Abstract
Background
Stroke is a leading cause of death and disability worldwide. A major factor in brain damage following ischemia is excitotoxicity caused by elevated levels of the neurotransmitter glutamate. In the brain, glutamate homeostasis is a primary function of astrocytes. Amburana cearensis has long been used in folk medicine and seed extract obtained with dichloromethane (EDAC) have previously been shown to exhibit cytoprotective activity in vitro. The aim of the present study was to analyse the activity of EDAC in hippocampal brain slices.
Methods
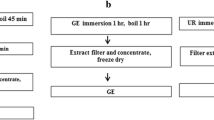
We prepared a dichloromethane extract (EDAC) from A. cearensis seeds and characterized the chemical constituents by 1H and 13C-NMR. Hippocampal slices from P6-8 or P90 Wistar rats were used for cell viability assay or glutamate uptake test. Hippocampal slices from P10-12 transgenic mice SOX10-EGFP and GFAP-EGFP and immunofluorescence for GS, GLAST and GLT1 were used to study oligodendrocytes and astrocytes.
Results
Astrocytes play a critical role in glutamate homeostasis and we provide immunohistochemical evidence that in excitotoxicity EDAC increased expression of glutamate transporters and glutamine synthetase, which is essential for detoxifying glutamate. Next, we directly examined astrocytes using transgenic mice in which glial fibrillary acidic protein (GFAP) drives expression of enhanced green fluorescence protein (EGFP) and show that glutamate excitotoxicity caused a decrease in GFAP-EGFP and that EDAC protected against this loss. This was examined further in the oxygen–glucose deprivation (OGD) model of ischemia, where EDAC caused an increase in astrocytic process branching, resulting in an increase in GFAP-EGFP. Using SOX10-EGFP reporter mice, we show that the acute response of oligodendrocytes to OGD in hippocampal slices is a marked loss of their processes and EDAC protected oligodendrocytes against this damage.
Conclusion
This study provides evidence that EDAC is cytoprotective against ischemia and glutamate excitotoxicity by modulating astrocyte responses and stimulating their glutamate homeostatic mechanisms.
Similar content being viewed by others
Background
The plant Amburana cearensis (Allemao) A.C. Sm. is used traditionally as tea, decoct and syrup for the treatment of various ailments, including headache, migraine and inflammation [1,2,3]. Previous work by our group has demonstrated neuroprotective effects against glutamate-mediated excitotoxicity in PC12 cells and primary cultures of cerebellar cells of the dichloromethane extract of A. cearensis seeds (EDAC) containing coumarin, ethyl ester, methyl esters and γ -sitosterol [4, 5]. Additionally, Amburoside A, a glucoside from A. cearensis trunk bark, has been shown to exhibit antioxidative and neuroprotective effects against 6-OHDA toxicity in rat mesencephalic cell cultures [6]. Together, these studies support the cytoprotective potential of compounds from A. cearensis in the CNS, but their effects on glial cells in brain tissues were unresolved.
Astrocytes and oligodendrocytes are the main glial cell types in the CNS. Oligodendrocytes are specialised to myelinate axons and are essential for the rapid conduction of neural impulses. Notably, oligodendrocytes are one of the most affected brain cells in ischemia, which results in devastating effects on CNS function [7,8,9,10]. For example, oligodendrocytes in the hippocampus are damaged following transient focal cerebral ischemia [11], and have been shown to be highly susceptible to oxygen–glucose deprivation (OGD), a model of ischemia-hypoxia that involves glutamate excitotoxicity [12,13,14]. Glutamate homeostasis is a primary function of astrocytes and they have been shown to protect oligodendrocytes following hypoxia and reperfusion-induced damage by uptake of excess glutamate [15, 16]. Astrocytes respond to glutamate excitotoxicity in a complex spatio-temporal manner that is highly context specific. Astrocyte pathological changes may be marked by a loss of processes and possibly cell death in acute phases and close to the lesion site [17]. At the other extreme, astrocytes may become hypertrophic, with increased glial fibrillary acidic protein (GFAP) and process branching [18, 14]. Since EDAC is cytoprotective for astrocytes and stimulates glutamate homeostasis, this led us to examine whether EDAC is also cytoprotective for oligodendrocytes in OGD in hippocampal slices from SOX10-EGFP mice, which enables us to visualise oligodendrocytes and their processes (Fig. 7A) [8]. Hippocampal slices were maintained in OGN or OGD conditions and treated with DMSO vehicle in controls or 10 µg/ mL EDAC, which we show above is the most effective concentration for cytoprotection and stimulating glutamate homeostasis. After 60 min OGN or OGD, slices were analysed for the total number of SOX10-EGFP + oligodendrocytes and counts of oligodendrocytes that were process-bearing compared to those that had lost their processes, which is an early indication of oligodendrocyte damage (Fig. 7A, insets). There was no significant difference in the total number of SOX10-EGFP + cells between the different treatment groups, indicating that oligodendrocytes survive acute OGD and that EDAC is non-toxic for these cells (Fig. 7A, B). In contrast, OGD resulted in a marked loss of processes in oligodendrocytes, with a significant decrease in process-bearing cells in all three strata of the CA1 region, compared to OGN, with 50% less in the stratum oriens, and 70% less in the strata pyramidale and radiatum (Fig. 7A, C; p values indicated on the graph). Treatment with EDAC protected oligodendrocytes against this damage in response to OGD (Fig. 7A), and the percentage of process-bearing SOX10-EGFP+ cells was not significantly different than OGN controls throughout the CA1 strata (Fig. 7C); EDAC appeared to most effective in stratum radiatum where the proportion of process-bearing oligodendrocytes in EDAC (54.9 ± 22%) was significantly greater (p < 0.05) than in OGD (26 ± 3.4%) (Fig. 7C). The results indicate that EDAC protect oligodendrocytes from OGD-induced acute cellular damage.
EDAC is cytoprotective for oligodendrocytes in OGD in hippocampal slices. Hippocampal slices from P10-12 SOX10-EGFP mice were incubated in aCSF for 1 h in OGN (normal oxygen + glucose) or OGD (no oxygen or glucose), with EDAC (10 mg/mL), or DMSO vehicle in controls (as indicated). A Representative confocal images of the CA1 region of the hippocampus illustrating the effects of OGD and EDAC on SOX10-EGFP + oligodendrocytes (green) counterstained with Hoechst for cell nuclei (blue). Insets are high magnification z-stacks illustrating oligodendrocyte morphology, illustrating that in OGN oligodendrocytes appear normal with bright somata and numerous fine processes, which support myelin sheaths, whereas in OGD there is a marked loss of processes and somata appear dim, and EDAC protected oligodendrocytes against these effects of OGD. Scale bar 50 µm in main panels and 30 μm in insets. B, C Counts were performed of total SOX10-EGFP + cells (B) and process-bearing SOX10-EGFP + cells (C, expressed as % of total SOX10-EGFP + cells) in constant FOV in the CA1 strata (as indicated), and plotted as mean ± SEM (n = 4 for each treatment group). Data were tested for significance using Kruskal–Wallis test between the control and several samples with post-hoc Dunns Multiple Comparison or standardized with the Mann–Whitney test of variance between two groups; **p < 0.01 indicates comparisons with OGN control, and #p < 0.05 indicates comparison with OGD control
Discussion
A number of constituents in extracts obtained from seeds of Amburana cearensis have been shown to be protective against glutamate cytotoxicity in PC12 cells [5] and primary cultures of cerebellar cells [4]. Here, we examined the effect of dichloromethane extract of A. cearensis seeds (EDAC) in hippocampal slices. The key finding of this study is that EDAC is cytoprotective against glutamate excitotoxicity and ischemia ex vivo in hippocampus slice cultures by stimulating astrocyte glutamate homeostasis, as summarised in Fig. 8. Glutamate dyshomeostasis is a major factor in stroke and other pathologies, including AD and MS [13], and our results suggest the natural product EDAC could provide a potential adjunct therapy in these diseases.
Proposed model of the cytoprotective effects of EDAC. Extract obtained from Amburana cearensis seeds (EDAC) is protective against astrocytes and oligodendrocytes in oxygen–glucose deprivation (OGD) and glutamate excitotoxicity in CA1 region of hippocampal slices. The protective effect of EDAC is associated with stimulation of astrocyte increased glutamate homeostasis
Our NMR analysis verified that EDAC is rich in coumarin, which encompasses a class of benzopyrones (1,2-benzopyrones or 2H-1-benzopyran-2-ones) phytochemicals and their derivatives. There are over 1,300 subtypes of coumarin and its derivatives and they are known to have antioxidant, anti-inflammatory, anti-bacterial and anti-viral activity [31, 32]. The most recognized pharmacological activity of derivatives from synthetic coumarins is anticoagulant activity, via its VitK inhibitory actions, hence coumarin derivatives are already in use as treatment for stroke and other vascular diseases [33]. Previously, metabolite profiling by Pereira and colleagues [5] using gas chromatography and mass spectrometry found that EDAC is composed of coumarin, methyl esters, γ-sitosterol and ethyl hexadecanoate. Our NMR analysis shows that coumarin is the main constituent of EDAC, comprising approximately one-third of the extract, and the recognised anti-oxidant properties of coumarin are likely to play a key role in the cytoprotective effects of EDAC demonstrated in the present study. Nonetheless, other components of EDAC may also play an important role, and two of them, methyl hexadecanoate and γ-sitosterol, have relevant pharmacological potential in the CNS. For example, methyl hexadecanoate has been shown to improve neuronal survival in the CA1 region of the hippocampus, as well as recovery of learning and memory, in a rat model of global cerebral ischemia [34], and γ-sitosterol was identified in neuroprotective terpenoid-rich extracts from orange juice [35]. Further studies are required to unravel the relative contributions of EDAC constituents to cytoprotection in the CNS, and although it is likely that coumarin is of major importance in the effects observed in the present study, an exciting possibility is that the multiple compounds in EDAC have combinatorial or even synergistic effects.
Due to its maintenance of cell–cell interactions and cytoarchitecture, hippocampal organotypic cultures exposed to glutamate excess have been widely used as an ex vivo model for bioprospection of neuroprotective compounds [21]. Additionally, the CA1 region of the hippocampus receptors is of clinical importance in neuropathology and is highly susceptible to glutamate due to the high density of glutamatergic neurons and NMDA receptors, which are strongly implicated in glutamate-mediated excitotoxicity [36, 37]. Here, we show that EDAC prevents cell death induced by cytotoxic levels of glutamate in hippocampal slices. We also demonstrate that EDAC stimulates astrocyte glutamate homeostatic mechanisms in the face of cytotoxic levels of glutamate. Astrocytes are the main detoxifying cells for excess glutamate, but they are also excited by activation of their NMDA and AMPA receptors [38], which can result in their damage by excess glutamate [39, 40]. In the present study, elevated glutamate induced an overall reduction in GFAP-EGFP in the hippocampus, indicating acute morphological disruption of astrocytes and cell loss, consistent with other studies [17]. Notably, the cytotoxic effect of glutamate on astrocytes was completely overturned by treatment with EDAC, which increased the morphological complexity and overall GFAP-EGFP fluorescence, and an equivalent effect of EDAC was observed in ischemia. Hence, the primary action of EDAC on astrocytes was to protect against cellular atrophy, which is generally associated with downregulation of glutamate transporters and GS and contributes to neuronal and oligodendrocyte demise [13]. GS is pivotal for depleting high levels of glutamate in astrocytes and its upregulation in astrocytes is an important mechanism for neuroprotection against glutamate-mediated excitotoxicity in vitro [20, 21] and in vivo [41]. Here, in addition to a marked increase of GS, we observed increases in glutamate transporters GLT-1 and GLAST in hippocampal organotypic slices treated with EDAC in excitotoxic glutamate. These transporters are expressed by morphologically distinct GFAP astrocytes [42], and their up regulation has been suggested as a neuroprotective mechanism of action for natural compounds against glutamate excitotoxicity [20, 21]. The increased of GFAP, GLT1, GLAST, and GS observed in the slices treated with EDAC + glutamate was associated with an increased number of GFAP-positive cells, which strongly suggests the astrocytes activation as the potential mechanism of EDAC protective effect.
Additionally, the increase in astrocyte processes induced by EDAC reflects greater coverage in the hippocampus and combined with enhanced glutamate homeostasis is a primary mechanism of EDAC cytoprotective activity in high glutamate, applied experimentally or in response to ischemia. Significantly, we show that EDAC also protects oligodendrocytes against ischemia. Oligodendrocyte viability and myelination are disrupted in ischemic stroke [43]. It has previously been shown that OGD induces the loss of oligodendrocyte processes which is mediated by glutamate excitotoxicity and precedes cellular death [14], and similar morphological changes in response to ischemia have been shown in oligodendrocyte precursors [44]. In the present study, we demonstrate OGD induced morphological atrophy in oligodendrocytes in the hippocampus and EDAC significantly protected oligodendroglial cells against these acute responses to ischemia. However, EDAC was not completely cytoprotective for oligodendrocytes, which is consistent with acute ischemic damage to these cells involving multiple mechanisms besides glutamate, including raised extracellular ATP and activation of P2X7 receptors [13, 45].
Conclusion
In conclusion, EDAC protects the hippocampus from glutamate excitotoxicity and ischemia. An important cytoprotective action of EDAC is to preserve astrocyte and oligodendrocyte integrity by stimulating glutamate homeostatic mechanisms. The results demonstrate EDAC is neuroprotective and support the need for further detailed analyses of the mechanisms underlying its biological effects in complex systems.
Availability of data and materials
The authors confirm that the data from which the findings of this study are derived are available within the article.
Abbreviations
- AMPA:
-
α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- SOX10:
-
SRY-Box Transcription Factor 10
- EGFP:
-
Green fluorescent protein
- GFAP:
-
Glial fibrillary acidic protein
- GS:
-
Glutamine synthetase
- GLAST:
-
Glutamate-aspartate transporter
- GLT1:
-
Glutamate transporter 1
- NMR:
-
Nuclear magnetic resonance
- CNS:
-
Central Nervus System
- DCM:
-
Dichloromethane
- PI:
-
Propidium iodide
- ATP:
-
Adenosine triphosphate
- NMDA:
-
N-methyl D-aspartate
References
Silva JH, Ferreira RS, Pereira EP, Braga-de-Souza S, Almeida MM, Santos CC, et al. Amburana cearensis: Pharmacological and neuroprotective effects of its compounds. Molecules. 2020;25:3394.
Paniagua Zambrana NY, Bussmann RW, Hart RE, Moya Huanca AL, Ortiz Soria G, Ortiz Vaca M, et al. Traditional knowledge hiding in plain sight - twenty-first century ethnobotany of the Chácobo in Beni. Bolivia J Ethnobiol Ethnomed. 2017;13:57.
Garcia D, Domingues MV, Rodrigues E. Ethnopharmacological survey among migrants living in the Southeast Atlantic forest of Diadema, São Paulo, Brazil. J Ethnobiol Ethnomed. 2010;6:29.
Lima Pereira ÉP, Santos Souza C, Amparo J, Short Ferreira R, Nuñez-Figueredo Y, Gonzaga Fernandez L, et al. Amburana cearensis seed extract protects brain mitochondria from oxidative stress and cerebellar cells from excitotoxicity induced by glutamate. J Ethnopharmacol. 2017;209:157.
Pereira EPL, Braga-de-Souza S, Santos CC, Santos LO, Cerqueira MD, Ribeiro PR, et al. Amburana cearensis seed extracts protect PC-12 cells against toxicity induced by glutamate. Rev Bras Farmacogn. 2017;27:199–205.
Leal LKAM, Nobre Junior HV, Cunha GMA, Moraes MO, Pessoa C, Oliveira RA, et al. Amburoside A, a glucoside from amburanacearensis, protects mesencephalic cells against 6-hydroxydopamine-induced neurotoxicity. Neurosci Lett. 2005;388:86–90.
Baltan S, Besancon EF, Mbow B, Ye ZC, Hamner MA, Ransom BR. White matter vulnerability to ischemic injury increases with age because of enhanced excitotoxicity. J Neurosci. 2008;28:1479–89.
Butt AM, Vanzulli I, Papanikolaou M, De La Rocha IC, Hawkins VE. Metabotropic glutamate receptors protect oligodendrocytes from acute ischemia in the mouse optic nerve. Neurochem Res. 2017;42:2468–78.
Ransom BR, Waxman SG, Davis PK. Anoxic injury of CNS white matter: Protective effect of ketamine. Neurology. 1990;40:1399–403.
Tekkök SB, Ye Z, Ransom BR. Excitotoxic mechanisms of ischemic injury in myelinated white matter. J Cereb Blood Flow Metab. 2007;27:1540–52.
Uchida H, Fujita Y, Matsueda M, Umeda M, Matsuda S, Kato H, et al. Damage to neurons and oligodendrocytes in the hippocampal CA1 sector after transient focal ischemia in rats. Cell Mol Neurobiol. 2010;30:1125–34.
Fern R, Möller T. Rapid ischemic cell death in immature oligodendrocytes: a fatal glutamate release feedback loop. J Neurosci. 2000;20:34–42.
Fern RF, Matute C, Stys PK. White matter injury: Ischemic and nonischemic. Glia. 2014;62:1780–9.
Salter MG, Fern R. NMDA receptors are expressed in develo** oligodendrocyte processes and mediate injury. Nature. 2005;438:1167–71.
Kato S, Aoyama M, Kakita H, Hida H, Kato I, Ito T, et al. Endogenous erythropoietin from astrocyte protects the oligodendrocyte precursor cell against hypoxic and reoxygenation injury. J Neurosci Res. 2011;89:1566–74.
Tognatta R, Karl MT, Fyffe-Maricich SL, Popratiloff A, Garrison ED, Schenck JK, et al. Astrocytes are required for oligodendrocyte survival and maintenance of myelin compaction and integrity. Front Cell Neurosci. 2020;14:74.
Shannon C, Salter M, Fern R. GFP imaging of live astrocytes: Regional differences in the effects of ischaemia upon astrocytes. J Anat. 2007;210:684–92.
Escartin C, Galea E, Lakatos A, O’Callaghan JP, Petzold GC, Serrano-Pozo A, et al. Reactive astrocyte nomenclature, definitions, and future directions. Nat Neurosci. 2021;24:312–25.
Shen Y, Lu H, Xu R, Tian H, **a X, Zhou FH, et al. The expression of GLAST and GLT1 in a transient cerebral ischemia Mongolian gerbil model. Neuropsychiatr Dis Treat. 2020;16:789–800.
dos Santos Souza C, Grangeiro MS, Lima Pereira EP, dos Santos CC, da Silva AB, Sampaio GP, et al. Agathisflavone, a flavonoid derived from Poincianella pyramidalis (Tul.), enhances neuronal population and protects against glutamate excitotoxicity. Neurotoxicology. 2018;65:85.
Ferreira RS, Teles-Souza J, dos Santos SC, Pereira ÉPL, de Araújo FM, da Silva AB, et al. Rutin improves glutamate uptake and inhibits glutamate excitotoxicity in rat brain slices. Mol Biol Rep. 2021;48:1475–83.
Nolte C, Matyash M, Pivneva T, Schipke CG, Ohlemeyer C, Hanisch UK, et al. GFAP promoter-controlled EGFP-expressing transgenic mice: a tool to visualize astrocytes and astrogliosis in living brain tissue. Glia. 2001;33:72–86.
Ribeiro PR, Teixeira R dos S, Souza AR, Pereira TCS, Boffo EF, Carosio MGA, et al. Blood plasma metabolomics of children and adolescents with sickle cell anaemia treated with hydroxycarbamide: a new tool for uncovering biochemical alterations. Br J Haematol. 2021;192:922–31.
Santos PM, Batista DLJ, Ribeiro LAF, Boffo EF, de Cerqueira MD, Martins D, et al. Identification of antioxidant and antimicrobial compounds from the oilseed crop Ricinus communis using a multiplatform metabolite profiling approach. Ind Crops Prod. 2018;124:834–44.
Stoppini L, Buchs P-A, Muller D. A simple method for organotypic cultures of nervous tissue. J Neurosci Methods. 1991;37:173–82.
AU - Young K, AU - Morrison H. Quantifying microglia morphology from photomicrographs of immunohistochemistry prepared tissue using imageJ. J Vis Exp. 2018;e57648.
Wishart DS, Knox C, Guo AC, Eisner R, Young N, Gautam B, et al. HMDB: a knowledgebase for the human metabolome. Nucleic Acids Res. 2009;37 suppl_1:D603–10.
Hirayama Y, Koizumi S, Subbotin OA, Zakharov PI, Zagorevskii VA, Zykov DA. 13C NMR spectrum of coumarin. Chem Nat Compd. 1975;11:476–9.
Hol EM, Pekny M. Glial fibrillary acidic protein (GFAP) and the astrocyte intermediate filament system in diseases of the central nervous system. Curr Opin Cell Biol. 2015;32:121–30.
Cookson MR, Pentreath VW. Alterations in the glial fibrillary acidic protein content of primary astrocyte cultures for evaluation of glial cell toxicity. Toxicol Vitr. 1994;8:351–9.
Fylaktakidou K, Hadjipavlou-Litina D, Litinas K, Nicolaides D. Natural and synthetic coumarin derivatives with anti-inflammatory / antioxidant activities. Curr Pharm Des. 2005;10:3813–33.
Venugopala KN, Rashmi V, Odhav B. Review on natural coumarin lead compounds for their pharmacological activity. Biomed Res Int. 2013;2013 Table 1.
Wittkowsky AK. Warfarin and other coumarin derivatives: pharmacokinetics, pharmacodynamics, and drug interactions. Semin Vasc Med. 2003;3:221–30.
Lee RH, Ph D, Couto A, Possoit HE, Lerner FM, Chen P, et al. Against Cardiac Arrest. 2020;1–27.
Sánchez-Martínez JD, Alvarez-Rivera G, Gallego R, Fagundes MB, Valdés A, Mendiola JA, et al. Neuroprotective potential of terpenoid-rich extracts from orange juice by-products obtained by pressurized liquid extraction. Food Chem X. 2022;13:100242.
Bye CM, McDonald RJ. A specific role of hippocampal NMDA receptors and arc protein in rapid encoding of novel environmental representations and a more general long-term consolidation function. Front Behav Neurosci. 2019;13:8.
Lana D, Ugolini F, Giovannini MG. An overview on the differential interplay among neurons-astrocytes-microglia in CA1 and CA3 hippocampus in hypoxia/ischemia. Front Cell Neurosci. 2020;14.
Parpura V, Verkhratsky A. Homeostatic function of astrocytes: Ca(2+) and Na(+) signalling. Transl Neurosci. 2012;3:334–44.
Jayaram B, Khan RS, Kastin AJ, Hsuchou H, Wu X, Pan W. Protective role of astrocytic leptin signaling against excitotoxicity. J Mol Neurosci. 2013;49:523–30.
Vanzulli I, Butt AM. mGluR5 protect astrocytes from ischemic damage in postnatal CNS white matter. Cell Calcium. 2015;58:423–30.
Zhang W, Miao Y, Zhou S, Jiang J, Luo Q, Qiu Y. Neuroprotective effects of ischemic postconditioning on global brain ischemia in rats through upregulation of hippocampal glutamine synthetase. J Clin Neurosci Off J Neurosurg Soc Australas. 2011;18:685–9.
Perego C, Vanoni C, Bossi M, Massari S, Basudev H, Longhi R, et al. The GLT-1 and GLAST glutamate transporters are expressed on morphologically distinct astrocytes and regulated by neuronal activity in primary hippocampal cocultures. J Neurochem. 2000;75:1076–84.
Skoff RP, Bessert DA, Barks JDE, Song D, Cerghet M, Silverstein FS. Hypoxic–ischemic injury results in acute disruption of myelin gene expression and death of oligodendroglial precursors in neonatal mice. Int J Dev Neurosci. 2001;19:197–208.
Falahati S, Breu M, Waickman AT, Phillips AW, Arauz EJ, Snyder S, et al. Ischemia-induced neuroinflammation is associated with disrupted development of oligodendrocyte progenitors in a model of periventricular leukomalacia. Dev Neurosci. 2013;35:182–96.
Butt AM. ATP: A ubiquitous gliotransmitter integrating neuron-glial networks. Semin Cell Dev Biol. 2011;22:205–13.
Acknowledgements
We would like to thank Dr. Maria G.A. Carosio (UFSCAR) and Dr. Antonio G. Ferreira (UFSCAR) for the acquisition of the 1H and 13C NMR spectra and Oswaldo Cruz Foundation—Bahia (FIOCRUZ) for the use of the LEICA confocal microscope. We thank Miss Jéssica Teles for the astrocyte illustration in the graphical abstract. The authentification was performed by Dr Érica Patrícia Lima Pereira from our lab (Laboratory of Neurochemistry and Cell Biology at the Federal University of Bahia). We thank Dr Érica Patrícia Lima Pereira (Laboratory of Neurochemistry and Cell Biology at the Federal University of Bahia) for the authentication and formal identification of the Amburana cearensis material used in this study.
Statement for experimental research on Amburana cearensis
Seeds of Amburana cearensis were purchased from a general store in the city of Feira de Santana, Bahia, Brazil, and checked for authenticity by comparison with seeds deposited in the Herbarium of the Biology Institute of the Federal University of Bahia, with the number 13734. Formal identification and authentication of A. cearensis seeds was performed by Dr Érica Patrícia Lima Pereira (Laboratory of Neurochemistry and Cell Biology at the Federal University of Bahia). All methods with A. cearensis seeds were carried out in accordance with the guidelines and standards of the University of Bahia, under registration in the National System for the Management of Genetic Heritage and Associated Traditional Knowledge (SisGen) under the number A73B242.
Funding
This work was supported by the UK / Brazil interchange cooperation (Edital RCUK-CONFAP/FAPESB- Research Partnerships Call 2014) grant, by the Bahia State Research Foundation (FAPESB – Project Nº 2957/2013, RED0016/2013), Coordination of Personnel Improvement of Higher Level (CAPES, PGCI-Process No. 88881.117666/2016–01; PGCI—88887.146001/2017–00), National Council for Scientific and Technological Development (CNPQ E. Universal/2018—429127/2018–9), the BBSRC (AB, Grant Number BB/M029379/1), MRC (AB, Grant Number MR/ P025811/1) and MS Society of the UK (AB, FP Award Reference: 40). We thank Miss Jéssica Teles for astrocyte illustration in the graphical abstract.
Author information
Authors and Affiliations
Contributions
Design of the study: VS, SLC and AB; Data and statistical analysis: RSF, PRR, JHCS, JBH, MMAA, BCLF, GBA, CGS, LGF, MFDC, CGS, AL, AMA, JCFM, FP, ADR; Writing, proofreading, and editing: RSF, SBS, SLC, AB and VS. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Animal research in the University of Portsmouth, UK, was approved by the revised Animals (Scientific Procedures) Act 1986, and the University of Portsmouth Animal Welfare and Ethical Review Board (P93781054). Animal research in the University of Bahia, Brazil, was approved by the Ethics Committee on the Use of Animals (CEP-UFRGS, protocol number 20005) (Bahia, Brazil).
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure S1.
Chemicalcharacterization of Amburana cearensis extract (EDAC).
Additional file 2:
Supplementary Table S1. Characterization of coumarin chemical structure.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferreira, R.S., Ribeiro, P.R., Silva, J.H.C.e. et al. Amburana cearensis seed extract stimulates astrocyte glutamate homeostatic mechanisms in hippocampal brain slices and protects oligodendrocytes against ischemia. BMC Complement Med Ther 23, 154 (2023). https://doi.org/10.1186/s12906-023-03959-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-023-03959-0