Abstract
Background
COPD is largely under-diagnosed and once diagnosed usually at a late stage. Early diagnosis is thoroughly recommended but most attempts failed as the disease is marginally known and screening marginally accepted. It is a rare cause of concern in primary care and spirometry is not very common. Exhaled carbon monoxide (eCO) is a 5-seconds easy-to-use device dedicated to monitor cigarette smoke consumption. We aimed to assess whether systematic eCO measurement in primary care is a useful tool to improve acceptance for early COPD diagnosis.
Methods
This was a two-center randomized controlled trial enrolling 410 patients between March and May, 2013. Whatever was the reason of attendance to the clinic, all adults were proposed to measure eCO during randomly chosen days and outcomes were compared between the two different groups of patients (performing and not performing eCO). Primary outcome was the rates of acceptance for COPD screening.
Results
Rate of acceptance for COPD screening was 28% in the eCO group and 26% in the other (P = 0.575). These rates increased to 48 and 51% in smokers (current and former). eCO significantly increased the rate of clinics during which a debate on smoking was initiated (42 vs. 24%, P = 0.001). eCO at 2.5 ppm was the discriminative concentration for identifying active smokers (ROC curve AUC: 0.935). Smoking was the only independent risk factor associated with acceptance for early COPD screening (OR = 364.6 (82.5-901.5) and OR = 78.5 (18.7-330.0) in current and former smokers, respectively) while eCO measurement was not.
Conclusions
Early COPD diagnosis is a minor cause of concern in primary care. Systematic eCO assessment failed to improve acceptance for early COPD screening.
Similar content being viewed by others
Background
Increasing concerns about Chronic obstructive pulmonary disease (COPD) are raised since it will be the fourth leading cause of deaths by 2030 [1]. Under diagnosis of COPD is a global problem, delaying adequate treatment and the possibility of preventing physical, emotional and socioeconomic consequences of the disease [2]. Multiple attempts aimed at diagnosing COPD earlier but to date none really penetrated the primary care in western countries. Early detection of COPD is crucial for promoting smoking cessation – which is more or less the unique way to interfere with the natural history of the disease. The under diagnosis of COPD is mostly related to spirometry pitfalls which included- but not restricted to-physicians- and patients-related factors. The reasons for general practitioners (GP) not performing spirometry might be limited access to the equipment, lack of adequate training and time constraints [2]. On the patients ‘side, under diagnosis may be a result of the gradual adaptation to increasing shortness of breath due to declining lung function and a reluctance to seek for medical advice before severe symptoms occur [3]. Moreover minor knowledge of the disease towards the general population leads to a non-discussion about shortness of breath: “Surrounding COPD is an historical nihilism, with patients and even their doctors establishing blame and blatantly denying a medical problem exists” was written in a review in 2009 [2]. Recently, the relative stability of the phenotype toward exacerbations rates identified a subgroup of COPD patients with a very low disease-related risk in terms of hospitalizations, exacerbation, accelerated decline in lung function or comorbidity [4,5]. This fact did not help for persuading GPs that early COPD diagnosis is a worth effort. Questionnaires have been developed and more or less successfully developed but the issue raised by most GPs associations dealt with an unacceptable number of questionnaires that might be applied routinely for most chronic diseases [6,7].
Assessing exhaled carbon monoxide (eCO) concentration is routinely used in tobacco weaning programs for up to fifteen years. It was shown as a valuable noninvasive biomarker of cigarette smoke daily consumption which passed through most validation studies. As it stands, eCO is a 5 or 10 seconds measurement that responds to most issues related to any tool: easy to do, no contraindication, no expertise requirement, absolute harmlessness, low cost [8].
As cigarette smoking remains the main cause of COPD in western countries, we hypothesized that assessing eCO in primary care will help GPs to improve awareness about COPD that will introduce acceptance for a COPD screening. We assumed that eCO assessment in waiting rooms will improve the debate on smoking and COPD during medical consultations.
Accordingly, we aimed to test this hypothesis in primary care through a two-center randomized controlled trial.
Methods
Study design and population
A prospective multicenter study was conducted in two outpatient primary care offices. All adult patients attending the outpatient clinic were consecutively included. The study was proposed to any patients who turned up at the clinics during the study period. Exclusion criteria were refusal to participate after information and age under 18 years old. Once attending the GP’s office, the investigator presented the study and gathered the non opposition approval. In the waiting room, a junior doctor (not the GP) fulfilled the Case Report Form (CRF) gathering the following information: age, gender, smoking status (current, former: 6 months of smoking abstinence, never). eCO concentration was assessed in the waiting room on randomly chosen days and other days considered as a control. In this study, we randomized the days and not the subjects. The randomization of days was done once for the study period to obtain balanced samples of patients. All patients were consecutively included with or without eCO assessment depending on the randomization table.
Afterwards, during medical consultations, the junior doctor observed if concerns about smoking were raised and if any awareness about COPD were discussed and who initiated it (the patient or the GP). In the end both doctors were the ones who would consider if the patient declared acceptance for a COPD screening. However, we didn’t know if the patients finally had an appointment with the pulmonologist. Note that the GPs did not modify their usual practice as medical consultations were conducted in a conventional way.
From March 2013 to May 2013 (3 months), 410 consecutive patients were screened and enrolled.
Ethics and consent
The local ethics committee “Comité de Protection des personnes Sud-Mediterranee III” approved the study design (code UF: 9134, register: 2013-A00104-41). Because of the non invasive design of this study, a non opposition statement was obtained for all included patients.
Statistical analysis
The primary outcome was the comparison of rates of patient’s acceptance of a COPD screening between the two different groups of patients (performing and not performing eCO). The number of subjects needed was calculated by assuming that this rate will reach 15% when exhaled CO levels were measured and remained equal or below to 5% without exhaled CO measurements. Assuming a two-sided alpha risk of 0.05 and a beta risk of 0.05, we calculated that at least 219 patients per group would be required to identify a difference of 10%.
Outcome variables were acceptance for COPD screening, awareness for COPD and debate on smoking. Predictors were gender, age, smoking status, pack-years and patient’s group (performing or not performing eCO).
Data are expressed as mean ± SD for continuous variables (age, pack-years, exhaled CO), or as number and percentage for categorical variables (gender, tobacco status). Continuous variables were compared using Student’s t-test for normally distributed variables or Mann-Whitney rank-sum test for non-normally distributed variables. Pearson’s Chi-squared test or Fisher exact test was used to compare categorical variables. We did not use any penalization for multiple testing procedures. Multivariate models were established. Significance was established at P< 0.05. Kernel density estimate was used with a Gaussian kernel to estimate the exhaled CO distribution. The thresholds of CO values to predict smokers and non smokers were assessed using a Receiver Operating Characteristic (ROC) curve analysis. Statistical analysis was performed by an independent statistician, with R software (version 2.15.2).
Results
Between March and May 2013, 410 patients were included in two different offices. Measurement of exhaled CO was conducted in 216 patients. Patients’ characteristics are presented in Table 1. Fifty-three percent were females and the mean age (± standard deviation) was 61 ± 16 years. Twenty-three and 32% were current and former smokers respectively. Within smokers and former smokers, mean ± standard deviation cigarette smoking history was 22 ± 16 pack-years.
Cigarette smoking was discussed with up to 138 different patients (33.7%). Table 2 presents the outcomes according to patient groups and smoking status. From these 138 consultations, 91 have been subjected to CO measurements (P < 0.001). Forty-three out of 138 consultations, the debate was initiated by the patient himself while 95 were introduced by the physician. Taking into account the 166 debates in which awareness about COPD was discussed, 95 had been subjected to CO measurements (P = 0.128). COPD debate was mostly introduced by the physician (149 out of 166). In the end, 111 patients agreed on entering a COPD screening process, 61 being subjected to CO measurements (P = 0.576). Figure 1 displays differences in outcomes according to patient’s groups and smoking status.
Univariate and multivariate logistic regressions for the three outcomes are presented in Table 3. Smoking status and eCO measurement were independent factors associated with the occurrence of a debate on smoking during the medical consultation with odds ratios of 34.8 (95% CI = 11.0 to 133, P < 0.001) in current smokers and 11.8 (95% CI = 5.3 to 26.2, P < 0.001) in former smokers, and 2.56 (95% CI = 1.45 to 4.51, P = 0.001) for eCO assessment.
The only independent factor associated with acceptance for COPD screening was the smoking status.
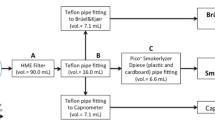
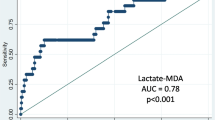
When assessed, mean ± standard deviation (median, interquartile range) eCO concentration was 3.88 ± 7.01 (1.00, [0 – 3.05]) exhaled CO (ppm). It reached 12.04 ± 9.00 (9.00, [4.00 – 19.00]) in current smokers, 0.82 ± 1.32 (0, [0 – 1.50]) for never smokers and 0.62 ± 1.29 (0, [0 – 1.00]) for former smokers. Figure 2 presents the distribution of the eCO for the overall population (Figure 2A), the non smokers (never and former, Figure 2B) and current smokers (Figure 2C). ROC correlating eCO value and current smoking status was performed (Figure 3), showing an optimal cutoff of eCO of over 2.5 ppm (AUC: 0.935, 95% CI [0.890-0.979], sensitivity: 0.867, specificity: 0.936, positive predictive value of 52/62 (83.9%), negative predictive value of 146/154 (94.8%)).
Discussion
In this study, we evaluated a screening model for early detection of patients with COPD assuming that measuring eCO can lead to a debate on smoking consequences. This investigation was to address a significant correlation between eCO assessment and a debate during consultations. This outcome was not achieved even though eCO increased expression of cigarette smoking concerns. Considering that smoking remains a key contributor factor to develop COPD, it was found that CO measurement device is a significant tool inducing a large increase in smoking discussions. The measurement of exhaled CO levels is an immediate and easy method of assessing a patient’s smoking status as it may potentially introduce a climate of concern.
Our study reveals that CO measurement in medical primary care consultations (for other causes than COPD symptoms) failed to promote patients acceptance for entering into a COPD screening process, even in current/former smokers. Potentially, this observation is related to poor COPD knowledge in the general population – and a weak concern in GP’s mind, and thus no clear debate was initiated on this subject or if so, the information exchanged during the debates on COPD was shallow. Nonetheless, rates of acceptance were surprisingly high (nearly half of the smokers) meaning that both patients and GPs behaviours could have been modified by the study itself, even in the group of patients not performing eCO measurement. The main limitation of the present study therefore is related to the lack of an observation period before the study.
As a wide spread of this disease is foreseen in the future and thus an increasing demand of medical consultations is expected, these results reinforce the need to commit additional efforts among lung specialists into sharing information about COPD among general population and doctors [2].
Spirometry in primary care will probably be the next step to achieve the goal of early COPD screening. PIKO-6 and other attempts related to airflow assessment mostly failed due to absence of funding and lack of expertise even though worth results were gathered [9-16]. Shortcoming spirometric pitfalls will probably require conjugated efforts between respiratory physicians and GPs but health care networks are currently working on these aspects. Pharmacists and other health care providers are to be involved too [17-19].
The opportunity offered by the future lung cancer screening programs that will be held in western countries should not be missed. These programs will potentially promote generalized and potentially repeated CT-scans in selected populations – who share the same risk factors than for COPD (age and smoking history). Findings unrelated to lung cancer have been shown to improve health status and potentially reduce deaths also because of these unexpected findings [20-23]. Successes of these programs are based on a clear and wide awareness for cancer in the general population, largely associated with smoking. Emphysematous changes of the lung parenchyma and other findings related to smoking (airway wall thickening, suggestive signs of bronchiolitis or desquamative interstitial pneumonia for example) are potential triggers for COPD screening as this can more easily be heard and become a cause for concern for both patients and doctors than spirometry alone [22].
Conclusions
We conclude that generalized eCO measurement in general practice failed to improve acceptance for early COPD screening. Larger studies using a comparative historical period are required to definitely conclude whether or not we should give up this very simple opportunity.
References
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
Soriano JB, Zielinski J, Price D. Screening for and early detection of chronic obstructive pulmonary disease. Lancet. 2009;374(9691):721–32.
Coultas DB, Mapel D, Gagnon R, Lydick E. The health impact of undiagnosed airflow obstruction in a national sample of United States adults. Am J RespirCrit Care Med. 2001;164(3):372–7.
Hurst JR, Vestbo J, Anzueto A, Locantore N, Mullerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–38.
GOLD [www.goldcopd.com].
Price D, Crockett A, Arne M, Garbe B, Jones RC, Kaplan A, et al. Spirometry in primary care case-identification, diagnosis and management of COPD. Prim Care Respir J. 2009;18(3):216–23.
Nelson SB, LaVange LM, Nie Y, Walsh JW, Enright PL, Martinez FJ, et al. Questionnaires and pocket spirometers provide an alternative approach for COPD screening in the general population. Chest. 2012;142(2):358–66.
Silkoff PE, Stevens A, Pak J, Bucher-Bartelson B, Martin RJ. A method for the standardized offline collection of exhaled nitric oxide. Chest. 1999;116(3):754–9.
Guerin JC, Roche N, Vicaut E, Piperno D, Granet G, Jannin M, et al. [Early detection of COPD in primary care: which tools?]. Rev Mal Respir. 2012;29(7):889–97.
Chibana K, Ishii Y, Anraku Y, Fukuda T. Prevalence of airflow limitation in patients diagnosed and treated for symptoms of chronic bronchitis by general practitioners in Tochigi Prefecture. Japan Intern Med. 2011;50(20):2277–83.
Frith P, Crockett A, Beilby J, Marshall D, Attewell R, Ratnanesan A, et al. Simplified COPD screening: validation of the PiKo-6(R) in primary care. Prim Care Respir J. 2011;20(2):190–8. 192 p following 198.
Sichletidis L, Spyratos D, Papaioannou M, Chloros D, Tsiotsios A, Tsagaraki V, et al. A combination of the IPAG questionnaire and PiKo-6(R) flow meter is a valuable screening tool for COPD in the primary care setting. Prim Care Respir J. 2011;20(2):184–9. 181 p following 189.
Solidoro P, Braido F, Baratta F, Bagnasco D, Esposito R, Aggeri M, et al. FEV6 assessment in spirometric abnormalities screening: the first population-based study in Italian pharmacies. Panminerva Med. 2013;55(1):87–92.
Gross NJ. Chronic obstructive pulmonary disease outcome measurements: what’s important? What’s useful? Proc Am Thorac Soc. 2005;2(4):267–71. discussion 290-261.
Pedersen OF. FEV6: a shortcut in spirometry? EurRespir J. 2006;27(2):245–7.
Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. FEV1/FEV6 and FEV6 as an alternative for FEV1/FVC and FVC in the spirometric detection of airway obstruction and restriction. Chest. 2005;127(5):1560–4.
Castillo D, Guayta R, Giner J, Burgos F, Capdevila C, Soriano JB, et al. COPD case finding by spirometry in high-risk customers of urban community pharmacies: a pilot study. Respir Med. 2009;103(6):839–45.
Takemura M, Mitsui K, Ido M, Matsumoto M, Koyama M, Inoue D, et al. Effect of a network system for providing proper inhalation technique by community pharmacists on clinical outcomes in COPD patients. Int J Chron Obstruct Pulmon Dis. 2013;8:239–44.
Verma A, Harrison A, Torun P, Vestbo J, Edwards R, Thornton J. Are pharmacists reducing COPD’S impact through smoking cessation and assessing inhaled steroid use? Respir Med. 2012;106(2):230–4.
Kanne JP. Screening for lung cancer: what have we learned? AJR Am J Roentgenol. 2014;202(3):530–5.
Aberle DR, DeMello S, Berg CD, Black WC, Brewer B, Church TR, et al. Results of the two incidence screenings in the National Lung Screening Trial. N Engl J Med. 2013;369(10):920–31.
Zurawska JH, Jen R, Lam S, Coxson HO, Leipsic J, Sin DD. What to do when a smoker’s CT scan is “normal”?: Implications for lung cancer screening. Chest. 2012;141(5):1147–52.
Cordier JF, Cottin V, Khouatra C, Revel D. Screening for lung cancer and idiopathic pulmonary fibrosis: killing two birds with one stone. Radiology. 2014;270(2):630–1.
Acknowledgements
We would like to thank Anne Verchere, who provided technical support to the implementation of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
NM, AB and IV conceived and designed the study. MA provided technical support to the implementation to the study. GM analyzed the data with support from NM. AB coordinated the writing of the manuscript with substantive contributions and critical revisions from CLK, ASG and NA. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Molinari, N., Abou-Badra, M., Marin, G. et al. Is generalization of exhaled CO assessment in primary care helpful for early diagnosis of COPD?. BMC Pulm Med 15, 44 (2015). https://doi.org/10.1186/s12890-015-0039-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-015-0039-6