screened the titles and abstracts recovered from all four databases, independently and in duplicate. Any discrepancies were resolved through discussion between all three authors. The same process was undertaken for the full-text screening of eligible studies.
Data extraction
A data extraction form was created a priori to collect information from each eligible article. The following items were extracted and summarized: title of study; author; year published; country/countries of participants; term(s) used to describe DHS; regulatory status of the DHSs; types of DHSs included in the study; study methodologies; theoretical underpinnings; pharmacist type; number of participants; outcomes; themes discussed; main findings; challenges encountered by the study population; limitations to the study; and study conclusions. UT and SD independently extracted data and discrepancies were resolved through discussion with JYN.
Thematic analysis
Thematic analysis was conducted based on the data extracted from Table 2 and Table 3, which included the themes, main findings, challenges encountered, limitations and conclusions. The available qualitative data was first summarized in tables and then analyzed by all three authors. UT and SD interpreted the evidence from the included papers to identify common key concepts. JYN, UT, and SD used words and phrases that captured key concepts to create codes, thematically organized codes into groups, and presented a discussion based on the research question as well as highlighted knowledge gaps in the currently published literature. Any disagreements were resolved through discussion.
Results
Search results
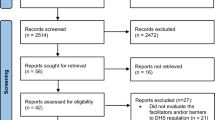
Searches identified a total of 1695 items, of which 1385 were unique, and 1272 titles and abstracts were eliminated, leaving 113 full-text articles for further review. Of those, 94 were deemed ineligible, because they did not include qualitative data (n = 89), were conference abstracts (n = 3) or were irretrievable (n = 2), leaving a total of 19 articles that were included in this qualitative systematic review [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. A PRISMA diagram can be found in Fig. 1.
Characteristics of included studies
As shown in Table 2, eligible articles were published from 2004 to 2020 and originated from 12 countries. The largest number of studies originated from the United States (n = 4). Most studies’ pharmacists practiced in a jurisdiction where regulations on DHSs existed but were limited (n = 7). Although many terms were used to describe dietary and herbal supplements (DHSs), the most common included natural health products (n = 3), dietary supplements (n = 3), and complementary and alternative medicine (n = 3). The most common research method used across eligible articles was the qualitative interview (n = 28). Most studies’ participants consisted of only community pharmacists (n = 15). The details associated with all eligible article characteristics can be found in Table 2.
Findings from thematic analysis
In total, three main themes emerged from our analysis and are described below.
Theme 1: challenges to DHS education
Many studies found that pharmacists’ education fell short of providing them with a thorough understanding of DHSs [30, 31, 33, 34, 37, 39, 41,42,43]. While some pharmacists expressed that they lacked a DHS education component in their pharmacy curricula [32, 35, 43], those that did receive training stated that they were not confident about their DHS knowledge [42, 43]. Furthermore, the pharmacists suggested that recent graduates may have less knowledge on this topic due to reduced DHS content in the curriculum [42, 43]. Pharmacists described that they were conscious of their poor knowledge and awareness of DHSs, including their safety, efficacy, and drug-DHS interactions [30, 35,36,37,38, 43, 46]. Others reported that much of their limited knowledge came from word-of-mouth and the media [38]. This lack of DHSs knowledge decreased pharmacists’ willingness to counsel patients on certain products, such as probiotics [37,38,39,40, 42, 43, 45]. Many pharmacists agreed with the need for continuing education surrounding DHSs and suggested more DHS curriculum should be incorporated into their university training [30, 32, 34, 35, 37, 40, 45].
Theme 2: post-graduation workplace challenges
Sub-theme 2.1: DHS training and resources in the workplace
Following graduation, pharmacists also expressed that DHS training in the workplace was inadequate, which was a factor that added to their lack of DHS knowledge [36, 38, 40, 44]. One study noted that many of the pharmacists interviewed had received no formal training on DHSs in the pharmacy and had been introduced to only some herbal medicines [38]. Pharmacists have expressed their desire for increased DHS training in order to gain a comprehensive understanding of these products and to provide better counselling to inquiring patients [31, 38, 40]. Additionally, the lack of reliable information about DHSs was a key contributing factor to pharmacists’ hesitation to counsel patients interested in DHSs [31, 35, 39, 40]. Pharmacists stated that they used evidence-based information to assess the risk-benefits of pharmaceutical medications and similarly require such information for DHSs, particularly with regards to safety and efficacy, in order to effectively counsel their patients [30, 33, 36, 41, 46, 48]. Some also indicated that because of the lack of information, their knowledge about such resources came from media sources, including advertisements [38]. To combat this lack of training, some pharmacists suggested the development of a readily accessible online database for providing information on DHSs [32, 36].
Sub-theme 2.2: lack of time to counsel about DHSs
Pharmacists voiced that the limited time available for patient counselling surrounding over the counter (OTC) products obstructed proper pharmacist-patient communication [40, 42]. Due to time constraints, pharmacists were concerned about the extent of the information they could relay, as well as the time they required to investigate the suitability of various DHSs [33, 47]. As a result of limited time constraints, pharmacists tended to refer patients to alternative healthcare practitioners or answer patient queries briefly, as opposed to providing comprehensive information surrounding these products [42, 47].
Sub-theme 2.3: limited DHSs regulations
Pharmacists expressed their concerns regarding the limited DHS regulations and framework, which they had identified as a barrier when providing patients with information about such products [28, 30, 34, 35, 39, 41, 47]. In some countries, there are no requirements regarding whether a pharmacy should or should not sell DHSs [34]. Many pharmacists lacked knowledge about the regulations in their country of practice, which they had identified as a barrier to stocking DHSs in their pharmacy [33, 38]. Moreover, in contrast to traditional OTC pharmaceutical medications, limited regulations surrounding DHSs were a reason why pharmacists lacked the confidence to advise their patients about DHSs [32, 33, 41]. Similarly, these limited regulations lead some pharmacists to believe that these products are unsafe for use, and furthered their reluctance to recommend them to patients [48]. Furthermore, pharmacists suggested that regulations were lacking with respect to their role in dispensing DHSs, and called for regulatory and policy support [31, 39, 47].
Theme 3: perceived role and importance of DHSs
Sub-theme 3.1: ambiguity in pharmacists’ professional roles
Due to a lack of education and training on DHSs, pharmacists were often unsure of their professional roles and responsibilities surrounding DHSs [33, 36, 40, 43, 47]. Some pharmacists understood that their role should involve providing adequate counselling, accurate information about products safety/efficacy, and recommending DHSs when appropriate [40, 47]. However, pharmacists’ lack of structured roles surrounding DHSs has affected their ability to assess the quality of counselling they provide to patients about these products [47]. Structure regarding how pharmacists should approach DHSs in their professional role is largely unknown, which makes it difficult for pharmacists to promote DHSs and advise patients on these products [40, 43, 47]. Pharmacists proposed that additional clarification on their role be provided to ensure a thorough understanding of their responsibilities pertaining to DHSs [40, 43, 47].
Sub-theme 3.2: perceived importance of DHSs
Many pharmacists perceived DHSs to be important [32, 38, 43, 45], and some even perceived DHSs to be as important as pharmaceutical medicine and vital to pharmacy practice [38, 43]. Some pharmacists suggested that their understanding of DHS importance stems from customer interactions, as they had expressed their desire for DHS use [45]. Furthermore, pharmacists have appeared to understand and empathize with customers’ demand for DHSs for their children, as they recognized that parents often seek alternative therapies for their children due to their own previous, negative experiences with pharmaceutical medications [45].
Discussion
A total of 19 studies were deemed eligible and included in this review. An analysis of these studies identified the following themes: challenges to DHS education; post-graduation workplace challenges surrounding DHSs; and pharmacists’ perceived role and importance of DHSs. Findings from this review that may assist in improving pharmacists’ knowledge about DHSs and the safe usage of DHSs by patients is discussed below.
Comparative literature
Challenges to DHS education
Findings across the literature support that pharmacists’ education related to DHSs was limited or non-existent. An American cross-sectional survey found that there were notable differences among pharmacy students’ recollection of when they had been introduced to DHSs in their program, despite taking the same courses [49]. This highlights the lack of structure surrounding DHSs in pharmacy curricula. This same study identified that the university did not have a course dedicated to DHSs, and suggested incorporating DHSs in didactic teaching [49]. Furthermore, a Jordanian cross-sectional study found that none of the pharmacists surveyed indicated that they had received any guidelines on DHSs during their formal training period before graduation [50].
The lack of DHSs education provided to pharmacists is likely responsible for their poor knowledge of these products, including drug-DHS interactions. An American survey found that only 2.4% of pharmacists who received inquiries surrounding DHSs felt that they could always answer the questions [51]. Moreover, a cross-sectional survey drew parallels between Saudi Arabian pharmacists and American pharmacists, in which both exhibited a lack of awareness of drug-DHS interactions [52]. Similarly, another American cross-sectional survey found that 26.3% of pharmacists provided inappropriate advice surrounding drug-DHS interactions [53]. This percentage of inaccurate drug-DHS advice is a reflection of pharmacists’ poor understanding of this topic. Notably, this lack of knowledge may be due to the near absence of premarket clinical trials of DHSs. One study found that patients with chronic disease were at the greatest risk of experiencing drug-DHS interactions, and it was suggested that part of this risk was due to the lack of premarketing regulations requiring safety trials on drug-DHS interactions [54]. Our finding suggest that a course dedicated to DHSs in pharmacy education may be of value, as well as improved regulations that mandate premarket clinical data for DHSs to test for drug-DHS interactions. Furthermore, the implementation of mandatory pharmacy practicums may be beneficial, as a Canadian assessment of pharmacy students’ knowledge suggested that fourth-year students who had completed a pharmacy practicum performed better on a standardized test about DHSs [55].
Post-graduation workplace challenges
There have been various calls for improved workplace training to maintain an adequate standard of DHSs knowledge among all pharmacists [18]. A systematic review identified that pharmacists agree that continuing education on DHSs should be mandatory, and noted that topics such as adverse drug reactions (ADRs), patient counselling, therapeutic uses and dosing would be most beneficial to include in this training [18]. Not only is workplace training on DHS limited, but DHSs-specific resources also appear to be lacking. For example, an American cross-sectional survey found that many pharmacists were not satisfied with the resources available to them [47, 56]. Therefore, one of the reasons pharmacists may be unable to counsel patients on the safe use of DHSs, is because they lack the necessary information to do so. Another cross-sectional survey conducted in Saudi Arabia revealed that a major concern for pharmacists included a lack of scientific evidence that supported the use of DHSs [57]. To facilitate pharmacists’ acquisition of knowledge, DHS training and continuing education programs should be implemented; furthermore, they should have access to the most up-to-date clinical research findings surrounding DHSs.
Compounding this issue is the fact that pharmacists may lack the time to adequately counsel patients about DHSs. This finding is supported by a cross-sectional survey conducted in Saudi Arabia, which found that the most common barrier for pharmacists in providing DHS counselling to patients was a lack of time due to their other responsibilities [57]. Another study that interviewed pharmacists found that very few reported ADRs related to DHSs due to time constraints in the workplace [58]. Since a lack of time is an identified barrier to pharmacists counselling on DHSs or reporting DHS-related ADRs, the adjustment and re-evaluation of pharmacists’ assigned roles warrants further investigation.
The present review also identified that pharmacists were concerned over the limited regulations governing the sale of DHSs, which is another issue also supported by the peer-reviewed literature. A review of issues surrounding complementary and alternative medicine in the United States found that DHSs are not regulated nearly as strictly as pharmaceutical medications, specifically with respect to safety testing, efficacy, and marketing [59]. This is largely because, in the United States, the Food and Drug Administration does not require manufacturers to provide evidence that their DHSs are safe or effective before they are brought to market [18]. Additionally, an Australian survey examining barriers faced by pharmacists in providing complementary and alternative medicine information found that one of the main obstacles included a need for better DHSs regulations [60]. This same study specified that the need for better regulations included more rigorous standards for listing DHSs on the Australian Register of Therapeutic Goods, clearer information about the type of evaluation the DHS was subjected to, and improved labelling of warnings if product effectiveness was not established [60]. Interestingly, a cross-sectional survey found that American pharmacists were less confident in answering patient questions about DHSs when compared to health food store employees [21]. These feelings of hesitation and self-doubt might be attributed to the limited regulations on DHSs, specifically regarding the labelling. In 2015, the New York State attorney general’s office found that many DHSs sold by major retailers lacked the ingredients listed on the label or contained other substances not listed [61]. As a result, it is not unreasonable to infer that pharmacists working in community settings may have little confidence in the quality of such products. To restore pharmacists’ confidence in counselling about DHSs, policymakers, practitioners, and federal health agencies must collaborate to develop improved regulations that govern the sale, safety, and services of these products.
Pharmacists’ perceived role and importance of DHSs
The roles and responsibilities of pharmacists surrounding DHSs, along with standard DHS curricula and workplace knowledge requirements remain unclear across many jurisdictions [62]. This issue should be addressed and defined through clear regulations that define a pharmacist’s role and standards of knowledge surrounding DHSs should be included in pharmacy education so that trainees are aware of their future professional responsibilities. Despite the difficulties in acquiring DHS knowledge, pharmacists perceive such products to be important to their profession and their patients. An American study found that pharmacy students considered knowledge of DHSs to be very important [63]. Other studies have found that pharmacists viewed DHSs with importance and recognized the need for further continuing education and professional development opportunities surrounding DHSs [20, 40, 45].
Future directions for pharmacy education and training on DHSs
One future direction may include a collaboration between pharmacy associations and academic institutions, in order to encourage the development of guidelines that provide recommendations for DHSs curriculum, continuing education, and clinical practice. Based on the present review’s findings, it seems prudent that pharmacy students should be required to complete a course dedicated to the safety, efficacy, and regulations of DHSs within their professional training [49]. The Center for the Advancement of Pharmacy Education (CAPE) is an organization that has identified educational outcomes that should be considered when updating pharmacy curricula. CAPE has called for improved foundational knowledge and encouraged academic institutions to meet their suggested learning objectives in order to guide curricular revision and pharmacy programs [64]. To improve DHS knowledge and education through the re-evaluation and revision of pharmacy curricula, educational outcomes such as those provided by CAPE should be considered. Continuing professional development (CPD) programs such as those offered through the Canadian Pharmacists Association, specifically tailored towards DHSs may be useful in improving pharmacists’ knowledge of a variety of relevant topics, such as cannabis [65]. Finally, pharmacy educators need to be aware of the various web-based online resources and their quality, with respect to ADRs, dosing, and the side effects of DHSs, which have been previously summarized [66].
Strengths and limitations
Common limitations identified by authors of eligible studies
Many included studies reported that a small sample size was identified as a limitation [31,32,33, 36, 40, 43, 45, 46]. The heterogeneity of the participants, with respect to factors such as age, sex, and educational background was also identified as a limitation across some included studies [40,41,42], as well as the fact that most participants were community pharmacists [30, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. The geographic distribution of participants was another limitation; some of the studies were conducted in jurisdictions that may not be representative of all pharmacists’ experiences country-wide [31, 38, 42, 43]. To some extent, this review has helped to mitigate this bias, as we combined data from all eligible studies to identify the commonalities between pharmacists working in different regions of the world. Additionally, all but one study incorporated an interview component into their study design [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]; reliance on interview data is subject to its own biases which include the researcher misinterpreting participants’ responses, or inadvertently influencing the participant to respond in a particular way. For example, if the interviewer is also a pharmacist, this may influence a participant’s answer differently than if the interviewer was not a healthcare professional [46, 47].
Strengths and limitations of the present systematic review
One strength of this study included a comprehensive search of the literature across multiple academic databases. Additionally, our systematic review followed PRISMA guidelines, and screening, data extraction and thematic analysis was conducted in duplicate and reviewed by a third author. One limitation includes the fact that only English language publications were considered for inclusion. Additionally, a small number of articles were irretrievable, despite receiving assistance from our university librarian in placing interlibrary loan requests. Lastly, it should be noted that reviews conducted on topics such as DHSs are limited by the operational definition selected.
Conclusions
This review provides a summary of the barriers, knowledge, and training that pharmacists report related to counselling about DHSs. Our findings suggest that pharmacists lack general knowledge of DHSs, especially pertaining to drug-DHS interactions. Notably, this knowledge gap largely stems from limited pharmacy education and post-graduation training on DHSs, which decreased pharmacists’ confidence in providing counselling on DHSs and increased the ambiguity surrounding their professional role. Lack of reliable resources and time were among the most common barriers to counselling about DHSs. High-quality resources that provide safety and efficacy profiles of DHSs should be made easily accessible to pharmacists. Adjustment and re-evaluation of pharmacists’ assigned roles also warrants further investigation. Furthermore, there is a need to standardize the quantity and quality of DHS curriculum across pharmacy school programs, as well as workplace training and CPD programs surrounding DHSs. It is worthwhile to note that throughout this review, the topic of limited DHS regulations was frequently explored by the included studies and influenced many of the main findings, suggesting the need to further explore how the regulation of these products can be improved. Following the implementation of any of these recommendations, a future qualitative systematic review may serve useful in re-assess pharmacists’ experiences with respect to DHSs.
Availability of data and materials
All relevant data are included in this manuscript.
Abbreviations
- ADR:
-
Adverse drug reaction
- CAPE:
-
Center for the Advancement of Pharmacy Education
- CPD:
-
Continuing professional development
- DHS:
-
Dietary and herbal supplement
- OTC:
-
Over-the-counter
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
References
Burnett AJ, Livingstone KM, Woods JL, McNaughton SA. Dietary supplement use among Australian adults: findings from the 2011–2012 National Nutrition and physical activity survey. Nutrients. 2017;9(11):1248. https://doi.org/10.3390/nu9111248.
Kantor ED, Rehm CD, Du M, White E, Giovannucci EL. Trends in dietary supplement use among US adults from 1999–2012. JAMA. 2016;316(14):1464–74. https://doi.org/10.1001/jama.2016.14403.
Consumer Health Products Survey. TMS Canada; 2016. [cited 2021 Jan 7]. Available from: https://www.chpcanada.ca/wp-system/uploads/2017/12/Consumer-Health-Product-Survey.pdf.
Ng JY, Garber A, Luong M, Cooley K, Busse JW. No improvement in disclosure of natural health product use to primary care medical doctors in the last 15 years: a survey of naturopathic patients. Complement Ther Clin Pract. 2020;39:101106. https://doi.org/10.1016/j.ctcp.2020.101106.
Levy I, Attias S, Ben-Arye E, Schiff E. Use and safety of dietary and herbal supplements among hospitalized patients: what have we learned and what can be learned?—a narrative review. Eur J Integr Med. 2017;16:39–45. https://doi.org/10.1016/j.eujim.2017.10.006.
Izzo AA, Hoon-Kim S, Radhakrishnan R, Williamson EM. A critical approach to evaluating clinical efficacy, adverse events and drug interactions of herbal remedies. Phytother Res. 2016;30(5):691–700. https://doi.org/10.1002/ptr.5591.
Yetley EA. Multivitamin and multimineral dietary supplements: definitions, characterization, bioavailability, and drug interactions. Am J Clin Nutr. 2007;85(1):269S–76S. https://doi.org/10.1093/ajcn/85.1.269S.
Job KM, Kiang TKL, Constance JE, Sherwin CMT, Enioutina EY. Herbal medicines: challenges in the modern world. Part 4. Canada and United States. Expert Rev Clin Pharmacol. 2016;9(12):1597–609. https://doi.org/10.1080/17512433.2016.1238762.
Teng L, Zu Q, Li G, Yu T, Job KM, Yang X, et al. Herbal medicines: challenges in the modern world. Part 3. China and Japan. Expert Rev Clin Pharmacol. 2016;9(9):1225–33. https://doi.org/10.1080/17512433.2016.1195263.
Barnes J, McLachlan AJ, Sherwin CM, Enioutina EY. Herbal medicines: challenges in the modern world. Part 1. Australia and New Zealand. Expert Rev Clin Pharmacol. 2016;9(7):905–15. https://doi.org/10.1586/17512433.2016.1171712.
About Natural Health Product Regulation in Canada. Government of Canada. 2004 [cited 2021 Jan 7]. Available from: https://www.canada.ca/en/health-canada/services/drugs-health-products/natural-non-prescription/regulation.html
Dietary Supplements. U.S. Food and Drug Administration. FDA; 2020 [cited 2021 Jan 7]. Available from: https://www.fda.gov/food/dietary-supplements
Complementary and Alternative Health Care in New Zealand [Internet]. Ministry of Health NZ. [cited 2021 Jan 7]. Available from: https://www.health.govt.nz/publication/complementary-and-alternative-health-care-new-zealand-0
Food Supplements Regulations. HSIS. [cited 2021 Jan 7]. Available from: https://www.hsis.org/food-supplements-regulations/
Tanaka H, Kaneda F, Suguro R, Baba H. Current system for regulation of health foods in Japan. JMAJ. 2004;47(9):436–50.
Regulation of complementary medicines in Australia. Therapeutic Goods Administration (TGA). Australian Government Department of Health; 2017 [cited 2021 Jan 7]. Available from: https://www.tga.gov.au/regulation-complementary-medicines-australia
Mehralian G, Yousefi N, Hashemian F, Maleksabet H. Knowledge, attitude and practice of pharmacists regarding dietary supplements: a community pharmacy- based survey in Tehran. Iran J Pharm Res IJPR. 2014;13(4):1457–65.
Kwan D, Hirschkorn K, Boon H. U.S. and Canadian pharmacists’ attitudes, knowledge, and professional practice behaviors toward dietary supplements: a systematic review. BMC Complement Altern Med. 2006;6:31. https://doi.org/10.1186/1472-6882-6-31.
Nelson MV, Bailie G. A survey of pharmacists recommendations for food supplements in the U.s.a. and U.k. J Clin Pharm Ther. 1990;15(2):131–9. https://doi.org/10.1111/j.1365-2710.1990.tb00367.x.
Hijazi MA, Shatila H, El-Lakany A, Ela MA, Kharroubi S, Alameddine M, et al. Beliefs, practices and knowledge of community pharmacists regarding complementary and alternative medicine: national cross-sectional study in Lebanon. BMJ Open. 2019;9(3):e025074. https://doi.org/10.1136/bmjopen-2018-025074.
Coon SA, Stevens VW, Brown JE, Wolff SE, Wrobel MJ. Comparison of dietary supplement product knowledge and confidence between pharmacists and health food store employees. J Am Pharm Assoc (2003). 2015;55(2):161–8. https://doi.org/10.1331/JAPhA.2015.14071.
Cochrane Handbook for Systematic Reviews of Interventions. [cited 2020 Aug 12]. Available from: https://training.cochrane.org/handbook/current
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care. Worldviews Evid-Based Nurs. 2016;13(3):241–9. https://doi.org/10.1111/wvn.12134.
Jørgensen CR, Thomsen TG, Ross L, Dietz SM, Therkildsen S, Groenvold M, et al. What facilitates “patient empowerment” in Cancer patients during follow-up: a qualitative systematic review of the literature. Qual Health Res. 2018;28(2):292–304. https://doi.org/10.1177/1049732317721477.
Administration AGD of HTG. An overview of the regulation of complementary medicines in Australia. Therapeutic Goods Administration (TGA). Australian Government Department of Health; 2013 [cited 2020 Aug 14]. Available from: https://www.tga.gov.au/overview-regulation-complementary-medicines-australia
Commissioner O of the. FDA 101: Dietary Supplements. FDA. FDA; 2019 [cited 2020 Aug 14]. Available from: https://www.fda.gov/consumers/consumer-updates/fda-101-dietary-supplements
Canada H. Natural health products. aem. 2004 [cited 2020 Aug 14]. Available from: https://www.canada.ca/en/health-canada/services/drugs-health-products/natural-non-prescription.html
WHO global report on traditional and complementary medicine, 2019. Geneva: World Health Organization; 2019. 226.
Barnes J, Butler R. Community pharmacists’ professional practices for complementary medicines: a qualitative study in New Zealand. Int J Clin Pharm. 2020;42(4):1109–17. https://doi.org/10.1007/s11096-020-01093-2.
Yao D, Hu H, Harnett JE, Ung COL. Integrating traditional Chinese medicines into professional community pharmacy practice in China – key stakeholder perspectives. Eur J Integrative Med. 2020;34:101063. https://doi.org/10.1016/j.eujim.2020.101063.
Harnett JE, Ung COL, Hu H, Sultani M, Desselle SP. Advancing the pharmacist’s role in promoting the appropriate and safe use of dietary supplements. Complementary Therapies Med. 2019;44:174–81. https://doi.org/10.1016/j.ctim.2019.04.018.
Ung COL, Harnett JE, Hu H, Desselle SP. Barriers to pharmacists adopting professional responsibilities that support the appropriate and safe use of dietary supplements in the United States: perspectives of key stakeholders. Am J Health Syst Pharm. 2019;76(13):980–90. https://doi.org/10.1093/ajhp/zxz079.
Cavaco AM, Arslan M, Şar S. Informing the homeopathic practice for Turkish pharmacists: reviewing the example of Portuguese community pharmacies. Homeopathy. 2017;106(2):93–102. https://doi.org/10.1016/j.homp.2017.02.003.
Ung COL, Harnett J, Hu H. Development of a strategic model for integrating complementary medicines into professional pharmacy practice. Res Soc Adm Pharm. 2017;14(7):663–72. https://doi.org/10.1016/j.sapharm.2017.07.012.
Ung COL, Harnett J, Hu H. Key stakeholder perspectives on the barriers and solutions to pharmacy practice towards complementary medicines: an Australian experience. BMC Complement Altern Med. 2017;17(1):394. https://doi.org/10.1186/s12906-017-1899-5.
Amarauche CO. Assessing the awareness and knowledge on the use of probiotics by healthcare professionals in Nigeria. J Young Pharmacists. 2016;8(1):53–5. https://doi.org/10.5530/jyp.2016.1.12.
Kretchy IA, Okere HA, Osafo J, Afrane B, Sarkodie J, Debrah P. Perceptions of traditional, complementary and alternative medicine among conventional healthcare practitioners in Accra, Ghana: implications for integrative healthcare. J Integrative Med. 2016 Sep 1;14(5):380–8. https://doi.org/10.1016/S2095-4964(16)60273-X.
Kheir N, Gad HY, Abu-Yousef SE. Pharmacists’ knowledge and attitudes about natural health products: a mixed-methods study. Drug Healthc Patient Saf. 2014;6:7–14. https://doi.org/10.2147/DHPS.S57756.
Asahina Y, Hori S, Sawada Y. Community pharmacists’ attitudes relating to patients’ use of health products in Japan. Int J Clin Pharm. 2012;34(4):529–37. https://doi.org/10.1007/s11096-012-9640-4.
Simmons-Yon A, Roth MT, Vu M, Kavalieratos D, Weinberger M, Rao JK. Understanding pharmacists’ experiences with advice-giving in the community pharmacy setting: a focus group study. Patient Educ Couns. 2012;89(3):476–83. https://doi.org/10.1016/j.pec.2012.08.011.
Jordan MA, Foster K, Gandhi A, Mohebbi N, Tehrani L. Assessment of herbal weight loss supplement counseling provided to patients by pharmacists and nonpharmacists in community settings. J Am Pharm Assoc. 2011;51(4):499–509. https://doi.org/10.1331/japha.2011.09233.
Walji R, Boon H, Barnes J, Welsh S, Austin Z, Baker GR. Reporting natural health product related adverse drug reactions: is it the pharmacist’s responsibility? Int J Pharm Pract. 2011;19(6):383–91. https://doi.org/10.1111/j.2042-7174.2011.00150.x.
Cramer H, Shaw A, Wye L, Weiss M. Over-the-counter advice seeking about complementary and alternative medicines (CAM) in community pharmacies and health shops: an ethnographic study. Health Soc Care Community. 2010;18(1):41–50. https://doi.org/10.1111/j.1365-2524.2009.00877.x.
Robinson N, Lorenc A. Responding to patient demand: community pharmacists and herbal and nutritional products for children. Phytother Res. 2010;25(6):892–6. https://doi.org/10.1002/ptr.3357.
Sim SN, Levine M. a. H. an evaluation of pharmacist and health food store retailer’s knowledge regarding potential drug interactions associated with St. John’s wort. Can J Clin Pharmacol. 2010;17(1):e57–63.
Kanjanarach T, Krass I, Cumming RG. Exploratory study of factors influencing practice of pharmacists in Australia and Thailand with respect to dietary supplements and complementary medicines. Int J Pharm Pract. 2006;14(2):123–8. https://doi.org/10.1211/ijpp.14.2.0006.
Webb IC, Chatterton JE, Beyerstein BL. An investigation of pharmacists' and health food store employees' knowledge about and attitudes toward kava. Sci Review Alternative Med. 2004;8(2):11–19.
Shah B, Siganga W, Mallya U, Shah S. Pharmacy student perspectives on classroom education about herbal supplements. Am J Pharm Educ. 2005;69(5):102. https://doi.org/10.5688/aj6905102.
Shilbayeh SA. Exploring knowledge and attitudes towards counselling about vitamin supplements in Jordanian community pharmacies. Pharm Pract (Granada). 2011;9(4):242–51. https://doi.org/10.4321/s1886-36552011000400010.
Clauson KA, Mcqueen CE, Shields KM, Bryant PJ. Knowledge and attitudes of pharmacists in Missouri regarding natural products. Am J Pharm Educ. 2003;67(2):41. https://doi.org/10.5688/AJ670241.
Alkharfy KM. Community pharmacists’ knowledge, attitudes and practices towards herbal remedies in Riyadh, Saudi Arabia. East Mediterr Health J. 2010;16(9):988–93. https://doi.org/10.26719/2010.16.9.988.
Sarino LV, Dang KH, Dianat N, Djihanian H, Natanian N, Hudmon KS, et al. Drug interaction between oral contraceptives and St. John’s wort: appropriateness of advice received from community pharmacists and health food store clerks. JAPhA. 2007;47(1):42–7. https://doi.org/10.1331/1544-3191.47.1.42.sarino.
Gardiner P, Phillips RS, Shaughnessy AF. Herbal and dietary supplement-drug interactions in patients with chronic illnesses. AFP. 2008;77(1):73–8.
Johnson T, Boon H, Jurgens T, Austin Z, Moineddin R, Eccott L, et al. Canadian pharmacy Students' knowledge of herbal medicine. Am J Pharm Educ. 2008;72(4):75. https://doi.org/10.5688/aj720475.
Nathan JP, Cicero LA, Koumis T, Rosenberg JM, Feifer S, Maltz F. Availability of and attitudes toward resources on alternative medicine products in the community pharmacy setting. J Am Pharm Assoc. 2005 Nov 1;45(6):734–9. https://doi.org/10.1331/154434505774909715.
Al-Arifi MN. Availability and needs of herbal medicinal information resources at community pharmacy, Riyadh region, Saudi Arabia. Saudi Pharma J. 2013;21(4):351–60. https://doi.org/10.1016/j.jsps.2012.11.004.
Green CF, Mottram DR, Raval D, Proudlove C, Randall C. Community pharmacists’ attitudes to adverse drug reaction reporting. Int J Pharm Pract. 1999;7(2):92–9. https://doi.org/10.1111/j.2042-7174.1999.tb00955.x.
C. Lee V. Current issues regarding complementary and alternative medicine (CAM) in the United States. P T 2010;35(9):514–522.
Semple SJ, Hotham E, Rao D, Martin K, Smith CA, Bloustien GF. Community pharmacists in Australia: barriers to information provision on complementary and alternative medicines. Pharm World Sci. 2006;28(6):366–73. https://doi.org/10.1007/s11096-006-9058-y.
O’Connor A. New York Attorney General Targets Supplements at Major Retailers. Well. 2015 [cited 2021 Jan 7]. Available from: https://well.blogs.nytimes.com/2015/02/03/new-york-attorney-general-targets-supplements-at-major-retailers/
Ung COL, Harnett J, Hu H. Community pharmacist’s responsibilities with regards to traditional medicine/complementary medicine products: a systematic literature review. Res Social Adm Pharm. 2017;13(4):686–716. https://doi.org/10.1016/j.sapharm.2016.08.001.
Axon DR, Vanova J, Edel C, Slack MK. Dietary supplement use, knowledge, and perceptions among student pharmacists. Am J Pharm Educ. 2017;81(5):92. https://doi.org/10.5688/ajpe81592.
Medina MS, Plaza CM, Stowe CD, Robinson ET, DeLander G, Beck DE, et al. Center for the Advancement of pharmacy education 2013 educational outcomes. AJPE. 2013;14(8):77(8). https://doi.org/10.5688/ajpe778162.
CPhA - CPD Programs - English. Canadian Pharmacists Association. [cited 2021 Jan 7]. Available from: https://www.pharmacists.ca/education-practice-resources/professional-development/
Ng JY, Munford V, Thakar H. Web-based online resources about adverse interactions or side effects associated with complementary and alternative medicine: a systematic review, summarization and quality assessment. BMC Med Informatics Decision Making. 2020;20(1):290. https://doi.org/10.1186/s12911-020-01298-5.
Acknowledgements
Not applicable.
Funding
JYN was awarded a Research Scholarship and an Entrance Scholarship from the Department of Health Research Methods, Evidence and Impact, Faculty of Health Sciences at McMaster University.
Author information
Authors and Affiliations
Contributions
JYN designed and conceptualized the study, collected and analysed data, critically revised the manuscript, and gave final approval of the version to be published. UT assisted with the collection and analysis of data, co-drafted the manuscript and gave final approval of the version to be published. SD assisted with the collection and analysis of data, co-drafted the manuscript, and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study involved a systematic review of peer-reviewed literature only; it did not require ethics approval or consent to participate.
Consent for publication
All authors consent to this manuscript’s publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ng, J.Y., Tahir, U. & Dhaliwal, S. Barriers, knowledge, and training related to pharmacists’ counselling on dietary and herbal supplements: a systematic review of qualitative studies. BMC Health Serv Res 21, 499 (2021). https://doi.org/10.1186/s12913-021-06502-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06502-4