Abstract
Background
Postoperative delirium (POD) is an important complication for older patients and recent randomised controlled trials have showed a conflicting result of the effect of deep and light anesthesia.
Methods
We included randomised controlled trials including older adults that evaluated the effect of anesthetic depth on postoperative delirium from PubMed, Embase, Web of Science and Cochrane Library. We considered deep anesthesia as observer’s assessment of the alertness/ sedation scale (OAA/S) of 0–2 or targeted bispectral (BIS) < 45 and the light anesthesia was considered OAA/S 3–5 or targeted BIS > 50. The primary outcome was incidence of POD within 7 days after surgery. And the secondary outcomes were mortality and cognitive function 3 months or more after surgery. The quality of evidence was assessed via the grading of recommendations assessment, development, and evaluation approach.
Results
We included 6 studies represented 7736 patients aged 60 years and older. We observed that the deep anesthesia would not increase incidence of POD when compared with the light anesthesia when 4 related studies were pooled (OR, 1.40; 95% CI, 0.63–3.08, P = 0.41, I2 = 82%, low certainty). And no significant was found in mortality (OR, 1.12; 95% CI, 0.93–1.35, P = 0.23, I2 = 0%, high certainty) and cognitive function (OR, 1.13; 95% CI, 0.67–1.91, P = 0.64, I2 = 13%, high certainty) 3 months or more after surgery between deep anesthesia and light anesthesia.
Conclusions
Low-quality evidence suggests that light general anesthesia was not associated with lower POD incidence than deep general anesthesia. And High-quality evidence showed that anesthetic depth did not affect the long-term mortality and cognitive function.
Systematic review registration
CRD42022300829 (PROSPERO).
Similar content being viewed by others
Introduction
It is well acknowledged that the older adults were more vulnerable to postoperative delirium (POD) and resulted in loss of autonomy and mortality [1]. Though the risk factors of POD were identified such as aged, ASA physical status > 2, Charlson Comorbidity Index > 2 and Mini-Mental State Examination, the drug or anesthetic interventions to reduce POD incidence remains uncertain [2].
In the past decade, electroencephalography-guided general anesthesia was considered a promising method to reduce POD incidence [3]. The essence is to avoid excessive general anesthesia intraoperatively. Evered et al. has reported that targeting light anesthesia (targeted bispectral (BIS) index 50) reduced the risk of POD [4]. However, Wildes et al. suggested EEG-guided anesthetic administration, did not decrease the incidence of POD [4, 5]. Similarly, previously meta-analysis has showed the contrary results of the outcomes of deep anesthesia on POD [6, 7]. These conflicting results mainly due to the difference in duration of excessive general anesthesia exposure and there are different definitions of light/deep anesthesia among these investigations. This limits the possibility of clinical application.
Therefore, we conducted this systematic review and meta-analysis, to provide the latest clinical evidences whether anesthetic depth was associated with the incidence of POD in older patients.
Methods
This systematic review and meta-analysis was followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines standards and the review protocol has registered with PROSPERO (Systematic review registration: CRD42022300829).
Eligibility criteria
Studies
We included published articles that enrolled patients were randomly divided into light anesthesia and deep anesthesia groups via BIS or observer’s assessment of the alertness/ sedation scale (OAA/S). Eligible studies were all randomized controlled trials (RCTs), case reports and observation studies were excluded. Studies which designed to compare the difference between processed electroencephalography monitoring and usual care were excluded in our study.
Participants
In consideration of older adults were more vulnerable to POD, we included original studies that reported on patients aged 60 years and older and plan to undergo selective operation.
Interventions
It is important to unify the definitions of light and deep anesthesia. Previously study has defined BIS ranged 50–60 as light anesthesia while 30–40 as deep anesthesia [8]. In addition, Short et al. suggested BIS targeted 50 as light and BIS targeted 35 as deep anesthesia based on based on large-scale observational data and close to the first and third quartiles for mean BIS recorded in an audit of a large tertiary hospital’s anesthetic database [9]. Generally, the recommended BIS ranges are 40–60 for general anesthesia. In this light, in our study, we considered deep anesthesia as modified OAA/S of 0–2 or targeted BIS < 45 intraoperatively regardless of whether combined with spinal anesthesia. As well, the light anesthesia was considered OAA/S 3–5 or targeted BIS > 50.
Comparison groups
We included studies which a comparison group received light anesthesia. Correspondingly, the light anesthesia was defined as OAA/S of 3–5 or targeted BIS > 50 intraoperatively regardless of whether combined with spinal anesthesia.
Outcomes
The primary outcome was incidence of POD within 7days after surgery. And the secondary outcomes were mortality and cognitive function 3 months or more after surgery.
Study selection and data extraction
Search strategy
A systematic search was conducted on studies published from inception to Dec 31 2021, with no restrictions on language of publication in PubMed, Embase, Web of Science and Cochrane Library by two independently researchers. Records were managed by EndNote X9.3 software to exclude duplicates. Search Strategy and keywords for these databases were described in supplementary materials.
Study selection and data extraction
Two independently investigators (Y.W and H.Z) screened Titles, abstracts, and full-text articles and assessed for their suitability and checked by the third researcher F.X. The disputed part was decided by F.X or by consensus. The data were extracted into a Microsoft Excel spreadsheet by one investigator (Y.W) and checked by S.Z. For the meta-analysis, collected data included: (1) first author, published year and country; (2) patient population characteristics; (3) surgery types; (4) outcome measures used; (5) the light/deep anesthesia targets and the sedation level in practice.
Quality assessment
We used Cochrane Risk of Bias 2.0 tool to evaluate the quality of the included studies by two investigators independently(Y.D and S.Z) [10]. Grading Recommendations Assessment, Development and Evaluation (GRADE) was used to assessed the overall certainty of evidence for primary and secondary outcomes [11]. We used the Guideline Development Tool (https://www.gradepro.org) to formulate the summary of findings table. The disputed part was solved by consensus.
Statistical analysis
All analysis was performed using Review Manager 5.4 (The Cochrane Collaboration) software. Heterogeneity among studies was examined through Cochran Q test and the I2 index (I2 > 50% for extensive heterogeneity). If heterogeneity was low (I2 < 50%), the fixed-effect model (Mantel-Haenszel method) was chosen to assess combined effects; otherwise, a random-effect model (Mantel-Haenszel method) was utilized. And P < 0.05 was considered to indicate statistical significance.
Results
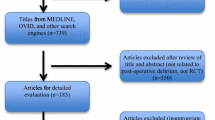
We identified 339 RCTs after literature search and added 1 RCT which was identified through citation search. Subsequently, we screened 212 abstracts and identified 21 studies as requiring full-article review. Among these, 15 were excluded with reasons and 6 studies met the inclusion criteria for the review. The steps of the literature search, study selection and reasons for exclusion was shown in Fig. 1.
Study characteristics and quality
The included 6 studies for the systematic review represented 7736 patients aged above 60 years old. All these studies were RCTs. Among these, 4 RCTs (66.7%) reported the comparation of POD incidences between light and deep anesthesia [4, 8, 12, 13] and 3 RCTs (50.0%) examined the mortality three months or more after surgery [8, 14, 15]. However, we found these studies differed significantly in type of surgery, assessment of anesthesia depth and methods for evaluating POD. Four RCTs [4, 8, 13, 14] used BIS and 2 RCTs [12, 15] used OAA/S score to evaluate the anesthesia depth. In addition, the intraoperative sedation levels were assessed in these 6 studies and actual levels of sedation were met corresponding targets (Table 1).
As shown in Fig. 2, the overall risk of bias as assessed by the Cochrane was low in 5 studies [4, 12,13,14,15], the risk of selection and reporting bias was unclear in 1 study8, and risk of attrition bias was high in one study8.
Primary outcome
Four trails ( N = 892) compared the POD incidence in deep and light anesthesia groups [4, 8, 12, 13]. Among them, 3 studies (N = 792) [4, 8, 13] utilized targeted BIS to assess the sedative level while 1 study (N = 200) [12] used OAA/S. Meta-analysis showed that the deep anesthesia would not increase incidence of POD when compared with the light anesthesia(OR, 1.40; 95% CI, 0.63–3.08, P = 0.41, I2 = 82%, low certainty) (Tables 2 and Fig. 3). We subsequently performed a sensitivity analysis in order to determine whether single studies included affected the overall statistical effect. However, when omitted Quan et al. [8], the overall results showed a significant decreased incidence of POD in light anesthesia group (OR, 1.96; 95% CI, 1.05–3.65, P = 0.03, I2 = 66%).
We next examined whether the methods of sedative assessments could influence the POD incidence. As shown in Fig. 3, there were no differences between the deep anesthesia and light anesthesia in POD incidence in studies used BIS (OR, 1.47; 95% CI, 0.42–5.12, P = 0.54, I2 = 88%).
Moreover, it was reported that the incidence of POD is associated with surgery types [16], due to the 4 studies draw conclusions from multiple procedures [4, 8, 12, 13], we intend to investigate the difference between major (lasting 2 h or more) and minor (lasting within 2 h) surgeries. As a result, 3 studies were included in analysis and our pooled data indicate that there were no differences between the deep anesthesia and light anesthesia in POD incidence in major surgeries (OR, 1.47; 95% CI, 0.42–5.12, P = 0.54, I2 = 88%) [4, 8, 13].
Secondary outcomes
Three studies of 628 patients reported the postoperative cognitive dysfunction incidence 3 months after surgery [3, 8, 15]. Similarly, the results showed no difference of postoperative cognitive dysfunction incidence at 3 months within deep anesthesia and light anesthesia (OR, 1.13; 95% CI, 0.67–1.91, P = 0.64, I2 = 13%, high certainty) (Tables 2 and Fig. 4). However, we could not identify enough studies to perform the further analysis at 12 months.
Three studies of 6949 patients assessed long-term mortality between deep anesthesia and light anesthesia [8, 14, 15]. It revealed no significant difference among two groups (OR, 1.12; 95% CI, 0.93–1.35, P = 0.23, I2 = 0%, high certainty) (Tables 2 and Fig. 5).
Discussions
This systematic review and meta-analysis suggested that light anesthesia would not decrease the incidence of POD when compared with the deep anesthesia in older adults. And this was consistent with mortality and cognitive function 3 months or more after surgery.
POD is an important complication for older patients and the incidence of POD varies between 22% and 50% [17, 18]. Up to now, evidences on the perioperative interventions such as use of anti-psychotics and other medications, intravenous versus inhalational maintenance of anesthesia in the management of POD are still inconclusive [19, 20]. Interestingly, Luo et al. have suggested that POD may relate to the dose of anesthesia drugs used during surgery [21]. Consequently, reducing the dose of anesthetic drugs may be considerable strategies to decreased the incidence of POD for older patients. Previous meta-analysis addressing depth of anesthesia and POD have compared deep anesthesia (target BIS range 30–50) versus light anesthesia (target BIS range 46–80), and have yielded inconclusive results [6, 7]. Such as Lu et al. enrolled 4 RCTs including 340 patients and found that no significant correlation between the depth of anesthesia and POD [7]. While another meta-analysis by Li and colleagues draw a conclusion that light anesthesia was associated with a decrease in POD in comparison with deep anesthesia after evidence synthesis of 10 studies (3142 patients) [6]. This contradictory conclusion in the effect of light anesthesia on the incidence of POD mainly caused by the differences in study designs such as different duration of excessive general anesthesia exposure and targes of light/deep anesthesia. For example, the BIS value of a light anesthesia group was 49.90 ± 13.50 may similar to a deep anesthesia target in another [22, 23].
Our results suggested that light anesthesia would not decrease the incidence of POD when compared with the deep anesthesia in older adults. Major strengths of our study include controlling the range of light/deep anesthesia and identified study population. Moreover, all RCTs enrolled in analysis reported the sedation level of two groups in practice, the actual sedation levels and duration mostly conform to the range designed and differed little among these studies. Though the European Society of Anesthesiologists the American Geriatric Society, and the UK’s National Institute for Health and Care Excellence all recommend that prevent excessive anesthetic administration to patients at high risk of POD via intraoperative EEG monitoring [24,25,26]. Consistent with our findings, the ENGAGES trial found among older adults undergoing major surgery, EEG-guided anesthetic administration (mean to avoid excessive general anesthesia), compared with usual care, did not decrease the incidence of postoperative delirium [5]. And regional anesthesia without sedation did not significantly reduce the incidence of postoperative delirium compared with general anesthesia [27]. Interestingly, it was reported that the degree of POD may associate with EEG [28]. However, none of included studies provided the information about the severity delirium. Whether the depth of anesthesia has an effect on the degree of delirium remains undetermined. As for mortality and cognitive function 3 months or more after surgery, our pooled data showed no significant difference in light or deep general anesthesia.
Importantly, “deep anesthesia” as well as “light anesthesia” is metaphorically apt.
but quantitatively hollow [25]. So far, the clear definition of deep or light anesthesia is still lacking. The BALANCED Anesthesia Study was defined deep anesthesia as targeted BIS 35 and light anesthesia as targeted BIS 50 on the basis of previous large RCTs [14]. It is reported that the BIS targets chosen were based on large-scale observational data and were close to the first and third quartiles for mean BIS recorded in an audit of a large tertiary hospital’s anesthetic database [9, 14]. However, in our study, to include RCTs with comparable sedation intervention as possible, we chose targeted BIS < 45 as deep anesthesia and targeted BIS > 50 as light anesthesia. And we further confirmed the BIS levels were actually achieved as the target level in respective studies to ensure the reliability of our conclusions. Furthermore, the OAA/S was considered accurately reflect the clinical picture and it was reported OAA/S correlated well with BIS [29]. So that studies used OAA/S to evaluate anesthesia depth were included in the analysis.
Our study had several limitations. Firstly, only 4 RCTs in our analysis were powered to detect a difference in POD and there was significant heterogeneity of the included trials. Subsequently, we have performed several subgroup analyses and the exact reason of the observed heterogeneity was not identified. It was reported that the incidence of POD varies greatly among different types of surgery: 6%~46% in cardiac surgery [30], 5%~39% in vascular surgery [31], 8%~54% in gastrointestinal surgery [32]. And this may contribute to a high heterogeneity. Though most studies clarified their valid assessments (consensus/3D-CAM) and investigators (trained/masked researcher or experienced psychometrician), the variety of diagnostic methods undoubtedly contributed to the heterogeneity. Moreover, when we performed the sensitive analysis, the results showed an inconsistent result as the incidence of POD between light/deep anesthesia. Therefore, the results of effects of anesthetic depth on POD in older adults must be undertaken with caution and further large multicenter RCTs are needed. Secondly, as reported, deep anesthesia may increase postoperative mortality in cardiac surgery patients rather than non-cardiac surgery patients. In our study, we were failed to investigate whether the specific groups populations or surgical types were benefited from light anesthesia due to lack of corresponding literature. Thirdly, in case of the exact definitions of deep/light anesthesia are still lacking, the effect of gradients of anesthesia depth on POD should be examined.
Conclusions
In conclusion, current data showed no difference between deep anesthesia and light anesthesia in the incidence of POD as well as mortality and cognitive function 3 months or more after surgery. However, since the total number of included RCTs was low, more multicenter RCTs with gradient anesthesia depth ranges are needed to validate this finding before clinical application in the future.
Data Availability
The data used to support the findings of this study are included within the article.
Abbreviations
- BIS:
-
Bispectral
- OAA/S:
-
Observer’s assessment of the alertness/sedation scale
- POD:
-
Postoperative delirium
- RCTs:
-
Randomized controlled trials
References
Deeken F, Sanchez A, Rapp MA, Denkinger M, Brefka S, Spank J, Bruns C, von Arnim CAF, Kuster OC, Conzelmann LO, et al. Outcomes of a Delirium Prevention Program in older persons after elective Surgery: a stepped-Wedge Cluster Randomized Clinical Trial. JAMA Surg. 2022;157(2):e216370.
Mevorach L, Forookhi A, Farcomeni A, Romagnoli S, Bilotta F. Perioperative risk factors associated with increased incidence of postoperative delirium: systematic review, meta-analysis, and Grading of recommendations Assessment, Development, and evaluation system report of clinical literature. Br J Anaesth 2022.
Punjasawadwong Y, Chau-In W, Laopaiboon M, Punjasawadwong S, Pin-On P. Processed electroencephalogram and evoked potential techniques for amelioration of postoperative delirium and cognitive dysfunction following non-cardiac and non-neurosurgical procedures in adults. Cochrane Database Syst Rev. 2018;5:CD011283.
Evered LA, Chan MTV, Han R, Chu MHM, Cheng BP, Scott DA, Pryor KO, Sessler DI, Veselis R, Frampton C, et al. Anaesthetic depth and delirium after major Surgery: a randomised clinical trial. Br J Anaesth. 2021;127(5):704–12.
Wildes TS, Mickle AM, Ben Abdallah A, Maybrier HR, Oberhaus J, Budelier TP, Kronzer A, McKinnon SL, Park D, Torres BA, et al. Effect of Electroencephalography-Guided Anesthetic Administration on Postoperative Delirium among older adults undergoing major Surgery: the ENGAGES Randomized Clinical Trial. JAMA. 2019;321(5):473–83.
Li Y, Zhang B. Effects of anesthesia depth on postoperative cognitive function and inflammation: a systematic review and meta-analysis. Minerva Anestesiol. 2020;86(9):965–73.
Lu X, ** X, Yang S, **a Y. The correlation of the depth of anesthesia and postoperative cognitive impairment: a meta-analysis based on randomized controlled trials. J Clin Anesth. 2018;45:55–9.
Quan C, Chen J, Luo Y, Zhou L, He X, Liao Y, Chou J, Guo Q, Chen AF, Wen O. BIS-guided deep anesthesia decreases short-term postoperative cognitive dysfunction and peripheral inflammation in elderly patients undergoing abdominal Surgery. Brain and Behavior. 2019;9(4):e01238.
Short TG, Leslie K, Chan MT, Campbell D, Frampton C, Myles P. Rationale and design of the Balanced Anesthesia Study: a prospective Randomized Clinical Trial of two levels of anesthetic depth on patient outcome after major Surgery. Anesth Analg. 2015;121(2):357–65.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical Research ed). 2011;343:d5928.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ. Group GW: GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical Research ed). 2008;336(7650):924–6.
Sieber FE, Neufeld KJ, Gottschalk A, Bigelow GE, Oh ES, Rosenberg PB, Mears SC, Stewart KJ, Ouanes JP, Jaberi M, et al. Effect of depth of Sedation in older patients undergoing hip fracture repair on postoperative delirium: the STRIDE Randomized Clinical Trial. JAMA Surg. 2018;153(11):987–95.
Valentin LS, Pereira VF, Pietrobon RS, Schmidt AP, Oses JP, Portela LV, Souza DO, Vissoci JR, Luz VF, Trintoni LM, et al. Effects of single low dose of Dexamethasone before Noncardiac and nonneurologic Surgery and General Anesthesia on postoperative cognitive Dysfunction-A phase III double Blind, Randomized Clinical Trial. PLoS ONE. 2016;11(5):e0152308.
Short TG, Campbell D, Frampton C, Chan MTV, Myles PS, Corcoran TB, Sessler DI, Mills GH, Cata JP, Painter T, et al. Anaesthetic depth and Complications after major Surgery: an international, randomised controlled trial. Lancet (London England). 2019;394(10212):1907–14.
Sieber F, Neufeld KJ, Gottschalk A, Bigelow GE, Oh ES, Rosenberg PB, Mears SC, Stewart KJ, Ouanes JP, Jaberi M, et al. Depth of sedation as an interventional target to reduce postoperative delirium: mortality and functional outcomes of the strategy to reduce the incidence of postoperative delirium in Elderly patients randomised clinical trial. Br J Anaesth. 2019;122(4):480–9.
Igwe EO, Nealon J, O’Shaughnessy P, Bowden A, Chang HR, Ho MH, Montayre J, Montgomery A, Rolls K, Chou KR, et al. Incidence of postoperative delirium in older adults undergoing surgical procedures: a systematic literature review and meta-analysis. Worldviews Evid Based Nurs. 2023;20(3):220–37.
Chuan A, Zhao L, Tillekeratne N, Alani S, Middleton PM, Harris IA, McEvoy L, Ni Chroinin D. The effect of a multidisciplinary care bundle on the incidence of delirium after hip fracture Surgery: a quality improvement study. Anaesthesia. 2020;75(1):63–71.
Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–22.
Igwe EO, Nealon J, Mohammed M, Hickey B, Chou KR, Chen KH, Traynor V. Multi-disciplinary and pharmacological interventions to reduce post-operative delirium in elderly patients: a systematic review and meta-analysis. J Clin Anesth. 2020;67:110004.
Miller D, Lewis SR, Pritchard MW, Schofield-Robinson OJ, Shelton CL, Alderson P, Smith AF. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac Surgery. Cochrane Database Syst Rev. 2018;8(8):CD012317.
Luo C, Zou W. Cerebral monitoring of anaesthesia on reducing cognitive dysfunction and postoperative delirium: a systematic review. J Int Med Res. 2018;46(10):4100–10.
Sieber FE, Zakriya KJ, Gottschalk A, Blute MR, Lee HB, Rosenberg PB, Mears SC. Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin Proc. 2010;85(1):18–26.
Shu AH, Wang Q, Chen XB. Effect of different depths of anesthesia on postoperative cognitive function in laparoscopic patients: a randomized clinical trial. Curr Med Res Opin. 2015;31(10):1883–7.
American Geriatrics Society Expert Panel on Postoperative Delirium in Older A. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc. 2015;63(1):142–50.
Smith D, Andrzejowski J, Smith A. Certainty and uncertainty: NICE guidance on ‘depth of anaesthesia’ monitoring. Anaesthesia. 2013;68(10):1000–5.
Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A, Cherubini A, Jones C, Kehlet H, MacLullich A, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34(4):192–214.
Li T, Li J, Yuan L, Wu J, Jiang C, Daniels J, Mehta RL, Wang M, Yeung J, Jackson T, et al. Effect of Regional vs General Anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture Surgery: the RAGA Randomized Trial. JAMA. 2022;327(1):50–8.
Guay CS, Kafashan M, Huels ER, Jiang Y, Beyoglu B, Spencer JW, Geczi K, Apakama G, Ju YS, Wildes TS, et al. Postoperative Delirium Severity and Recovery Correlate with Electroencephalogram Spectral features. Anesth Analg. 2023;136(1):140–51.
Glass PS, Bloom M, Kearse L, Rosow C, Sebel P, Manberg P. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology. 1997;86(4):836–47.
Crocker E, Beggs T, Hassan A, Denault A, Lamarche Y, Bagshaw S, Elmi-Sarabi M, Hiebert B, Macdonald K, Giles-Smith L, et al. Long-Term effects of postoperative delirium in patients undergoing Cardiac Operation: a systematic review. Ann Thorac Surg. 2016;102(4):1391–9.
Oldroyd C, Scholz AFM, Hinchliffe RJ, McCarthy K, Hewitt J, Quinn TJ. A systematic review and meta-analysis of factors for delirium in vascular surgical patients. J Vasc Surg. 2017;66(4):1269–1279e1269.
Scholz AF, Oldroyd C, McCarthy K, Quinn TJ, Hewitt J. Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal Surgery. Br J Surg. 2016;103(2):e21–2.
Acknowledgements
Not Applicable.
Funding
This study was supported by the National Natural Science Foundation (82071251), National Key Research and Development Program of China (2018YFC2001802) and Hubei Province Key Research and Development Program (2021BCA145).
Author information
Authors and Affiliations
Contributions
Study conception/design: Y.W and X.C; Data acquisition: Y.W, and H.Z; Data analysis: Y.W, F.X and S.Z; Writing paper: Y.W, Y.D, H.Z and F.X; Revising paper: All authors; All authors approved the final version of the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Zhu, H., Xu, F. et al. The effect of anesthetic depth on postoperative delirium in older adults: a systematic review and meta-analysis. BMC Geriatr 23, 719 (2023). https://doi.org/10.1186/s12877-023-04432-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04432-w