Abstract
Background
Early essential newborn care has been implemented in countries regardless high or low neonatal mortality. This study aims to investigate the current practice of skin-to-skin contact (SSC) and its effect on exclusive breastfeeding during the hospital stay.
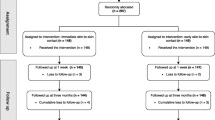
Methods
This is a cross-sectional study of 1812 Vietnamese mothers in multicenter. A questionnaire answered by the mothers was used to assess the duration of both SSC and breastfeeding practices. Multivariable logistic regression was used to identify a dose–response relationship between early SSC and prevalence of exclusive breastfeeding in hospital.
Results
There were 88.7% of mothers experiencing SSC with their infants right after birth and the highest prevalence of SSC was found in district hospitals. Among those experiencing SSC, 18.8% of the infants received more than 90 min of SSC and completed the first breastfeeding during SSC time. Prevalence of exclusive breastfeeding during maternity hospital stay was 46.7%. We found a significant dose–response relation between the duration of SSC and exclusive breastfeeding in hospital. Compared with infants without SSC, the prevalence of exclusive breastfeeding was higher in infants who experienced SSC for 15–90 min (adjusted odds ratio [aOR], 95% confidence interval [95%-CI]: 2.62 [1.61–4.27]) and more than 90 min (aOR [95%-CI]: 5.98 [3.48–10.28]). Completed first breastfeeding during SSC time (aOR [95%-CI]: 4.24 [3.28–5.47]) and being born in district hospitals (aOR [95%-CI]: 2.35 [1.79–3.09]) were associated with increased prevalence of exclusive breastfeeding during hospital stay. On the other hand, mother education level as high school/intermediate (aOR [95%-CI]: 0.58 [0.42–0.82]) and place of residence classified as rural decreased odds of exclusive breastfeeding in hospital (aOR [95%-CI]: 0.78 [0.61–0.99]).
Conclusion
Our results demonstrate a strong dose–response relationship between duration of SSC and exclusive breastfeeding in hospital. Interventions that support exclusive breastfeeding during hospital stay, especially achieving prolonged uninterrupted SSC, could improve the duration of breastfeeding.
Similar content being viewed by others
Introduction
Optimal breastfeeding practice is one of the most cost-effective intervention for improving mortality and morbidity for children under five years [1, 2]. It could save over 800,000 or 12% of all deaths annually [3, 4]. Despite strong evidence of the short- and long-term health benefits for both children and mothers, at global level, nearly two third of infants are not exclusively breastfed during the first six months of life and nearly 60% of infants are not put on breast in the first hour of life [5]. Strategies that have had great impact on promoting breastfeeding rate, especially in develo** countries, includes breastfeeding education and support. Skin-to-skin contact (SSC) is another crucial evidence-based practice that provides a maximized chance for breastfeeding [6, 7].
Early exclusive breastfeeding during hospital stay was identified as an effective strategy to improve the duration of breastfeeding [8,9,10]. Infants who breastfed exclusively in hospital were breastfed for four months longer than those who supplemented with formula [8]. Among mothers who intended exclusive breastfeeding, by day 60, formula supplementation in hospital was associated threefold risk of cessation of breastfeeding [10]. Thus, improving exclusive breastfeeding during hospital stay could have significant impact on short- and long-term breastfeeding outcomes. Despite the benefits, the proportion of exclusive breastfeeding in hospital remains lower than the current recommendations. Vehling et al. showed a prevalence of 74% infants were exclusively breastfed in hospital in Canada [8], Cox et al. reported a prevalence of 82.7% in Australia [11], while this proportions were lower in areas of southern Vietnam with 33% [12]. Identifying factors associated with exclusive breastfeeding in hospital is important to prioritize strategies for promoting exclusive breastfeeding in hospital.
Immediate SSC is referred to the placement of the naked baby prone to the bare chest of his or her mother at birth. Prolonged SSC is an important component of the package intrapartum and immediate newborn care interventions named Early Essential Newborn Care (EENC). This package includes: immediate and thorough drying newborn; immediate and sustained SSC between mother and babies for at least 90 min; delayed cord clam** for at least one to three minutes; non-separation mother and babies until the first breastfeeding is completed [13]. Since 2014, World Health Organization (WHO) has supported countries in the Western Pacific Region to scale up EENC widely. During the COVID-19 pandemic, SSC is still recommended by WHO as “the benefits substantially outweigh the potential risks of transmission and illness associated with the disease” [14]. Despite strong recommendations from the WHO, the practice of SSC varies from 1–98% of infants across the world, with higher prevalence of SSC in high income countries compared to low-middle-income countries with a range from 8 to 74% [15]. Variation in the starting time and duration of SSC is another concern. Nevertheless, limited number of studies have been reported in develo** countries to identifying the rate of SSC and its effects [15]. Several studies with small sample size showed evidence support the benefits of SSC to breastfeeding at hospital discharge and one to four months after birth [16]. Women who experienced SSC also breastfed their children longer [16]. Further, Bramson 2010 and Li 2020 found that a longer duration of SSC was correlated with a higher rate of exclusive breastfeeding [17, 18]. However, there are still lacking evidence on clear advantages of longer duration of SSC and optimal duration of SSC has not been established yet.
Between 2016 and 2017, among 1383 maternal interviews from eight countries in East Asia and the Pacific, 90.9% of mothers practiced SSC with their babies after birth [18]. The exclusive breastfeeding rate since birth and before discharge ranged from 67.8% for infants not experienced SSC to 92.7% for infants placed in 60–90 min of uninterrupted SSC. On the other hand, exclusive breastfeeding rate at 4–5 months was 41.3% for this region between 2010 and 2018 [Maternal and infant characteristics Detailed maternal and infant characteristics are presented in Table 1. Nearly 85% of the mothers had education level from high school to postgraduate. There were 49.6% of the infants were delivered by C-section and 64.7% of the infants were delivered in central/provincial hospitals. Overall, 88.7% of all mothers had SSC with their infants after birth. Prevalence of SSC was significantly higher in district hospitals compared to central/provincial hospitals (p < 0.001). The most common duration of SSC was 15–90 min (45.4%), followed by < 15 min (32.7%) and > 90 min (21.9%). Qualified SSC was identified in 18.8% of all mothers. The C-section group had a higher proportion of SSC than vaginal delivery group in all central/provincial, district and private hospitals (Fig. 2). The highest prevalence of qualified SSC were in district hospital (26.0%). There were 96.9% (n = 1755) of mothers breastfed their infants and 40.9% (n = 742) provided them with formula during maternal hospital stay. Overall, the exclusive breastfeeding rate was 46.7% (n = 846). The exclusive breastfeeding rate was significantly higher in infants born by vaginal delivery than C-section (p < 0.0001). The C-section and vaginal delivery groups had similar proportion of breastfeeding (95.8% vs 97.9%, p = 0.3) but the C-section group had higher proportion of using formula milk (47% vs 35.1%, p < 0.001) (Fig. 3). There were 332 mothers (18.3%) fed their infants with colostrum milk powder which was balanced between the C-section and vaginal delivery groups. In multivariate logistic regression analysis, after adjusting for maternal and infant characteristics in Table 2 (mother’s age and education level, having complication during pregnancy and delivery, place of residence, parity, mode of delivery, hospital of birth, infant’s sex, birth weight and complication at birth), significant association was found between the duration of SSC during maternal hospitalization and the rate of exclusive breastfeeding. The longer early SSC mothers and infants, the more likely that the infants were breastfed exclusively during hospital stay. Compared with infants without SSC, the prevalence of exclusive breastfeeding was higher in infants who experienced SSC for 15–90 min (adjusted odds ratio [aOR], 95% confidence interval [95%-CI]: 2.62 [1.61–4.27]) and more than 90 min (aOR [95%-CI]: 5.98 [3.48–10.28]). After adjusting for various explanatory variables, initiation of first breastfeeding during SSC time was associated with increased rate of exclusive breastfeeding with aOR of 4.24 (95% confidence interval (CI) 3.28 to 5.47). Another factor increased the odds of exclusive breastfeeding was giving birth in district hospitals. On the other hand, mother education level as high school/intermediate and place of residence classified as rural decreased odds of exclusive breastfeeding (Table 2).Skin-to-skin contact practice
Breastfeeding practice
Duration of skin-to-skin contact associated with increased exclusive breastfeeding rate
Other factors associated with exclusive breastfeeding rate
Discussion
Since 2014, Vietnam was among eight priority countries in the Western Pacific Region that has been supported by WHO to introduce, sustain and scale-up EENC [26]. In 2017, 88% of hospitals in the country have adopted EENC. Our study showed a high prevalence of babies (88.7%) receiving early SSC, but only 18.8% of the babies received qualified SSC. Another key finding of the current research is that the exclusive breastfeeding rate during maternal hospital stay was 46.7%. Multivariable logistic regression identified six factors associated with prevalence of exclusive breastfeeding rate included mother’s education level, place of residence, level of hospital where providing childbirth services, duration of SSC and initiation of first breastfeeding during SSC.
In our study, most infants experienced SSC, consistent with previous reports of the WHO for the Western Pacific Region [26]. This rate, however, showed an impressive improvement of SSC practice to those reported by WHO for Vietnam in 2017 with 59% [26]. Early SSC is a key component of a package of simple evidence-based interventions delivered around the time of birth. It starts in the first minute of life after immediate and thorough drying and assessment of the infants. At least ninety minutes of uninterrupted SSC between mothers and newborns maximizes the chance for infants to be ready to breastfeed [16, 18]. Readiness to breastfeed differs considerably from infant to infant. A longer duration of uninterrupted SSC, the higher possibility of infant completing the first breastfeed [17, 27]. Previous studies have indicated that early initiation of breastfeeding increased the likelihood of exclusive breastfeeding. Our finding regarding the relationship between duration of SSC and prevalence of exclusive breastfeeding during hospital stay is in line with previous results [7, 17, 18]. The optimal SSC duration after birth has not yet been established [18]. In the current study, SSC of 15–90 min was associated with increased prevalence of exclusive breastfeeding compared with non-SSC. However, the most significant improvement in prevalence of exclusive breastfeeding was found when SSC duration was over 90 min.
Despite the fact that uninterrupted SSC for at least 90 min is highly recommended, only about 20% of the infants in our study had experienced > 90 min contact with their mothers. As a result of that, less than one fifth of the infants had received > 90 min of SSC and completed first breastfeeding before separation which was defined as qualified SSC in our study. In 2017, WHO reported a prevalence of prolonged (≥ 90 min) SSC in national hospital was 76% and 25% in subnational hospitals in Vietnam [26]. Our finding, in contrast, showed a lower prevalence of prolonged SSC in central/provincial hospitals than in district hospitals. Over-crowding in central and provincial levels could be a barrier to maintain SSC over 90 min. More importantly, results of both previous reports and current study emphasized the need for improving the quality of SSC including increasing the length of early SSC and completing the first breastfeeding before separation.
Prevalence of exclusive breastfeeding during hospital stay in our study was higher than reported for Vietnam by Le et al. (33%), and Ramoo et al. (7%) [12, 24]. This improvement may be linked to the action at healthcare facilities to limit the use of formula, the strategies for scaling up and improving early SSC practices in a national scale. Our finding also have a similar pattern of breastfeeding behaviour with Le et al. finding that the majority of mothers fed their infants with breast milk during hospital stay. However, formula and colostrum milk powder were still used by nearly half of mothers to feed their infants during the first few days of life. Monitoring and intervention are needed to reduce the use of formula in healthcare facilities.
Factors associated with exclusive breastfeeding during maternity hospital stay is another important finding of our research. Our hypothesis that the duration of uninterrupted SSC had a strong positive dose–response relationship with prevalence of exclusive breastfeeding during hospital stay was confirmed. Moreover, we have included in multivariable logistic regression maternal and infant sociodemographic variables, complication during pregnancy and at birth, mode of delivery, level of hospital at birth, early SSC and initiation of first breastfeeding. After controlling for these factors, level of hospital at birth, place of residence, mother’s education level had impacts on exclusive breastfeeding rate. Our results share a number of similarities with Bramson et al. and Le et al. [12, 17]. SSC between mothers and infants was not uniformly implemented in different levels and types of hospitals [17, 26]. In Vietnam, central and provincial hospitals in large cities are facing a problem of overcrowding with very high occupancy rates. Less overcrowded or not crowded in district hospital may play a part in the effectiveness of SSC including longer duration of SSC. The difference in factors associated with breastfeeding practice between urban and rural was also found in a previous study [12]. The study results provide further evidence to recommend optimal duration of SSC for improving breastfeeding outcomes.
Strengths and limitations of the study
To our knowledge, this is the first analysis to examine the current practice of SSC in Vietnam and the significant dose–response relationship between increasing duration of SSC and prevalence of exclusive breastfeeding during maternity hospital stay in a lower middle-income country that controlled for potential confounding factors such as maternal and infant’s demographic characteristic, hospital of birth, mode of delivery, problem during pregnancy and at birth of mothers and infants. In addition, the exclusive breastfeeding rate was calculated based on feeding types that mothers reported providing for infants. This is likely to reduce bias resulting from the perception of mothers of the definition of the exclusive breastfeeding.
The study has some limitations. As this study was restricted to mothers who brought their children to the CHC for routine immunisation in two cities of Vietnam, the results may not be generalized for the whole population and do not represent quality of healthcare services. Recall bias is another concern as the study used self-report questionnaire and the data collection were conducted far from birth. Variables such as cultural and the intent to breastfeed, the capability of being able to afford to buy formulas have not been included in our questionnaire.
Conclusions
This study highlights the suboptimal breastfeeding practice in Vietnam and demonstrate the significant dose–response relationship between increasing duration of SSC and prevalence of exclusive breastfeeding. In addition, the completion of first breastfeeding during SSC time also significantly increased the likelihood of exclusive breastfeeding during hospital stay. To maximise the chance of receiving first breastfeeding and exclusive breastfeeding practice, infants should receive immediate and uninterrupted SSC for 90 min and more. More efforts are needed to accelerate high-quality EENC for improving breastfeeding in Vietnam.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available, because these data is a subset of a dataset and another manuscripts are drafting based on analysing the dataset, but are available from the corresponding author on reasonable request.
Abbreviations
- EENC:
-
Early Essential Newborn Care
- CHC:
-
Commune Health Center
- SSC:
-
Skin-to-skin Contact
References
Gülmezoglu AM, Lawrie TA, Hezelgrave N, et al. Interventions to Reduce Maternal and Newborn Morbidity and Mortality. In: Black RE, Laxminarayan R, Temmerman M, et al., editors. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2016 Apr 5. Chapter 7. Available from: https://www.ncbi.nlm.nih.gov/books/NBK361904/. https://doi.org/10.1596/978-1-4648-0348-2_ch7.
Lassi ZS, Middleton PF, Crowther C, Bhutta ZA. Interventions to improve neonatal health and later survival: an overview of systematic reviews. EBioMedicine. 2015;2(8):985–1000.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51.
World Health Organization. Infant and young child feeding. Available at: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding. Accessed 15 Oct 2021.
World Health Organization: Breastfeeding. Available at: https://www.who.int/health-topics/breastfeeding#tab=tab_1. Accessed 08 Nov 2020.
Safari K, Saeed AA, Hasan SS, Moghaddam-Banaem L. The effect of mother and newborn early skin-to-skin contact on initiation of breastfeeding, newborn temperature and duration of third stage of labor. Int Breastfeed J. 2018;13(1):32.
Mikiel-Kostyra K, Mazur J, Bołtruszko I. Effect of early skin-to-skin contact after delivery on duration of breastfeeding: a prospective cohort study. Acta Paediatr (Oslo, Norway : 1992). 2002;91(12):1301–6.
Vehling L, Chan D, McGavock J, Becker AB, Subbarao P, Moraes TJ, et al. Exclusive breastfeeding in hospital predicts longer breastfeeding duration in Canada: implications for health equity. Birth. 2018;45(4):440–9.
Holmes AV. Establishing successful breastfeeding in the newborn period. Pediatr Clin North Am. 2013;60(1):147–68.
Chantry CJ, Dewey KG, Peerson JM, Wagner EA, Nommsen-Rivers LA. In-hospital formula use increases early breastfeeding cessation among first-time mothers intending to exclusively breastfeed. J Pediatr. 2014;164(6):1339-45.e5.
Cox K, Giglia R, Zhao Y, Binns CW. Factors associated with exclusive breastfeeding at hospital discharge in rural Western Australia. J Hum Lact. 2014;30(4):488–97.
Le QNT, Phung KL, Nguyen VTT, Anders KL, Nguyen MN, Hoang DTT, et al. Factors associated with a low prevalence of exclusive breastfeeding during hospital stay in urban and semi-rural areas of southern Vietnam. Int Breastfeed J. 2018;13(1):46.
Tran HT, Mannava P, Murray JCS, Nguyen PTT, Tuyen LTM, Hoang Anh T, et al. Early essential newborn care is associated with reduced adverse neonatal outcomes in a Tertiary Hospital in Da Nang, Viet Nam: a pre- post- intervention study. EClinicalMedicine. 2018;6:51–8.
World Health Organization. Skin-to-skin contact helps newborns breastfeed. Available at: https://www.who.int/westernpacific/news/feature-stories/detail/skin-to-skin-contact-helps-newborns-breastfeed. Accessed 16 Oct 2021.
Abdulghani N, Edvardsson K, Amir LH. Worldwide prevalence of mother-infant skin-to-skin contact after vaginal birth: a systematic review. PloS One. 2018;13(10):e0205696-e.
Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016;11(11):CD003519-CD.
Bramson L, Lee JW, Moore E, Montgomery S, Neish C, Bahjri K, et al. Effect of early skin-to-skin mother–infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. J Hum Lact. 2010;26(2):130–7.
Li Z, Mannava P, Murray JCS, Sobel HL, Jatobatu A, Calibo A, et al. Association between early essential newborn care and breastfeeding outcomes in eight countries in Asia and the Pacific: a cross-sectional observational -study. BMJ Glob Health. 2020;5(8):e002581.
Zong Xn, Wu H, Zhao M, Magnussen CG, ** B. Global prevalence of WHO infant feeding practices in 57 LMICs in 2010-2018 and time trends since 2000 for 44 LMICs. EClinicalMedicine. 2021;37:100971.
World Health Organization, Regional Office for the Western Pacific. Second biennial progress report : 2016–2017 (Action Plan for Health Newborn Infants in the Western Pacific Region: 2014–2020. Manila: WHO Regional Office for the Western Pacific, 2018. Available at: https://apps.who.int/iris/handle/10665/272803. Accessed 24 Mar 2022.
Binns C, Lee A, Sauer K, Hewitt K. Reported Breastfeeding Rates in the Asia-Pacific Region. Curr Pediatr Rev. 2012;8(4):339–45.
Checkley W, Epstein LD, Gilman RH, Figueroa D, Cama RI, Patz JA, et al. Effects of EI Niño and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355(9202):442–50.
Le DC, Kubo T, Fu**o Y, Pham TM, Matsuda S. Health care system in Vietnam: current situation and challenges. Asian Pac J Dis Manag. 2010;4(2):23–30.
Ramoo S, Trinh TA, Hirst JE, Jeffery HE. Breastfeeding practices in a hospital-based study of Vietnamese women. Breastfeeding Med. 2014;9(9):479–85.
Musengimana G, Mukinda FK, Machekano R, Mahomed H. Temperature variability and occurrence of diarrhoea in children under five-years-old in Cape Town Metropolitan Sub-Districts. Int J Environ Res Public Health. 2016;13(9):859.
WHO Reginal Office for the Western Pacific. Consultation on the draft regional action plan for healthy newborns in the Western Pacifc 2014–2018. Manila: WHO Reginal Office for the Western Pacific, 2013. Available at: https://apps.who.int/iris/handle/10665/208778. Accessed 20 Oct 2021.
Widström AM, Lilja G, Aaltomaa-Michalias P, Dahllöf A, Lintula M, Nissen E. Newborn behaviour to locate the breast when skin-to-skin: a possible method for enabling early self-regulation. Acta Paediatr (Oslo, Norway: 1992). 2011;100(1):79–85.
Acknowledgements
We would like to thank Nguyen Do Thi Phuong Thao, Nguyen Thanh Tai, Tran Thanh Dat, Huynh Ngoc Truong Thy, Nguyen Thi Nhu Y, Phan Cao Sang, Mac Thi Luu, Nguyen Thi Minh Phuong, Nguyen Thi Lan Nhi, Do Thi Hong Nhien, Nguyen Thi Bich Vy, Nguyen Thi Thanh Thuy, Le Han, Nguyen Quang Huy, Nguyen Tan Thinh, Duong Thi Y Nhu, Tran Huynh Anh Thu, Hoang Thi Dao, Nguyen Thinh Duc, Bui Huu Trong, Nguyen Thi Hong Sa, Dinh Kieu Hoa Phuong, Le Van Hiep, Nguyen Thi Linh, Nguyen Thi Thuy Trang, Do My Hanh for supporting us in data collection of this study.
Funding
This research is funded by Funds for Science and Technology Development of the University of Danang under project number B2020-DN01-28.
Author information
Authors and Affiliations
Contributions
HTNG, DTTD, NLV, NTTN, TTP, LQT, LO, PDTA, TTK, NTAT, MNL, TTTN, LTMH performed the research. HTNG designed the research study, analysed data and wrote the first draught of the study. NTH and NLV provided major revisions. DTTD, NTTN, TTP, LQT, LO, PDTA, TTK, NTAT, MNL, TTTN, LTMH provided study revisions and reviewed content for technical accuracy. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of University of Medicine and Pharmacy at Ho Chi Minh City according to Decision No. 990/HĐĐĐ-ĐHYD date 11/01/2020. The written informed consent was obtained from all the participants. This was an anonymous survey.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Giang, H.T.N., Duy, D.T.T., Vuong, N.L. et al. Prevalence of early skin-to-skin contact and its impact on exclusive breastfeeding during the maternity hospitalization. BMC Pediatr 22, 395 (2022). https://doi.org/10.1186/s12887-022-03455-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03455-3