Abstract
Background
The incidence of refractive surgery-related dry eye disease (DED) is rising due to the increasing popularity of corneal refractive surgery. The moisture chamber goggles (MCGs) have been shown to tear evaporation by increasing local humidity and minimizing airflow. The current study aims to evaluate the efficacy of moisture chamber goggles for refractive surgery-related DED.
Methods
In this nonrandomized open-label controlled study, 78 participants (156 eyes) receiving refractive surgery were enrolled between July 2021 and April 2022, and sequentially allocated to MGC and control groups. 39 participants were allocated to the MGC groups, of which 53.8% received small-incision lenticule extraction (SMILE) and 46.2% received femtosecond laser-assisted in situ keratomileusis (FS-LASIK), and were instructed to wear MCGs for the duration of 1 month postoperatively, in addition to the standard postoperative treatment received by the control groups (56.4% SMILE, 43.6% FS-LASIK). Participants underwent full ophthalmic examinations, including visual acuity, manifest refraction, DED evaluations, and higher-order aberrations (HOAs), both preoperatively and at routine follow-ups 1 day, 1 week, and 1 month after surgery. DED parameters included non-invasive tear film break-up time (NIBUT), tear meniscus height (TMH), conjunctival congestion, lipid layer thickness (LLT), and ocular surface disease index (OSDI) questionnaires. Student’s t-test was used for comparisons between control and MCG groups, and between preoperative and postoperative parameters within groups.
Results
Postoperative NIBUT decreased in both SMILE and FS-LASIK control groups 1 day after the surgery (SMILE, P = 0.001; FS-LASIK, P = 0.008), but not in the corresponding MCG groups (SMILE, P = 0.097; FS-LASIK, P = 0.331). TMH in the MCG group was significantly higher at 1 week (P = 0.039) and 1 month (P = 0.015) in SMILE, and 1 day (P = 0.003) in FS-LASIK groups. In FS-LASIK participants, significantly lower HOAs and coma levels in the MCG group were observed 1 day (total HOAs, P = 0.023; coma, P = 0.004) and 1 week (total HOAs, P = 0.010, coma, P = 0.004) after surgery. No consistent statistically significant intergroup difference was observed between MCG and control groups in conjunctival congestion, LLT, and OSDI.
Conclusions
MCGs effectively slowed tear evaporation, increased tear film stability, and improved HOAs in patients receiving SMILE and FS-LASIK surgeries. MCG is an effective adjuvant therapy in the comprehensive management of refractive surgery-related DED.
Similar content being viewed by others
Background
Dry eye disease (DED) is a multifactorial disease of the ocular surface, characterized by the loss of homeostasis of the tear film. DED can be induced by a variety of iatrogenic factors, including corneal refractive surgery [1, 2]. The increasing popularity of refractive surgery is accompanied by the increasing prevalence of refractive surgery-related DED. Previous studies have demonstrated that refractive surgery inevitably leads to transient ocular surface disturbances postoperatively, with varying incidence and severity between studies [3,4,5,6]. A number of etiologies have been shown to contribute to refractive surgery-related DED, including prior history of DED, meibomian gland function, ocular inflammation, choice of surgical techniques, and damage to the corneal subbasal nerve plexuses [7, 8].
The current consensus recommended comprehensive management for surgically-induced DED, encompassing both preoperative and postoperative approaches [9, 10]. The Tear Film and Ocular Surface (TFOS) Dry Eye Workshop (DEWS) II reports stressed the importance of treatment of preexisting DED before surgery, postoperative tear replacement, tear conservation, and anti-inflammation therapies [1, 9]. Moisture chamber goggles (MCGs) were recommended as a basic approach for tear conservation. They have been shown to slow tear evaporation by increasing local humidity and minimizing airflow. Previous studies have focused on the short-term efficacy of MCGs in DED patients, as well as in patients exposed to adverse environment [11,12,13,14]. However, the long-term efficacy of MCGs and their effects on refractive surgery recipients require further investigation.
This prospective controlled intervention study aims to explore the effects of MCG on refractive surgery-related DED, by comparing the visual outcomes and DED parameters between the control and MCG-treated participants in the postoperative period.
Patients and methods
Study design
This nonrandomized open-label controlled study enrolled patients who underwent small-incision lenticule extraction (SMILE) and femtosecond laser-assisted in situ keratomileusis (FS-LASIK) procedures between July 2021 and April 2022 at the Department of Ophthalmology, Peking Union Medical College Hospital (PUMCH). The participants were sequentially allocated to MCG and control groups. The study adhered to the tenets of the Declaration of Helsinki and was supervised by the institutional review board at PUMCH. Signed informed consent was obtained from all patients.
Inclusion criteria were as follows: (1) age between 18 and 40 years; (2) stable refractive error (≤ 0.5 D change of refractive error) in the past 1 year; (3) spherical equivalent (SE) between -2.50 D and -20.00 D; (4) astigmatism up to -5.00 D; (5) logarithm of the minimal angle of resolution (LogMAR) of BCVA of 0.1 or better; (6) clear crystalline lens.
Exclusion criteria included current or history of severe ophthalmic diseases including corneal diseases, cataracts, glaucoma, retinal detachment, neuro-ophthalmic diseases, trauma, ocular surgery, and diagnosed autoimmune diseases. Patients with severe preoperative dry eye, defined as prominent desiccation before surgery, a fluorescein TBUT < 2 s, and/or corneal epithelial defects in 2 quadrants or more and/or fluorescein staining ≥ 30, were excluded from the study [15, 16].
All participants underwent complete preoperative ophthalmic examinations, including uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), manifest and cycloplegic refraction by autorefractometery (RM-800, Topcon, Japan), standard slit-lamp biomicroscopy and funduscopic examinations, gonioscopy, intraocular pressure (IOP) by a non-contact tonometer (Canon, Japan), and corneal topography (Canon, Japan). The participants underwent routine follow-ups at 1 day, 1 week, and 1 month postoperatively, with examinations including BCVA, manifest refraction, standard slit-lamp biomicroscopy, and IOP measurement. OSDI, DED evaluation, and HOA examinations were performed at the preoperative examination and each follow-up session. Participants unable to complete preoperative examinations or more than 1 follow-up examinations were excluded from the analyses.
Surgical procedures
Surgical procedures were performed by an experienced surgeon (YL). SMILE was performed under topical anesthesia, with the VisuMax 500 kHz femtosecond laser (Carl Zeiss Meditec, Germany). Cap thickness was set at 110–120 μm, cap diameter at 7.0–7.5 mm, and lenticules diameter at 6.0–6.5 mm, with a transition zone of 0.1 mm. A 2 mm side cut incision was made at the 10 o’clock position of the cornea. Cut energy was set at 135 nJ. The stromal lenticules were removed using forceps.
FS-LASIK was performed using the VisuMax 500 kHz femtosecond laser (Carl Zeiss Meditec, Germany) for flap creation, and the Schwind Amaris 179 excimer laser (Schwind Eye-Tech-Solutions, Germany) for refractive correction. Flap thickness was set at 90 or 100 μm, flap diameter at 8.5 mm, and hinged at the 12 o’clock position of the cornea. The side cut angle was at 120 degrees.
The prescriptions for postoperative management were as follows: tobramycin dexamethasone eye drops (s.a. Alcon-Couvreur n.v.), four times a day for two weeks, deproteinized calf blood extract eye gel (**ngqi pharmaceuticals), once for four weeks, and sodium hyaluronate eye drops, four times a day for four weeks.
Moisture chamber goggle
The moisture chamber goggle consists of two moisture-retaining chambers and supporting structures. The chambers have rubber adapters to better fit the frame of the user, providing better sealing and a more comfortable wearing experience. At each junction of the chamber and the temples, a tank connected to the chamber, filled with water-absorbing material, was designed to provide moisture and maintain humidity levels in the chambers. The participants were asked to fill the tanks each time before use. The participants were instructed to use MCG for at least half of the day according to instruction postoperatively for 1 month.
DED evaluation
DED-1L Dry Eye Analyzer (Kanghuaruiming Science Technology, China) is a comprehensive dry eye diagnostic system that performs non-invasive tear film break-up time (NIBUT), tear meniscus height (TMH), lipid layer interferometry, and congestion assessment [17]. NIBUT and TMH measurement was performed under infrared light, while lipid layer interferometry and congestion examination was conducted under natural white illumination. NIBUT is automatically measured as the duration from the last complete blink to the first discontinuity in Placido ring reflections under infrared illumination. TMH was calculated as the average of three measurements at central, medial, and lateral paracentral locations. The congestion levels in the conjunctival and perilimbal regions were automatically measured under natural light, and an average congestion score was calculated.
The LipiView Ocular Surface Interferometer (TearScience, United States) measures the absolute thickness of the lipid layer using interferometric images of the tear film. During the examination, the participants were asked to maintain still and blink normally. The camera was adjusted to focus on the tear film plane and captured a 25-s video with a clear interferometric image of the tear film [18]. Lipid layer thickness (LLT) is measured in interferometric color units (ICU). LipiView automatically calculates the average (AvgICU), maximal (MaxICU), and minimal (MinICU) measurements of LLT. The homogeneity in lipid layer distribution is reflected by \(DevICU= \sqrt{{(MaxICU-AvgICU)}^{2}+{(MinICU-AvgICU)}^{2}}\).
To avoid introducing bias from diurnal variations, objective DED evalutions were performed in the mornings. The participants were asked to complete the OSDI questionnaire at preoperative examination and 1-month follow-up.
HOA evaluation
The iTrace aberrometer (Tracey Technologies, United States) was used to measure ocular HOAs following 10 min of dark adaptation without pharmacological pupil dilatation before the operation and at the follow-ups. The root means square values of total HOAs, spherical aberration, secondary astigmatism, coma aberration, and trefoil aberration were recorded.
Statistical analysis
Statistical analyses were performed with R (version 4.2.3) and RStudio (2023.03.1 + 446). BCVA and UCVA were converted to logMAR visual acuity. Continuous variables were presented as mean ± standard deviation (SD) under normal distribution or median with interquartile range (IQR) under non-normal distribution. Independent student’s t-test was used for comparisons of parameters between control and MCG groups. Paired student’s t-test was used for comparisons between preoperative and postoperative parameters within a group. A p-value of less than 0.05 was considered statistically significant.
Results
Demographics and clinical characteristics
Demographics and preoperative parameters are shown in Table 1. The SMILE control and MCG groups included 22 (27.3% male, 72.7% female) and 21 (19.0% male, 81.0% female) participants, and The FS-LASIK control and MCG groups included 17 (23.5% male, 76.5% female) and 18 (16.7% male, 83.3% female) participants, respectively. The mean age was 28.41 ± 6.08 and 26.67 ± 4.48 years for SMILE control and MCG groups (P = 0.290), and 30.41 ± 5.82 and 31.61 ± 10.58 years for FS-LASIK control and MCG groups (P = 0.680), respectively. There was no statistically significant difference in preoperative SE, visual acuity, total HOA, and main DED parameters.
Visual acuity and postoperative SE
In both SMILE control and MCG groups, postoperative UCVA significantly improved compared to preoperative BCVA at 1 week (control, P = 0.002; MCG, P = 0.024) and 1 month (control, P < 0.001; MCG, P < 0.001) after surgery, but not at 1 day (control, P = 0.322; MCG, P = 0.525) (Tables 2 and 3). In FS-LASIK groups, postoperative UCVA was significantly better at 1 day in both control (P = 0.001) and MCG groups (P = 0.030), and 1 month in the control group (P = 0.004), but not at 1 week (control, P = 0.179; MCG, P = 0.923) or 1 month in the MCG group (P = 0.268). Postoperative MRSE significantly improved compared to preoperative at 1 day, 1 week, and 1 month after surgery for both SMILE and FS-LASIK control and MCG groups (P < 0.001). No statistically significant intergroup difference was observed in postoperative UCVA and MRSE in both SMILE and FS-LASIK groups (Fig. 1).
Visual acuity and manifest refractive spherical equivalent after moisture chamber goggles treatment at postoperative 1 day, 1 week, and 1 month. A Visual acuity of control and MCG groups in SMILE participants, best-corrected visual acuity (BCVA) in log MAR preoperatively, and uncorrected visual acuity (UCVA) postoperatively; B Visual acuity of control and MCG groups in FS-LASIK participants, BCVA preoperatively and UCVA postoperatively; C MRSE of control and MCG groups in SMILE participants; D MRSE of control and MCG groups in FS-LASIK participants. Independent student’s t-test for comparisons between control and MGC groups. MRSE, manifest refractive spherical equivalent; MCG, moisture chamber goggles; SMILE, small-incision lenticule extraction; FS-LASIK, femtosecond laser-assisted in situ keratomileusis; PreOp, preoperative; Po, postoperative; NS, not significant
Dry eye parameters
Non-invasive tear break-up time
In both SMILE and FS-LASIK control groups, postoperative NIBUT decreased 1 day after the surgery (SMILE, P = 0.001; FS-LASIK, P = 0.008), but not in the corresponding MCG groups (SMILE, P = 0.097; FS-LASIK, P = 0.331) (Tables 2 and 3). This effect persisted in the FS-LASIK control group at 1 week (P = 0.037) and 1 month (P = 0.033) postoperatively, but not in the SMILE control group. Intergroup differences between control and MCG groups were not statistically significant at each follow-up in both SMILE and FS-LASIK participants (Fig. 2).
Tear meniscus height, non-invasive tear film break-up time, and congestion evaluation after moisture chamber goggles treatment at postoperative 1 day, 1 week, and 1 month. A TMH of control and MCG groups in SMILE participants; B TMH of control and MCG groups in FS-LASIK participants; C NIBUT of control and MCG groups in SMILE participants; D NIBUT of control and MCG groups in FS-LASIK participants; E Congestion score of control and MCG groups in SMILE participants; F Congestion score of control and MCG groups in FS-LASIK participants. *p < 0.05, **p < 0.01, ***p < 0.001, independent student’s t-test. TMH, tear meniscus height; NIBUT, non-invasive tear film break-up time; MCG, moisture chamber goggles; SMILE, small-incision lenticule extraction; FS-LASIK, femtosecond laser-assisted in situ keratomileusis; PreOp, preoperative; Po, postoperative; NS, not significant
Tear meniscus height
A significant decrease in TMH was observed in SMILE control groups at 1 week (P = 0.011) and 1 month (P = 0.003) follow-ups, and a significant increase in FS-LASIK MCG groups 1 day postoperatively (P = 0.024) (Tables 2 and 3). In both SMILE and FS-LASIK participants, TMH measurements in the MCG groups were higher than those in the control groups (Fig. 2). The comparison was statistically significant at 1 week (P = 0.039) and 1 month (P = 0.015) postoperatively in the SMILE groups, and 1 day (P = 0.003) in the FS-LASIK groups.
Conjunctival congestion
The conjunctival congestion level was generally lower in the MCG groups compared to the control groups (Tables 2 and 3). A significant decrease in postoperative congestion score was observed in the SMILE MCG group at 1 week (P = 0.002) and 1 month (P = 0.004) after surgery, FS-LASIK control group at 1 month (P = 0.001), and FS-LASIK MCG group at 1 week (P < 0.001). No statistically significant intergroup difference existed except in FS-LASIK groups at 1-week follow-up (P < 0.001) (Fig. 2).
Lipid layer thickness
A significant decrease in AvgICU was observed in the SMILE MCG group in all three follow-ups (1 day, P = 0.023; 1 week, P = 0.001; 1 month, P = 0.014), and the SMILE control group (P = 0.037) and FS-LASIK MCG group (P = 0.004) at 1 week postoperatively. No significant intergroup difference was observed in AvgICU except between FS-LASIK groups 1 week after the surgery (P = 0.018) (Fig. 3). DevICU was significantly decreased in the FS-LASIK MCG group 1 day postoperatively (P = 0.005). DevICU showed no significant intergroup difference.
Lipid layer assessment after moisture chamber goggles treatment at postoperative 1 day, 1 week, and 1 month. A AvgICU of control and MCG groups in SMILE participants; B AvgICU of control and MCG groups in FS-LASIK participants; C DevICU of control and MCG groups in SMILE participants; D DevICU of control and MCG groups in FS-LASIK participants. *p < 0.05, independent student’s t-test. AvgICU, average lipid layer thickness in interferometric color units; DevICU, deviation in lipid layer thickness in interferometric color units; MCG, moisture chamber goggles; SMILE, small-incision lenticule extraction; FS-LASIK, femtosecond laser-assisted in situ keratomileusis; PreOp, preoperative; Po, postoperative; NS, not significant
Higher-order aberrations
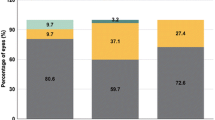
Postoperative HOA significant decrease compared to preoperative in both SMILE and FS-LASIK groups (Tables 2 and 3). In FS-LASIK participants, the MCG group had significantly lower total HOAs, as well as coma levels 1 day (total HOAs, P = 0.023; coma, P = 0.004) and 1 week (total HOAs, P = 0.010, coma, P = 0.004) after surgery compared to the control group (Fig. 4). No significant intergroup difference was observed in SMILE participants postoperatively.
Higher-order aberrations evaluation after moisture chamber goggles treatment at postoperative 1 day, 1 week, and 1 month. A Total HOA of control and MCG groups in SMILE participants; B Total HOA of control and MCG groups in FS-LASIK participants; C Coma of control and MCG groups in SMILE participants; D Coma of control and MCG groups in FS-LASIK participants. *p < 0.05, **p < 0.01, independent student’s t-test. HOA, higher-order aberrations; MCG, moisture chamber goggles; SMILE, small-incision lenticule extraction; FS-LASIK, femtosecond laser-assisted in situ keratomileusis; PreOp, preoperative; Po, postoperative; NS, not significant
Ocular surface disease index
A significant increase in OSDI was observed in the FS-LASIK control group (P = 0.020), but not in the FS-LASIK MCG group (P = 0.200), or SMILE control (P = 0.265) and MCG (P = 0.663) groups (Tables 2 and 3). No statistically significant intergroup difference was observed in OSDI in either SMILE or FS-LASIK groups (Fig. 5).
Ocular surface disease index after moisture chamber goggles treatment at postoperative 1 day, 1 week, and 1 month. A OSDI of control and MCG groups in SMILE participants; B OSDI of control and MCG groups in FS-LASIK participants. Independent student’s t-test for comparisons between control and MGC groups. OSDI, ocular surface disease index; SMILE, small-incision lenticule extraction; FS-LASIK, femtosecond laser-assisted in situ keratomileusis; PreOp, preoperative; Po, postoperative; NS, not significant
Discussion
To reduce the incidence and severity of refractive surgery-related DED, a comprehensive management approach throughout the perioperative period is needed. The current consensus recommended that both the preoperative identification and treatment of DED, and postoperative tear replacement, tear conservation, and anti-inflammation therapies, should be implemented [1, 9]. The TFOS DEWS II reports have recommended the use of MCGs for tear conservation, as they can slow tear evaporation by increasing local humidity and minimizing airflow [9]. A number of studies have investigated MCGs’ short-term efficacy in DED patients, as well as in patients exposed to adverse environments [11,12,13]. However, further evidence is required for the long-term efficacy of MCGs in DED patients, and their efficacy in refractive surgery-related DED. This study is the first to investigate the long-term effects of MCG on the DED parameters and visual outcomes in participants receiving refractive surgery.
Our results demonstrate that MCG treatment effectively conserved tear and stabilized the postoperative tear film. TMH was significantly higher in the MCG group compared to control 1 week and 1 month postoperatively in SMILE participants, and 1 day in FS-LASIK participants. Despite the lack of statistical significance, TMH was generally higher in the MCG groups in both SMILE and FS-LASIK participants. Previous studies reported a significant increase in TMH after the application of moisture chamber goggles [11, 12]. By maintaining a higher level of humidity inside the chambers, MCG effectively decreased the evaporation of the tear film.
In both SMILE and FS-LASIK control groups, NIBUT at postoperative 1 day postoperative decreased significantly compared to preoperatively, but not in the corresponding MCG groups. This is consistent with previous observations that MCG can elongate BUT and stabilize the tear film [12]. In the FS-LASIK control group, the decrease in NIBUT persisted 1 month after surgery, possibly due to the more significant corneal subbasal nerve dysfunction and ocular surface inflammation [3, 19]. However, this effect was reversed by MCG treatment, and a longer NIBUT was maintained in the FS-LASIK MCG group.
MCG can ameliorate conjunctival congestion after refractive surgery. The congestion scores were generally lower in the MCG groups compared to the control groups. The effect of MCG on the lipid layer of the tear film is less clear. Average LLT was significantly lower in the FS-LASIK MCG group 1 week postoperatively. No significant trend in the homogeneity of lipid layer distribution was observed. As MCG mainly inhibit the evaporation of the tear film, they are less likely to affect the lipid layer. A previous study on MCG with heating functions showed that increased temperature can lead to increased LLT [11]. Further studies are required to clarify the effects of MCG on the lipid contents in the tear film.
A significant decrease in total HOA was observed after both SMILE and FS-LASIK surgery and further improved by the use of the MCG. In the FS-LASIK MCG group, total HOA was significantly lower compared to the control group, at 1 day and 1 week after surgery. Previous studies have demonstrated that DED was associated with increased HOAs and poor visual quality and that DED interventions have led to improvement in both tear film stability and HOAs [20, 21]. This is consistent with our findings that improvements in NIBUT, TMH, and HOAs were observed in tandem after treatment with MCG.
The postoperative OSDI scores were generally lower in the MCG groups compared to the control, despite the lack of statistical significance. This demonstrates that the use of MCG can ameliorate postoperative discomfort in both SMILE and FS-LASIK recipients. In addition, a significant increase in OSDI scores was observed in the FS-LASIK control group, reflecting a higher level of discomfort induced by this surgery. This observation was consistent with previous reports that SMILE was associated with less postoperative discomfort than FS-LASIK [3, 5].
This is the first study investigating the efficacy of MCG on DED after refractive surgery. Previous studies mainly focused on the short term effects of MCG, making this study an important addition to current knowledge on the effects of moisture chamber goggles. This study uses non-invasive techniques for tear film evaluations, thereby reducing the disturbance of tear film during examinations. This study has a few important limitations. The variance in NIBUT and LLT is large, despite repeated examinations. However, this variation was consistent with previous reports [18]. Our study was conducted in the span of a year. The changes in temperature and humidity might have contributed to the variation in the results. However, the DED evaluations were conducted in an air-conditioned room, reducing the variations in temperature and humidity. In addition, potential bias might originated from differences in participants’ life styles, such as screen usage, near-work activities, cosmetics, and nutrition, etc.[22]. Future studies of DED should take lifestyle variations into consideration, and investigate potential interactions between lifestyle and the disease. Another limitation is the small sample size. However, the sample size in our study was comparable with previous reports evaluating the effects of MCG [11,12,13]. Future research with a larger cohort and a better-controlled environment is required to further evaluate the efficacy of MCG.
In conclusion, our results demonstrated the efficacy of MCG in refractive surgery-related DED. MCG usage effectively slowed tear evaporation, increased tear film stability, improved HOAs, and potentially reduced postoperative inflammation and discomfort in patients receiving SMILE and LASIK surgeries. MCG is a promising adjuvant therapy in the comprehensive management of refractive surgery-related DED.
Availability of data and materials
The datasets supporting the conclusions of this article are available upon request to the corresponding author.
Abbreviations
- DED:
-
Dry eye disease
- MGC:
-
Moisture chamber goggle
- SMILE:
-
Small-incision lenticule extraction
- FS-LASIK:
-
Femtosecond laser-assisted in situ keratomileusis
- HOA:
-
Higher-order aberration
- NIBUT:
-
Non-invasive tear film break-up time
- TMH:
-
Tear meniscus height
- LLT:
-
Lipid layer thickness
- OSDI:
-
Ocular surface disease index
- TFOS:
-
Tear Film and Ocular Surface
- DEWS:
-
Dry Eye Workshop
- PUMCH:
-
Peking Union Medical College Hospital
- SE:
-
Spherical equivalent
- ACD:
-
Anterior chamber depth
- LogMAR:
-
Logarithm of the minimal angle of resolution
- BCVA:
-
Best corrected visual acuity
- UCVA:
-
Uncorrected visual acuity
- IOP:
-
Intraocular pressure
- ICU:
-
Interferometric color unit
- AvgICU:
-
Average lipid layer thickness in interferometric color unit
- MaxICU:
-
Maximal lipid layer thickness in interferometric color unit
- MinICU:
-
Minimal lipid layer thickness in interferometric color unit
- DevICU:
-
Deviation in lipid layer thickness in interferometric color unit
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
References
Gomes JAP, Azar DT, Baudouin C, Efron N, Hirayama M, Horwath-Winter J, Kim T, Mehta JS, Messmer EM, Pepose JS, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511–38.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–83.
Denoyer A, Landman E, Trinh L, Faure J-F, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015;122(4):669–76.
Ma KK, Manche EE. Corneal sensitivity and patient-reported dry eye symptoms in a prospective randomized contralateral-eye trial comparing laser in situ keratomileusis and small incision lenticule extraction. Am J Ophthalmol. 2022;241:248–53.
Recchioni A, Sisó-Fuertes I, Hartwig A, Hamid A, Shortt AJ, Morris R, Vaswani S, Dermott J, Cerviño A, Wolffsohn JS, et al. Short-term impact of FS-LASIK and SMILE on dry eye metrics and corneal nerve morphology. Cornea. 2020;39(7):851–7.
Shen Z, Zhu Y, Song X, Yan J, Yao K. Dry eye after small incision lenticule extraction (SMILE) versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia: a meta-analysis. PLoS ONE. 2016;11(12): e0168081.
Toda I. Dry eye after LASIK. Invest Ophthalmol Vis Sci. 2018;59(14):DES109–15.
**g D, Liu Y, Chou Y, Jiang X, Ren X, Yang L, Su J, Li X. Change patterns in the corneal sub-basal nerve and corneal aberrations in patients with dry eye disease: an artificial intelligence analysis. Exp Eye Res. 2022;215:108851.
Jones L, Downie LE, Korb D, Benitez-Del-Castillo JM, Dana R, Deng SX, Dong PN, Geerling G, Hida RY, Liu Y, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575–628.
Chinese Branch of the Asian Dry Eye S, Ocular S, Tear Film Diseases Group of Ophthalmology Committee of Cross-Straits Medicine Exchange A, Ocular S, Dry Eye Group of Chinese Ophthalmologist A. Expert consensus on dry eye in China: dry eye related to eye surgery (2021). Zhonghua Yan Ke Za Zhi. 2021;57(8):564–72.
Ren Y, Chen J, Zheng Q, Chen W. Short-term effect of a developed warming moist chamber goggle for video display terminal-associated dry eye. BMC Ophthalmol. 2018;18(1):33.
Shen G, Qi Q, Ma X. Effect of moisture chamber spectacles on tear functions in dry eye disease. Optom Vis Sci. 2016;93(2):158–64.
Zhou Y, Liu J, Cui Y, Zhu H, Lu Z. Moisture chamber versus lubrication for corneal protection in critically ill patients: a meta-analysis. Cornea. 2014;33(11):1179–85.
Cortese D, Capp L, McKinley S. Moisture chamber versus lubrication for the prevention of corneal epithelial breakdown. Am J Crit Care. 1995;4(6):425–8.
Expert consensus on the diagnosis and treatment of dry eye during perioperative period of corneal refractive surgery in China (2021). [Zhonghua Yan Ke Za Zhi] Chin J Ophthalmol 2021;57(9):644–650.
Expert consensus on dry eye in China: dry eye related to eye surgery (2021). [Zhonghua Yan Ke Za Zhi] Chin J Ophthalmol 2021;57(8):564–572.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, Gupta PK, Karpecki P, Lazreg S, Pult H, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539–74.
Singh S, Srivastav S, Modiwala Z, Ali MH, Basu S. Repeatability, reproducibility and agreement between three different diagnostic imaging platforms for tear film evaluation of normal and dry eye disease. Eye (Lond). 2023;37(10):2042–7.
Zhao J, Li Y, Yu T, Wang W, Emmanuel MT, Gong Q, Hu L. Anterior segment inflammation and its association with dry eye parameters following myopic SMILE and FS-LASIK. Ann Med. 2023;55(1):689–95.
Koh S. Irregular Astigmatism and Higher-Order Aberrations in Eyes With Dry Eye Disease. Invest Ophthalmol Vis Sci. 2018;59(14):DES36–40.
Rhee J, Chan TC, Chow SS, Di Zazzo A, Inomata T, Shih KC, Tong L. A systematic review on the association between tear film metrics and higher order aberrations in dry eye disease and treatment. Ophthalmol Ther. 2022;11(1):35–67.
Craig JP, Alves M, Wolffsohn JS, Downie LE, Efron N, Galor A, et al. TFOS lifestyle report executive summary: a lifestyle epidemic - Ocular surface disease. Ocul Surf. 2023;30:240–53.
Acknowledgements
We would like to thank Yumei ** and Lei Sun from the Ophthalmology Department, Peking Union Medical College Hospital, for their support in data collection; and extend our sincere gratitude to all the patients for their participation in this study.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 82000863), National High Level Hospital Clinical Research Funding (Grant No. 2022-PUMCH-A-198) and Young Scholarship Program of Peking Union Medical College Hospital (Grant No. pumch201910845).
Author information
Authors and Affiliations
Contributions
TZH and YCW devised the idea and designed the study. TZH analyzed the data and wrote the manuscript. ZZ and QYW participated in study management and collected the data. DC and YL supervised the study and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Ethics Board of Peking Union Medical College and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from the participants of this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, T., Wang, Y., Zhu, Z. et al. Moisture chamber goggles for the treatment of postoperative dry eye in patients receiving SMILE and FS-LASIK surgery. BMC Ophthalmol 23, 501 (2023). https://doi.org/10.1186/s12886-023-03241-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03241-4