Abstract
Background
Most of the head and neck cancers are time-critical and need urgent surgical treatment. Our unit is one of the departments in the region, at the forefront in treating head and neck cancers in Pakistan. We have continued treating these patients in the COVID-19 pandemic with certain modified protocols. The objective of this study is to share our experience and approach towards head and neck reconstruction during the COVID-19 pandemic.
Results
There were a total of 31 patients, 20 (64.5%) were males and 11 (35.4%) patients were females. The mean age of patients was 52 years. Patients presented with different pathologies, i.e. Squamous cell carcinoma n = 26 (83.8%), mucoepidermoid carcinoma n = 2 (6.4%), adenoid cystic carcinoma n = 2 (6.4%) and mucormycosis n = 1 (3%). The reconstruction was done with loco-regional flaps like temporalis muscle flap n = 12 (38.7%), Pectoralis major myocutaneous flap n = 8 (25.8%), supraclavicular artery flap n = 10 (32.2%) and combination of fore-head, temporalis major and cheek rotation flaps n = 1 (3%). Defects involved different regions like maxilla n = 11 (35.4%), buccal mucosa n = 6 (19.3%), tongue with floor of mouth n = 6 (19.3%), mandible n = 4 (12.9%), parotid gland, mastoid n = 3 (9.6%) and combination of defects n = 1 (3%). Metal reconstruction plate was used in 3 (9.6%) patients with mandibular defects. All flaps survived, with the maximum follow-up of 8 months and minimum follow-up of 6 months.
Conclusion
Pedicled flaps are proving as the workhorse for head and neck reconstruction in unique global health crisis. Vigilant use of proper PPE and adherence to the ethical principles proves to be the only shield that will benefit patients, HCW and health system.
Similar content being viewed by others
Introduction
Corona virus (COVID-19) was first reported in December 2019 in the city of Wuhan, China, and soon it was declared as a global pandemic by the World Health Organization in March 2020 [1]. At the end of March 2020, the COVID-19 outbreak was announced in Pakistan, all the elective procedures were discouraged to conserve the resources and strategically contain the COVID-19 spread following guidelines from centers for disease control and prevention (CDC) [2]. All the other urgent and emergency surgical procedures are modified to overcome the burden on the health system.
In our department, surgeries were limited to the treatment of trauma and aggressive cancers. The risks and benefits for the patient were thoroughly evaluated, kee** in mind the safety of health care workers involved in the peri-operative care.
The majority of patients presented to us with advanced cancers, being referred from peripheral hospitals. Such patients could not be further delayed because holding-up treatment would have deleterious impact on functional and aesthetic outcomes. These patients fell in tier 3a and 3b category (high-acuity surgery for malignancies of the upper aero-digestive tract, cutaneous melanoma and high-risk cutaneous squamous cell carcinoma with non-delayable reconstructions for most defects involving the upper aerodigestive tract) according to Centers for Medicare and Medicaid services (CMS) surgical guide lines [3].
Our team has been playing a leading role in head and neck reconstruction for the last 20 years in Pakistan. Micro-vascular free tissue transfer is considered standard of care in head and neck reconstruction [4].
Hence, micro-vascular free tissue transfer is often our first choice for head and neck reconstruction. Since the COVID-19 pandemic started with its unique challenging crisis, we have to modify our practice by taking a step down on the reconstructive ladder. In this paper, we are presenting our experience of head and neck reconstruction with loco-regional pedicled flaps, during the COVID-19 pandemic.
Material and methods
In a 3 months period from April 1st 2020 till July 1st 2020, 31 patients underwent reconstruction for post ablative head and neck defects who were included in the study. Loco-regional flaps were used in all patients. Two surgeons (head and neck surgeon and reconstructive plastic surgeon) and two assistants were involved in all cases. All patients were pre-operatively screened with PCR COVID-19 nasal swabs and high-resolution CT scan (HRCT) Chest. Only COVID-19 negative (screened with PCR and HRCT) patients were operated. Patients, in which these investigations were not done, like in emergency and life threatening situations, were considered COVID-19 positive and excluded from study. During surgery all the operating room staff was directed to use particulate respirator mask (e.g. N95), eye protective goggles/face shields, surgical disposable gowns and gloves. Duration of surgical exposure, outcomes in terms of flap loss, wounds' infection/dehiscence, and functional recovery were noted. In these procedures the involved staff COVID-19 status was checked with the PCR every 2 weeks. This is a retrospective study approved from the ethical committee (Reference: IRB# 300-1120-2020). An informed consent was taken from all the patients whose pictures were used for publication purposes.
Quality of life questionnaire (QOL Q)
In this study European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30) version 3 (the validated Taiwan Chinese version) was employed. [5, 6] Out of 31 patients only 8 patients took part in answering the questionnaire due to COVID-19 restrictions. Patients completed the EORTC QLQ-C30 after the surgery at 6 months follow-up. The scores of QLQ-C30 items were linearly transformed to 0–100 scales. All scales were calculated according to EORTC scoring manual. [7, 8] Higher scores on functioning scales represent better functional outcome and high scores for symptom scales correspond to higher problems or symptoms.
Results
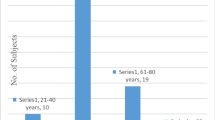
There were a total of 31 patients, 20 (64.5%) were males and 11 (35.4%) patients were females. The mean age of patients was 52 years. Patients presented with different pathologies, i.e. squamous cell carcinoma n = 26 (83.8%), mucoepidermoid carcinoma n = 2 (6.4%), adenoid cystic carcinoma n = 2 (6.4%) and mucormycosis n = 1 (3%). The reconstruction was done with loco-regional flaps like temporalis muscle flap n = 12 (38.7%), pectoralis major myocutaneous flap n = 8 (25.8%), supraclavicular artery flap n = 10 (32.2%) and combination of fore-head, temporalis major and cheek rotation flaps n = 1 (3%). Defects involved different regions like maxilla n = 11 (35.4%), buccal mucosa n = 6 (19.3%), tongue with floor of mouth n = 6 (19.3%), mandible n = 4 (12.9%), parotid gland, mastoid n = 3 (9.6%) and combination of defects n = 1 (3%). Metal reconstruction plate was used in 3 (9.6%) patients with mandibular defects. Patients evaluated clinically at follow-ups. All flaps survived, with the maximum follow-up of 8 months and minimum follow-up of 6 months. At 1 month follow-up, good mucosalization was seen in intraoral flaps. Minor wound dehiscence was seen in 4 (12.9%) patients who were conservatively managed. Mean operating time was 207 min with a range of 140 min to 347 min, (mean resection time 106 min, reconstruction time 101 min). Mean hospital stay was 3 days. Tracheostomy was done in 17 (54.8%) patients, which were removed on the 3rd post-operative day. None of the HCW involved in these cases was infected with COVID-19. Long term data is not available due to short follow-up course. Table 1 shows patients characteristics of our study.
EORTC QLQ-C30
Quality of life assessment using EORTC QLQ-C 30 in 8 patients is mentioned in Table 2. The mean global health status was 66.46. The functional scales values were high in social functioning, role functioning and emotional functioning representing in improvement of their overall function after treatment. The symptoms scales had low scores in most aspects except for pain (mean score 19.68), fatigue (mean score 24.39) and financial difficulties (mean score 45.75).
Following are our cases (Fig. 1. Case 1, Fig. 2. Case 2, Fig. 3. Case 3, Fig. 4. Case 4, Fig. 5. Case 5, Fig. 6. Case 6, Fig. 7. Case 7) showing the pre-operative pictures, per-operative pictures and their immediate follow-ups. Figure 8 shows patients after rehabilitation period of 6 months.
Case 1 a Young lady with large defect right cheek, nasal dorsum and palate with visible tongue at base. b Markings for forehead flap, temporalis muscle flap and cheek rotation advancement flaps. c Temporalis muscle flap inset done to reconstruct palate and fill the dead space. d Per-operative pic showing inset of forehead and cheek flaps. e Intra-oral view showing good mucosalization of temporalis muscle. f Frontal view of face at early follow up period
Case 2 a Case 2 Young male with recurrent Squamous cell carcinoma lower lip and mandible. There is a visible supraclavicular flap of previous surgery. b CT scan showing extent of tumor to bone and floor of mouth. c Per-operative view of wide local excision showing soft tissue and boney defect. d Per-operative view showing pectoralis major myocutaneous flap after inset and Karapandzic technique used for lip defect. e Early followup picture. f Frontal view of patient showing nicely healed wounds
Case 3 a Middle age male with large fungating mass of the left maxilla. b CT scan showing tumor invading maxillary bone and extending into palate. c Intra-operative picture showing large defect after wide local excision. d Early followup picture showing temporalis muscle at left palatal half. e Picture showing flap mucosalization at 4 weeks follow up. f Late follow up picture with good facial contours with mild temporal hollowing
Case 4 a Middle aged male with biopsy proven well differentiated squamous cell carcinoma of the left maxilla. b CT scan with contrast showing enhancement in the left maxilla sinus, left sided palate with destruction of the left maxillary arch. c Picture showing a moderate volume with large surface area defect after wide local excision of the tumor (subtotal maxillectomy) including resection of maxillary arch, palate and anterior and lateral walls with preservation of the orbital floor. d Four weeks follow up picture showing good mucosalisation of the temporal muscle flap. e Follow up CT scan of the patient showing temporalis muscle flap filling the defect. f Late follow up picture, patient has good facial contours with mild temporal hollowing
Case 5 a A young female patient presented with an ulcerative lesion of the right buccal mucosa, Biopsy reported well differentiated squamous cell carcinoma. b After resection of the tumor, An extended supraclavicular flap was elevated. c De-epithelialization of the proximal part of the flap was done, which was tunneled under the neck skin into the defect. d picture showing the flap inset into the defect and primary closure of the donor site. e, f 2 weeks follow up of the patient showing right sided cheek edema with good flap mucosalisation and good healing of the donor area
Case 6 a Patient with squamous cell carcinoma of body of the right mandible with left mandible extension with involvement of the floor of the mouth (T4a) b He had limited mouth opening with restricted tongue movements c Orthopantomogram (OPG) showing cortical destruction around the mandibular symphysis. d Enbloc Resected specimen showing mandibular arch with part of the floor of the mouth and bilateral neck nodes. e right lateral Xray view showing the reconstructed lower jaw with metallic reconstruction plate. f soft tissue coverage was provided with myocutaneous pectoralis major flap. Picture showing healed donor site
Case 7 a A young female patient presented with diagnosed case of adenoid cystic carcinoma of the right parotid with involvement of the middle ear b lateral view showing the extension of the tumor into the mastoid area. c Marking of the resection with 1 cm margins. d Excision involved peri-auricular skin, superficial parotidectomy, external and internal auditory meatus. Ear was intact by a bridge of skin at the root of the helix. e A supraclavicular artery flap was designed according to the defect size f Picture showing flap inset and donor site closure over a Redivac drain g Lateral view of patient at 1 month follow up
Discussion
The world has witnessed many global health challenges since the beginning of time. The COVID-19 also called as ‘’Severe acute respiratory syndrome 2 (SARS-2)’’ is one of special kinds that has some unique characteristics [8]. It is highly contagious, sprightly transmittable and has inherent stealth properties. The common mode of transmission is by direct human to human contact, aerosol generation, respiratory droplets, oro-fecal route and contaminated surfaces in our environment [9,40]. Even in some circumstances local pedicled flaps are preferred over free flaps, such as patients who cannot tolerate lengthy general anesthesia and with co-morbids [42]. In many circumstances regional flaps prove to be reliable and less expensive as compared to the free flaps [41].
Pectoralis major muscle flap has adequate bulk, and it easily adheres to irregular 3 dimensional defects. It can be used to wrap around metal recon plate to avoid plate extrusion and reconstruct the floor of the mouth. We have used it for coverage of chin defect, reconstructing the floor of mouth and enfolding the reconstruction plates. It provided as filling dead space and reliable soft tissue coverage.
For reconstruction of palate, buccal mucosa, retro-molar trigone and mastoidectomy defects, we have used Temporalis muscle flap, which provided adequate surface coverage and mucosalization was seen after 4 weeks in patients. The temporalis muscle flap is an all-round flap for craniofacial defects like orbit, the lateral base of the skull and oral cavity. This flap is advantageous because of the close vicinity and robust blood supply. Temporalis muscle flap is preferred in situations where free tissue transfer cannot be done [43].
Temporalis muscle flap has less donor site morbidity with hidden scar and no obvious functional deformity [44]. Tara Brennan et al. and Jesse E et al. showed very good results of temporalis muscle flap for reconstruction of palatal and tongue base defects. It has a high success rate and an outstanding alternative in the reconstruction of difficult intra-oral defects [45, 46]. In cases where a hair-free and less bulky flap is needed, temporalis muscle flap has superior results over the pectoralis major muscle flap [47].
In our patients where large buccal mucosa, cheek and floor of mouth defects were created, a supraclavicular artery flap was used. Although, it has some limitations in length, we didn’t experience any problem in distal flap circulation. It was first described by Lamberty in 1979 [48].
The supraclavicular artery flap provides large thin fascio-cutaneous coverage to most of the defects of the head and neck region [49]. This flap is easy to harvest and a good colour match if used for skin defects [50]. Super-charge of flap can be done if a large size flap is needed [51].
A combination of different flaps was used in one patient who presented to us with a large composite defect of cheek, maxilla, and nasal wall. She is a known case of Mucormyscosis, treated with multiple debridements. A forehead flap was used to reconstruct side of nose, cheek rotation flap used to cover cheek defect and temporalis muscle flap was used to reconstruct palate. She recovered well from the surgery. The temporalis flap had good mucosalization in fourth week.
Whenever there is need, always utilize a combination of flaps technique, which gives similar type of tissue readily available in the vicinity and scars / patches, can be hidden in facial aesthetic units.
In order to reduce duration of surgery, metal plate reconstruction of mandible is a favorable option. Three of our patients had mandibular (hemi-mandible n = 2, segmental n = 1, marginal n = 1) defects, in which metal reconstruction plates were used. These plates were enfolded with Pectoralis major muscle flaps to avoid extrusion. Saunders et al. in their study of 27 patients presented their success rates of 78–85% with metal reconstruction plate use. [52] Once this pandemic is over, in these patients at a later stage, vascularized free fibula reconstruction can be done.
Regarding chemo-radiotherapy treatment in such patients, critical specialized units should be designated with proper screening counters [53]. These patients are at higher risk of contracting the disease as they are immunocompromised, where possible telemedicine services should be utilized [54].
In disaster scenarios or health crises that we are facing today in 2020, we are forced to consider, a step down on the reconstructive ladder. The basic essence of our specialty is versatility and adaptability. There is no single best solution to any problem, but the circumstances define what is best at that moment in that particular case. The rapidly ongoing research and observation from across the world should be shared to enlighten the guidelines and experiences about the novel Corona Virus management and prevent complications.
The "resurrection" of local and regional flaps can prove to be a useful adjunct in the reconstruction of composite head and neck defects in current situation.
In this time of historical crisis we should be adherent to the ethical principles of utilitarianism, egalitarianism, fidelity, veracity and respect for people [55].
Conclusion
Pedicled flaps are proving as the workhorse for head and neck reconstruction in unique global health crisis. Vigilant use of proper PPE and adherence to the ethical principles proves to be the only shield that will benefit patients, HCW and health system. Routine methods must be mastered, but never let them master you. (The Principles and Art of Plastic Surgery).
Availability of data and materials
All data generated or analyzed during this study are included in this published article. Further information if needed can be requested from corresponding author.
References
World Health Organization. Coronavirus disease 2019 (COVID-2019) Situation Report-51. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10.
Coronavirus Disease 2019: For Healthcare Professionals. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html.
CMS Adult Elective Surgery and Procedures Recommendations. https://cms.gov/files/document/covid-elective-surgery-recommendations.pdf.
Wong CH, Wei FC. Microsurgical free flap in head and neck reconstruction. Head Neck. 2010;32(9):1236–45.
Chie WC, Hong RL, Lai CC, Ting LL, Hsu MM. Quality of life in patients of nasopharyngeal carcinoma: validation of the Taiwan Chinese version of the EORTC QLQ-C30 and the EORTC QLQ-H&N35. Qual Life Res. 2003;12(1):93–8.
Chie WC, Yang CH, Hsu C, Yang PC. Quality of life of lung cancer patients: validation of the Taiwan Chinese version of the EORTC QLQ-C30 and QLQ-LC13. Qual Life Res. 2004;13(1):257–62.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76.
Fayers PM, Aaronson NK, Bjordal K, Gronvold M, Curran D, Bottomley A. EORTC QLQ-C30 Scoring Manual; 2001.
Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2019. https://doi.org/10.1056/nejmoa2002032.
**ao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020. https://doi.org/10.1053/j.gastro.2020.02.055.
Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020. https://doi.org/10.1016/S2468-1253(20)30048-0.
Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020. https://doi.org/10.1080/22221751.2020.1729071.
Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020. https://doi.org/10.1001/jama.2020.3227.
Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020. https://doi.org/10.1056/nejmc2004973.
Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020. https://doi.org/10.1038/s41586-020-2196-x.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html.
Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, et al. False-negative results of initial RT-PCR assays for covid-19: a systematic review. MedRxiv. 2020;. https://doi.org/10.1101/2020.04.16.20066787.
Ioannis D, Selby K, Bernard P, Genton B, Cornuz J. Performance du frottis nasopharyngé-PCR pour le diagnostic du Covid-19 Recommandations pratiques sur la base des premières. 2020:699–701.
Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020. https://doi.org/10.1056/NEJMc2001737.
Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020. https://doi.org/10.1001/jama.2020.2565.
Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020. https://doi.org/10.1007/s12630-020-01591-x.
American College of Surgeons. COVID-19: elective case triage guidelines for surgical care. https://www.facs.org/covid-19/clinical-guidance/elective-case.
Tien HC, Chughtai T, Jogeklar A, Cooper AB, Brenneman F. Elective and emergency surgery in patients with severe acute respiratory syndrome (SARS). Can J Surg. 2005.
Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000003924.
Wenner L, Pauli U, Summermatter K, Gantenbein H, Vidondo B, Posthaus H. Aerosol generation during bone-sawing procedures in veterinary autopsies. Vet Pathol. 2017. https://doi.org/10.1177/0300985816688744.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
International Council of Nurses. High proportion of healthcare workers with COVID-19 in Italy is a stark warning to the world: protecting nurses and their colleagues must be the number one priority. https://www.icn.ch/sites/default/files/inline-files/PR_09_COVID-19-Italy.pdf.
"Closing Pakistan's Maternity Wards Puts Women at Risk". Human Rights Watch. 9 May 2020. Retrieved 10 May 2020.
American Society of Plastic Surgeons. ASPS Guidance Regarding Elective and Non-Essential Patient Care. http://email.plasticsurgery.org/q/12EC50dbrptNnCCaBimf8m0W/wv. Accessed 24 Apr 2020.
American Medical Association. AMA praises government on elective surgery guidelines during pandemic. https://www.ama-assn.org/press-center/ama-statements/ama-praises-government-elective-surgery-guidelines-during-pandemic. Accessed 24 Apr 2020.
Chaves A, Castro A, Marta G, et al. Emergency changes in international guidelines on treatment for head and neck cancer patients during the COVID-19 pandemic. Oral Oncol. 2020;107:1–3.
Galante E, Gallus G, Chiesa F, Bono A, Bettoni I, Molinari R. Growth rate of head and neck tumors. Eur J Cancer Clin Oncol. 1982;18(8):707–12.
Jensen AR, Nellemann HM, Overgaard J. Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol. 2007;84(1):5–10.
Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClin Med. 2020. https://doi.org/10.1016/j.eclinm.2020.100331.
Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–7. https://doi.org/10.1016/S1470-2045(20)30096-6.
Yu J, Ouyang W, Chua MLK, **e C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020. https://doi.org/10.1001/jamaoncol.2020.0980.
World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID19). https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf. Accessed 24 Apr 2020.
Wong C-H, Wei F-C. Microsurgical free flap in head and neck reconstruction. Head Neck. 2010. https://doi.org/10.1002/hed.21284.
Mahieu R, Colletti G, Bonomo P, Parrinello G, Iavarone A, Dolivet G, Livi L, Deganello A. Head and neck reconstruction with pedicled flaps in the free flap era
Ci G, Tewfik K, Bardazzi A, Allevi F, Chiapasco M, Mandalà M, Rabbiosi D. Regional flaps in head and neck reconstruction: a reappraisal. J Oral Maxillofac Surg. 2015. https://doi.org/10.1016/j.joms.2014.10.021.
Muyuan L, Weiwei L, **hong Y, Haipeng G, Hanwei P. Pectoralis major myocutaneous flap for head and neck defects in the era of free flaps: harvesting technique and indications.
Liliana E, Opeoluwa D, Elizabeth N. Temporalis muscle flap. Oper Tech Otolaryngol Head Neck Surg. 2019. https://doi.org/10.1016/j.otot.2019.04.006.
Hanasono MM, Utley DS, Goode RL. The temporalis muscle flap for reconstruction after head and neck oncologic surgery. Laryngoscope. 2001. https://doi.org/10.1097/00005537-200110000-00009.
Brennan T, Tham TM, Costantino P. The temporalis muscle flap for palate reconstruction: case series and review of the literature. Int Arch Otorhinolaryngol. 2017. https://doi.org/10.1055/s-0037-1598653.
Smith JE, Ducic Y, Adelson R. The utility of the temporalis muscle flap for oropharyngeal,base of tongue, and nasopharyngeal reconstruction Dallas and Fort Worth, Texas
Koranda FC, McMahon MF, Jernstrom VR. The temporalis muscle flap for intraoral reconstruction. Arch Otolaryngol Head Neck Surg. 1987;113(7):740–3. https://doi.org/10.1001/archotol.1987.01860070054015.
Lamberty BG. The supra-clavicular axial patterned flap. Br J Plast Surg. 1979;32:207–12.
Kokot N, Mazhar K, Reder LS, Peng GL, Sinha UK. The supraclavicular artery island flap in head and neck reconstruction applications and limitations. JAMA Otolaryngol Head Neck Surg. 2013;139(11):1247–55. https://doi.org/10.1001/jamaoto.2013.5057.
Shenoy A, et al. Supraclavicular artery flap for head and neck oncologic reconstruction: an emerging alternative. Int J Surg Oncol. 2013. https://doi.org/10.1155/2013/658989.
Atallah M-R, Alfalasi M, Ayad T. Supraclavicular flap for head and neck reconstruction.
Saunders JR, Hirata RM, Jaques DA. Definitive mandibular replacement using reconstruction plates. Am J Surg. 1990. https://doi.org/10.1016/s0002-9610(05)80549-5.
Sahu KK, **dal V, Siddiqui AD. Managing COVID-19 in patients with cancer: a double blow for oncologists.
**dal V, Sahu KK, Gaikazian S, Siddiqui AD, Jaiyesimi I. Cancer treatment during COVID-19 pandemic. Med Oncol. 2020;37:1–3.
American College of Surgeons: COVID-19 and surgery ethical considerations. https://www.facs.org/covid-19/ethics.
Acknowledgements
We want to thank all the patients and Health care workers who were involved in this research work. We had a continuous support from Medical staff affairs department Shifa International Hospital who made it possible for us to continue treating cancer patients during the COVID-19 Pandemic.
Funding
No funding received for this study.
Author information
Authors and Affiliations
Contributions
HUR and MR wrote the main manuscript text, NB and NK prepared figures. SSA has reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is approved from the Institutional review board and ethical committee of Shifa International Hospital Islamabad Pakistan (Reference: IRB# 300–1120-2020). Written informed consent was taken from all patients regarding participation in the study. Informed consent has been taken from patients regarding the use of their pictures and data for publication purposes in an open access journal and information sharing platforms.
Consent for publication
Written informed consent was obtained from the patients for publication of this study and any accompanying images.
Competing interests
There are no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rashid, H.U., Rashid, M., Khan, N. et al. Taking a step down on the reconstruction ladder for head and neck reconstruction during the COVID-19 pandemic. BMC Surg 21, 120 (2021). https://doi.org/10.1186/s12893-021-01134-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-021-01134-1