Abstract
Glioblastomas remain the most lethal primary brain tumors. Natural killer (NK) cell-based therapy is a promising immunotherapeutic strategy in the treatment of glioblastomas, since these cells can select and lyse therapy-resistant glioblastoma stem-like cells (GSLCs). Immunotherapy with super-charged NK cells has a potential as antitumor approach since we found their efficiency to kill patient-derived GSLCs in 2D and 3D models, potentially reversing the immunosuppression also seen in the patients. In addition to their potent cytotoxicity, NK cells secrete IFN-γ, upregulate GSLC surface expression of CD54 and MHC class I and increase sensitivity of GSLCs to chemotherapeutic drugs. Moreover, NK cell localization in peri-vascular regions in glioblastoma tissues and their close contact with GSLCs in tumorospheres suggests their ability to infiltrate glioblastoma tumors and target GSLCs. Due to GSLC heterogeneity and plasticity in regards to their stage of differentiation personalized immunotherapeutic strategies should be designed to effectively target glioblastomas.
Similar content being viewed by others
Introduction
Glioblastomas (gliomas WHO grade IV; GBMs) remain among the most aggressive malignancies of the brain, with no or little progress in the standard treatment for nearly 20 years. Only 5% of the patients survive 5 years or more and only half of the patients are still alive at 15 months after diagnosis1,2. Cancer cells with self-renewing properties, named GBM stem-like cells (GSLCs), propagate GBMs and express stemness markers3,4. GSLCs are resistant to standard therapy due to efficient DNA repair mechanisms and multidrug resistance causing regrowth of GBM tumors4,5. Moreover, GSLC ability to evade immunosurveillance4 and immunosuppressive GBM microenvironment prevent efficiency of checkpoint blockade and CAR T cell approaches in GBM therapy6,7.
Natural killer (NK) cells are large granular and cytotoxic lymphocytes that are important first-line defense immune effectors against tumors. NK cells are able to recognize and spontaneously kill damaged and stressed infected or tumor cells, without prior sensitization. NK cell activity and interaction with target cells are mediated by a balance between stimulatory and inhibitory receptors on NK cell surface and ligands on the target cells8,9. For instance, tumor cell surface presence of major histocompatibility complex molecules (MHC) class I, which interact with inhibitory killer immunoglobulin-like receptors on NK cells, induces inhibitory signals which may allow the survival of tumor cells9,10,11. NK cells have ability to control cancer progression directly via cancer cell lysis and indirectly by regulating innate and adaptive antitumor immune responses. NK cell killing of target (tumor) cells is mediated through secreted granules containing membrane-disrupting proteins perforins and proteolytic enzymes granzymes that trigger target cell lysis. NK cell killing can also be mediated by factors from the tumor necrosis factor (TNF) family9,10,11,12.
NK cell-based immunotherapy is a perspective approach in treatment of several cancers, including GBMs9,13,14. Namely, NK cells have been shown as the only immune effectors known to recognize and kill GSLCs, without approaches to generate immunogenic antigens and cell priming with appropriate costimulatory signals, as are needed for potential T cell- or dendritic cell (DC)-based immunotherapies3,11,15,16,17. This is important in GBMs since these tumors are extremely heterogeneous at the molecular and cellular levels1, expressing or lacking specific antigens in subsets of tumor cells, thereby exhibiting different genetic fingerprints in a single tumor. In addition, tumor-infiltrating immune cells, such as macrophages and Tregs, generate immunosuppressive microenvironment6, lacking antigen-presenting potential and costimulatory antigens, leading to the tumor resistance to immunotherapy.
NK cells that can select and kill cancer stem-like cells are CD16brightCD56dimCD69− population and represent 90% of peripheral blood NK cells11. In tumor microenvironment upon interactions with tumor cells and stromal cells, NK cells lose CD16 expression and increase expression of CD56 surface receptor, leading to decreased cytotoxicity and increased production of cytokines, including interferon gamma (IFN-γ). These cells are considered to be split anergized NK cells and are able to regulate the function of other cells, tumor and immune, in the tumor microenvironment11,18,19. Various cytokines, including IL-2, IL-15 and IL-12, can be used to activate and expand NK cells in vitro20. It has been shown previously that split anergy in NK cells can be achieved by the treatment of NK cells with human recombinant IL-2 and anti-CD16 monoclonal antibodies10,18,21.
In addition to cytotoxic function, NK cells act as regulatory cells and secrete various pro- and anti-inflammatory cytokines and chemokines, such as IFN-γ and interleukin (IL)−6 that orchestrate innate and adaptive immune responses and shape tumor microenvironment. For example, NK cells boost the tumor infiltration as well as maturation and activation of DCs and T cells and by that promote antitumor immune responses12,22. NK cells provide critical signals to tumor cells, which results in the differentiation of cancer stem-like cells18. IFN-γ, secreted from split anergized NK cells, was shown to be primarily responsible for NK-mediated increase in tumor cell surface expression of MHC class I, CD54, which is intercellular adhesion molecule I (ICAM1), and programmed cell death receptor ligand 1 (PD-L1), a ligand for immune checkpoint protein PD-110,18,23. Those surface markers, together with CD44, are associated with immune cell function, such as resistance or susceptibility to NK cell and T cell-mediated recognition and lysis10,18,19,23,24,34,35,36. Our immunohistochemical data also demonstrated that a certain population of NK cells, expressing CD56 in some tumors did not express CD16 receptor, implicating a possible down-regulation of CD16 by GSLCs or by other stromal elements in the niches. Lack of CD16 expression in tumor-residing NK cells is in line with previous reports on decreased CD16 expression after NK cell interactions with cancer stem-like cells34, demonstrating impairment of NK cell cytotoxicity but increasing IFN-γ secretion. This NK cell state is annotated as split anergized NK cells11,18.
NK cell delivery to GBM is considered a perspective therapeutic approach but large-scale production and activation of NK cells are still challenging9,20. Our previous work has demonstrated that osteoclasts as a feeder layer and probiotic bacteria can stimulate growth and activation of primary peripheral blood-derived NK cells to become super-activated and as such highly cytotoxic cells with high secretion of cytokines up to 1 month in cell cultures after their isolation from healthy donors. These cells are named super-charged NK cells19. One example of activating signals that are provided by osteoclasts are IL-15 and IL-12. Namely, IL-15 blocking resulted in impaired cytotoxicity and expansion of super-charged NK cells in vitro. NK cell-mediated cytotoxicity and IFN-γ secretion were decreased in super-charged NK cell cultures after IL-12 blocking19. These super-charged NK cells prevented growth and tumor-initiating potential of pancreatic and oral tumor stem-like cells as well as restored immune cell effector functions in humanized BLT mice19,23,26.
We showed that super-charged NK cells kill GSLCs in in vitro experiments in 2D co-cultures and 3D tumorospheres. In comparison to IL-2 activated primary NK cells, super-charged NK cells killed more GSLCs in both 2D and 3D in vitro models. Moreover, CD16 down-regulation in NK cells by monoclonal antibody treatments, mimicking the in vivo split anergized cells, decreased the cytotoxicity of primary and super-charged NK cells against GSLCs.
More complex 3D in vitro cellular models, including tumorosheres and organoids, that mimic tumor heterogeneity, cell-cell interactions, oxygen and nutrient deprivation and physical barriers in tumors in vivo37, are needed to test immunotherapeutic strategies, such as NK cell-based approaches. In 3D GSLC models in vitro and in human GBM tumor tissue sections, we have shown that NK cells penetrate GBM tumors and can directly interact with GSLCs. NK cells penetrate the BBB, and therefore application of NK cells to GBM patients could restore NK cell function within the tumor microenvironment.
In the present study, we demonstrated that the differential susceptibility of GSLCs to NK-mediated cytotoxicity correlates with different in vitro and in vivo properties of GSLCs. Several studies have shown great GSLC plasticity suggesting that multiple cellular states of GSLCs with different differentiation/stemness programs exist in GBM tumors. They are defined by specific phenotypic properties and biomarkers38. As described above, we selected two models of GSLCs, GS025 and NCH421k cells, with low and high susceptibility to NK cell cytotoxicity, respectively. Slowly growing GS025 cells, more sensitive to FBS differentiation, were less susceptible to NK-mediated cytotoxicity compared to highly proliferating and tumorigenic NCH421k cells with strong stemness potential3. GS025 cells also expressed higher cell surface levels of CD54 and MHC I than NCH421k cells. Increased MHC I and CD54 imply decreased susceptibility of tumor cells to NK cell-mediated lysis11. Increased MHC I expression on tumor cell surface means that tumor cells are likely to be recognized by T cells, while decreased expression or the dysfunctional MHC class I on GSLCs may be responsible for decreased T cell recognition24,25. GS025, but not NCH421k cells, expressed high levels of cell surface receptor CD44. In GBMs, CD44 is characteristically overexpressed in mesenchymal GSLC subtype, associated with higher aggressiveness, therapeutic resistance and lower survival of patients with this GBM subtype1,38. Mesenchymal GSLC aggressiveness could also be a consequence of GSLC immune evasion from NK-mediated killing as demonstrated in our experiments with GS025 cells. All GBM cells express PD-L1, known to inhibit T cell cytotoxicity. Additional experiments with fast-growing NCH421k GSLCs showed that treatment of the cells with serum and IFN-γ induced differentiation of the cells, which expressed lower levels of the transcription factor and stem-like marker OLIG2 and proliferated more slowly, and reduced their susceptibility to super-charged NK cell-mediated cytotoxicity. This phenomenon was associated with an altered balance between ligands of activating and inhibitory NK cell receptors on NCH421k cells. Moreover, the presence of NK cells and the secretion of IFN-γ in the tumor microenvironment may trigger the differentiation of GSLCs, which are less sensitive to NK cell cytotoxicity, but express high levels of MHC class I.
NK cells do not only contribute to antitumor immunity by directly eliminating tumor cells, but also by regulating the function of other immune cells, including DCs, cytotoxic lymphocytes and macrophages, through cytokine secretion30. Addition of primary NK cells to GSLCs in 2D and 3D cultures increased secretion of main pro-inflammatory cytokine IFN-γ. Split anergized primary NK cells induced higher secretion of IFN-γ after interaction with GSLCs than cytotoxic primary NK cells. Higher increase in IFN-γ secretion was detected when NK cells were cultured with NCH421k cells that had higher stemness characteristics, supporting our previous studies in other types of cancer10,11,18,23.
Elevated pro-inflammatory cytokine IL-6 has been found in GBM tumors and CSF of GBM patients21,39. Namely, IL-6 has been associated with pro-tumorigenic role in gliomas. IL-6 promotes GBM tumor progression in mice39 and activates STAT3 pathway in GSLCs to maintain tumorigenic potential40.
GBM tumors are different in that they remain persistently inflammatory even upon treatment with immune effectors, and they will increase, rather than decrease, inflammatory cytokines IL-6 and IL-8 while decreasing IFN-γ21. This is similar to what we see in CSF of GBM patient, since patient has increased IL-6 and IL-8 secretion and low IFN-γ secretion. Although IFN-γ is increased in the CSF of the GBM patient with IL-2 or IL-2 and anti-CD3/CD28 mAb treatment and this results in the decreased IL-6/IFN-γ or IL-8/IFN-γ ratio, the IFN-γ secreted from these cells is likely to increase differentiation of GSLCs. However, this will result in only further decrease in IFN-γ secretion from the interacting immune effectors while the levels of IL-6 or IL-8 will continuously rise, the scenario, which we see by the interaction of NK cells with GBM cells. Thus, during the immunotherapeutic treatment of GBM patients, the levels of IL-6 or IL-8 should be targeted to minimize their effect on the growth or expansion of GBM cells21.
Finally, studying a possible cooperation between NK cells and chemotherapeutic drugs we showed that exposure of GSLCs to NK cell supernatants increased their sensitivity to chemotherapeutic agents CDDP and TMZ. NK cell supernatants increased the cytostatic effect of CDDP in both GSLCs. However, NK cells increased TMZ cytostatic and cytotoxic effect only in fast growing and tumorigenic NCH421k tumor cells. Both chemotherapeutic drugs showed increased effect in highly tumorigenic and proliferating NCH421k after their exposure to NK supernatant, but did not show cytotoxicity in slowly proliferating GS025 GSLCs. This effect may be expected, as it is well known that DNA damaging effect of chemotherapeutics is more pronounced in faster dividing tumor cells. There is a whole spectrum of yet unknown TMZ activities that has been challenged recently41 and as seen in present study one of them is also TMZ-mediated increase of immune-related surface markers.
We observed that NK cells can change GSLC phenotype and lower their resistance to chemotherapy. However, in this case the NK supernatants did not induce GSLC differentiation into the astrocyte-like differentiated GBM cells. Instead, NK supernatant and TMZ may have induced the GSLC trans-differentiation into another GSLC state with altered immune response to T and NK cells due to their known plasticity. NK cells and TMZ did indeed increase cell surface expression of CD44, CD54 and MHC class I, important for immune cell recognition10,11,25. It is possible that NK paracrine effects decreased expression of multidrug resistance genes/proteins, such as ABC (ATP-binding cassette) transporters, decreasing general GSLC resistance to chemotherapeutics1,3,4.
In conclusions, we showed that NK cell function was impaired in peripheral blood of GBM patients in comparison to healthy donors. The presence of NK cell markers in peri-vascular GBM tissue areas indicates that NK cells crossed the leaky BBB and infiltrated the GBM tumors. Super-charged NK cells eliminated GSLCs in 2D and 3D cellular models in vitro more efficiently than the primary NK cells. Super-charged NK cell cytotoxicity was impaired after GSLC differentiation and this phenomenon was associated with altered expression levels of ligands for activating and inhibitory NK cell receptors. Besides their cytotoxicity, NK cells secreted pro-inflammatory IFN-γ and IL-6 and increased sensitivity of GSLCs to chemotherapeutic drugs, TMZ and cisplatin. Immunotherapy with allogenic super-charged NK cells appears a promising therapeutic approach in the treatment of GBM by selectively killing malignant cancer stem-like cell population, and increasing their immune-related surface markers (MHC class I and CD54) as well as their susceptibility to chemotherapy (Fig. 6k). However, known GSLC plasticity and heterogeneity is urging the research into designing a personalized approach that needs to be considered when applying NK immunotherapy in GBM treatment. To confirm our findings, in vitro and in vivo studies with higher number of patient-derived GSLCs are planned. These studies are focused on evaluating the antitumor effect of injected super-charged NK cells in GBM-bearing humanized BLT mice.
Methods
More material details are in Supplementary file.
Fluorescence immunohistochemistry
Glioblastoma biopsies were obtained from glioblastoma patients who were operated at the Department of Neurosurgery, University Medical Center of Ljubljana, Slovenia. The study was approved by the National Medical Ethics Committee of the Republic of Slovenia (Approval no. 0120-190/2018/4). Altogether, 8 patients with glioblastoma (World Health Organization [WHO] glioma grade IV) were included. Tumor diagnoses were established by standard histopathology protocols at the Institute of Pathology of the Medical Faculty, University of Ljubljana. Details of GBM patients and their tumors are described in Supplementary Table 2. Formalin-fixed, paraffin-embedded tissue sections were used for immunohistochemical analyses33,42. Tissue sections were permeabilized and non-specific binding was blocked using a solution containing 10% fetal bovine serum (v/v), 0.1% Triton X-100 (v/v) and 1% BSA (w/v) in PBS for 1 h at room temperature. After blocking, sections were incubated with TrueBlack reagent (Biotium) diluted 1:20 in 70% ethanol for 30 s to block autofluorescence due to lipofuscin and blood components. Primary goat anti-human CD56, mouse anti-human CD16, mouse anti-human SOX2, rabbit anti-human SMA and rabbit anti-human CD3 were used. Alexa Fluor 488-conjugated donkey anti-goat antibodies, Alexa Fluor 546-conjugated donkey anti-rabbit antibodies and Alexa Fluor 647-conjugated anti-mouse antibodies, were used as secondary antibodies. Nuclei were stained with Hoechst 33258 solution (94403, 1:1000, Sigma-Aldrich), for 5 min at room temperature. After washing with PBS, slides were mounted in mounting solution (P36930, Invitrogen), cover-slipped, and sealed with nail polish. Confocal imaging was performed using confocal microscope (SP8 TCS, Leica) and LAS X Life Sciences software. Details of antibodies used for fluorescence immunohistochemistry are listed in Supplementary Table 3.
Tumor cell cultures
GSLCs NCH421k were a generous gift of prof. Christel Herold-Mende (Heidelberg University, Heidelberg, Germany)3,42. GS025 GSLCs were isolated from patients with GBM at University of California Los Angeles (UCLA) under UCLA Institutional Review Board (IRB) protocol 10-00065515. GS025 and NCH421k cells were grown in serum-free conditions as described before and were validated to express GSLC markers, such as CD133 and SOX23,15,33,43. Oral squamous carcinoma stem cells (UC2) were isolated from cancer patients with tongue tumor at UCLA and cultured as described previously21,23,26. All cells were checked for Mycoplasma using MycoAlert Mycoplasma Detection Kit (Lonza, Switzerland). Authentication of cells was performed by DNA fingerprinting using Amp-FlSTR Profiler Plus PCR Amplification Kit, as described previously3,44. GS025 and NCH421k cells have a methylated MGMT promoter15,45.
Purification and treatment of primary NK cells
NK cells were purified from healthy donors with no clinical signs of disease and patients diagnosed with GBM using EasySep Human NK Enrichment kit (STEMCELL technologies, Canada) as described previously19,21,23. Freshly purified primary NK cells were then activated with IL-2 or combination of IL-2 (1000 units/mL) and anti-CD16 monoclonal antibody (mAb; 3 μg/mL) for 18–24 h to obtain primary cytotoxic and split anergized NK cells, respectively. In addition, PBMCs and NK cells were purified from three patients diagnosed with GBM. GBM patient PBMCs and NK cells were also treated with combination of IL-2 (1000 units/mL) and anti-CD3/28 mAb (25 µL/mL) or sonicated pro-biotic bacteria AJ219,23 for 18–24 h to activate T cells and induce IFN-γ secretion, respectively. The studies with immune cells from peripheral blood of healthy donors and GBM patients were approved by the UCLA Institutional Review Board (IRB#11-000781), and all participants signed written informed consent in accordance with the Declaration of Helsinki.
Generation of osteoclasts and expansion of super-charged NK cells
Generation of osteoclasts and super-charged NK cells from heathy donors was performed as described previously19,23. Briefly, purified human monocytes were differentiated to osteoclasts by treatment with M-CSF (25 ng/ml) and RANKL (25 ng/ml) for 21 days. Human purified primary NK cells were activated with IL-2 (1000 units/ml) and anti-CD16 mAb (3 μg/ml) for 18–20 h before they were cocultured with osteoclasts as feeder cells and sonicated pro-biotic bacteria AJ219,23. The culture media was refreshed with IL-2 every 3 days. The number of NK cells and contamination with T cells was monitored during super-charged NK expansion by flow cytometric analysis of CD16/56 and CD3 immunostaining. Not older than 1 month expanded super-charged NK cells were used for experiments. Details of antibodies used for flow cytometry are listed in Supplementary Table 4.
2D cocultures of NK cells and GBM cells
NK cells were left untreated or treated with IL-2 or IL-2 and anti-CD16 mAb for 18–24 h, before they were cocultured with GBM cells (single cell suspension) in different ratios for 24 h.
3D GBM model- tumorospheres
GBM cells were labelled with 30 μM of CellTracker Green for 30 min. Then GBM cell tumorospheres were established as described previously3,44 and incubated for 6 days in cell incubator (37 °C, 5% CO2). NK cells were labelled with 10 μM CellTracker Blue for 30 min before they were added to GBM cell tumorospheres in different ratios in U-bottom 96-well plate for 4–48 h. Tumorospheres were dissociated using a mixture of TrypLE Express and Collagenase type II for 30 min and cells were stained to assess cell count with Trypan blue staining, cell death using propidium iodide (PI) and flow cytometry and marker surface expression using immunolabelling and flow cytometry. Number of dead GSLCs was determined as % of CellTracker green-gated dead cells (PI-positive) and multiplied by the number of GSLCs in control spheroids.
Flow cytometry
Surface staining was performed as described previously23,46. PBMCs from patients and heathy donors were stained with antibodies against CD45, CD3, CD4. CD8, CD14, CD19, CD56/CD16 and analyzed with flow cytometry to determine % of immune cell populations within the CD45-positive cell population. Tumor cells were labelled with PE-conjugated antibodies against CD44, CD54, MHC class I, PD-L1 and B7-H6, FITC-conjugated antibodies against CD155 and ULBP1, unconjugated antibodies against ULBP3 and APC-conjugated antibodies against MICA/B, ULBP2/5/6, CD112, and HLA-E, and incubated for 30 min at 4 °C. After washing samples were analyzed by Attune flow cytometer (Invitrogen) and FlowJo software (Ashland, OR, USA). IgG isotypic controls were used as controls. PI in final concentration of 10 μg/mL was added to cell suspension to evaluate cell death. GFAP, OLIG2, and CD133 intracellular staining was performed as described previously3 and measured by flow cytometer. Primary monoclonal mouse anti-human GFAP antibody, monoclonal rabbit anti-human OLIG2 antibody, polyclonal rabbit anti-human CD133 antibody were used. Secondary PE-conjugated anti-mouse secondary antibody and Alexa Fluor 488-conjugated goat anti-rabbit antibody were used for GFAP and OLIG2/CD133 staining, respectively. Details of antibodies used for flow cytometry are listed in Supplementary Table 4.
Cytotoxicity assay - Chromium release assay
The 51Cr release assay was performed as described previously18,19,21,26. Briefly, different numbers of purified NK cells were incubated with 51Cr–labeled tumor target cells. After a 4 h incubation, the supernatants were harvested from each sample and counted for released radioactivity using the gamma counter. The percentage of specific cytotoxicity was calculated as follows (Equation 1):
LU (lytic unit) 30/106 is calculated by using the inverse of the number of effector cells needed to lyse 30% of tumor target cells × 100.
Cytotoxic ability of patient-derived primary NK cells was always tested on UC2 cells.
ELISA
ELISA kits for human IFN-γ and IL-6 (Biolegend, San Diego, CA, USA) were used according to manufacturer’s instructions.
ELISPOT
The number of IFN-γ secreting cells was analyzed using Human IFN-γ Single-Color Enzymatic ELISPOT Assay, ImmunoSpot® S6 UNIVERSAL analyzer and ImmunoSpot® SOFTWARE (all CTL Europe GmbH, Bohn, Germany), according to manufacturer’s instructions.
Multiplex cytokine assay
Multiplex arrays were used to determine the levels of secreted cytokines and chemokines. Analysis was performed using MILLIPLEX MAP Human High Sensitivity T Cell Panel (Millipore, Danvers, MA, USA) and data was analyzed using xPONENT 4.2 software (Luminex, Austin, TX, USA).
Proliferation analysis in vitro
GBM cells (5 × 104) were seeded in 12-well plate and cultured for 72, 96 and 120 h. Cells were harvested and doubling time was calculated as follows (Equation 2):
Doubling time in GBM tumorospheres was calculated based on cell numbers after dissociation by the same formula.
Confocal imaging and analysis of tumorospheres
GBM tumorosheres in U-bottom well plate were imaged from 4 h to 48 h after addition of NK cells under ×100 magnification using inverted laser scanning confocal microscope with AiryScan LSM880 and ZEN black software (both Zeiss, Germany). CellTracker blue was excited with laser line at 405 nm and emission was detected between 410 and 485 nm. CellTracker green and PI were excited with laser line at 488 nm and emission was detected between 495 and 550 nm for CellTracker green and 570–700 nm for PI. Laser power, gain and offset were kept constant between experiments and conditions. Z-stacks of confocal sections were acquired with a step size of 2.99 μm. Z-stack images of tumorospheres were analyzed and reconstructed using ZEN blue software (Zeiss, Germany) and Imaris (Bitplane) software version 9.5.1 (Oxford Instruments, United Kingdom). The number of GBM cells and dead cells was quantitated with the spot detection tool of the Imaris software. For analysis of direct cellular interactions, surface 3D renderings were created using surface area module for NK cell (CellTracker blue) and GSLC (CellTracker Green) surface using Imaris software. We then obtained surface reconstructions of NK cell surface touching GSLC surface in gray color using surface-surface contact area plug in.
Treatment of GSLCs with NK supernatants and IFN-γ
GSLCs were exposed to a total of 30 ng of human recombinant IFN-γ for 48 h and analyzed for surface marker expression. Treatment of GSLCs with NK supernatants was conducted as described previously18. Briefly, activation of NK cells was done by treatment with a combination of IL-2 (1000 U/mL) and anti-CD16 mAb (3 μg/mL) for 18 h before the supernatants were removed and used for further experiment. The amounts of IFN-γ produced by activated NK cells were assessed using ELISA kit as described above. To treat GSLCs a total of 3900 pg of IFN-γ containing supernatants were added for 5 days. After that these GSLC cells were treated with cytotoxic drugs cisplatin (CDDP, cis-diamminedichloridoplatinum(II), in final concentrations of 25 μg/mL and 50 μg/mL) and temozolomide (TMZ in final concentration of 430 μM) for 24 h and 72 h, respectively. Cell culture media and drug vehicle DMSO were used as control for CDDP and TMZ treatment, respectively. Cell number and cell death was evaluated using Trypan blue and PI staining.
Cytotoxicity assay – Calcein AM release assay
After NCH421k cells were grown in Neurobasal culture medium (Gibco, ThermoFisher Scientific) supplemented with 10% FBS for 7 days or exposed to 30 ng of human recombinant IFN-γ for 48 h, they were tested for super-charged NK cell-mediated cytotoxicity. Super-charged NK cells were activated overnight with 1000 IU IL-2/mL. Super-charged NK cells were prepared in selected effector to target ratios. NCH421k target cells were labeled with 15 µM calcein-AM stain in serum-free media for 30 min. After a washing step, 5000 target cells were added to effector cells. The plate was centrifuged at 200 g for 1 min and incubated for 3 h at 37 °C with 5% CO2. After incubation, the plate was centrifuged at 700 g for 5 min, and 50 µl supernatant was transferred to a new microtiter plate for fluorescence measurements. Released calcein-AM was measured using microplate reader Infinite M1000 Tecan (Tecan, Switzerland) at 496 nm excitation and 516 nm emission. The percentage of cytotoxicity was calculated as: 100 × (test release−spontaneous release)/(total release−spontaneous release). Spontaneous release of calcein-AM was measured in wells containing 100 μl super-charged NK culture medium and 50 μl target cells. For total release, 2% Triton X-100 was added to the super-charged NK culture media to achieve target cell lysis. Lytic units (LU) were calculated using the inverse of the number of effector cells needed to lyse 30% of the target cells multiplied by 100.
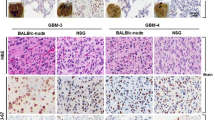
Intracranial mice injections
Animal research was performed at UCLA under the written approval of the UCLA Animal Research Committee (ARC) (protocol # 2012-101-13). Analysis of GBM cell growth was analyzed in immune-deficient NSG mice (Jackson Laboratory, USA) after intracranial injection of GS025 and NCH421k cells. Briefly, GBM cells were injected (4 × 105 cells per injection) into the right striatum of the brain in female NSG mice (3 weeks old). Injection coordinates were 2 mm lateral and 1 mm posterior to the bregma, at a depth of 2 mm15. Mice were sacrificed when clinical signs of brain tumor developed.
Tumor burden measurements in mice and isolation of tumor cells from mice tumors
Tumor burden was monitored on the basis of secreted Gaussia luciferase measurements in mice blood. GBM cells were infected with a lentiviral vector containing a secreted Gaussia luciferase (sGluc)-encoding reporter gene (Targeting Systems no. GL-GFP) and intracranially implanted into the right striatum in mice. Measurements of sGluc levels were performed as described previously15. GBM mice tumors were minced, washed with 1× PBS, incubated with trypsin for 10 min and passed through 70 μm strainer. Isolated single human GSLC (GS025, NCH412k) suspensions were incubated in serum-free conditions and imaged for several days.
Statistics and reproducibility
All experiments were set up in duplicates or triplicates and tested in at least three independent experiments (n ≥ 3) unless stated otherwise. An unpaired, two-tailed Student’s t test or one-way ANOVA test with Bonferroni correction was used to perform statistical analyses in GraphPad Prism software version 8 (La Jolla, CA, USA). P values < 0.05 were considered to indicate significant differences. The p values were expressed within the Figures as follows: ***p value < 0.001, **p value: 0.001–0.01, *p value: 0.01–0.05.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data generated or analyzed during this study are included in this published paper and its Supplementary File and Supplementary Data File 1. The datasets generated during and/or analyzed during the current study are also available from the corresponding author on reasonable request.
References
Lah, T. T., Novak, M. & Breznik, B. Brain malignancies: Glioblastoma and brain metastases. Semin. Cancer Biol. 60, 262–273 (2020).
Louis, D. N. et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 131, 803–820 (2016).
Podergajs, N. et al. Transmembrane protein CD9 is glioblastoma biomarker, relevant for maintenance of glioblastoma stem cells. Oncotarget 7, 593–609 (2016).
Gimple, R. C., Bhargava, S., Dixit, D. & Rich, J. N. Glioblastoma stem cells: lessons from the tumor hierarchy in a lethal cancer. Genes Dev. 33, 591–609 (2019).
Bao, S. et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature 444, 756–760 (2006).
Perus, L. J. M. & Walsh, L. A. Microenvironmental Heterogeneity in Brain Malignancies. Front. Immunol. 10, 2294 (2019).
Kwok, D. & Okada, H. T-Cell based therapies for overcoming neuroanatomical and immunosuppressive challenges within the glioma microenvironment. J. Neurooncol. 147, 281–295 (2020).
Lo, H. C. et al. Resistance to natural killer cell immunosurveillance confers a selective advantage to polyclonal metastasis. Nat. Cancer 1, 709–722 (2020).
Golán, I., De La Fuente, L. R. & Costoya, J. A. NK cell-based glioblastoma immunotherapy. Cancers (Basel) 10, 1–16 (2018).
Tseng, H. C. et al. Differential targeting of stem cells and differentiated glioblastomas by NK cells. J. Cancer 6, 866–876 (2015).
Jewett, A. et al. Natural Killer Cells: Diverse Functions in Tumor Immunity and Defects in Pre-neoplastic and Neoplastic Stages of Tumorigenesis. Mol. Ther. - Oncolytics 16, 41–52 (2020).
Vivier, E., Tomasello, E., Baratin, M., Walzer, T. & Ugolini, S. Functions of natural killer cells. Nat. Immunol. 9, 503–510 (2008).
Zhang, C. et al. ErbB2/HER2-Specific NK Cells for Targeted Therapy of Glioblastoma. J. Natl Cancer Inst. 108, 1–12 (2016).
Han, J. et al. CAR-engineered NK cells targeting wild-type EGFR and EGFRvIII enhance killing of glioblastoma and patient-derived glioblastoma stem cells. Sci. Rep. 5, 1–13 (2015).
Mai, W. X. et al. Cytoplasmic p53 couples oncogene-driven glucose metabolism to apoptosis and is a therapeutic target in glioblastoma. Nat. Med. 23, 1342–1351 (2017).
Hasan, T. et al. Interleukin-8/CXCR2 signaling regulates therapy-induced plasticity and enhances tumorigenicity in glioblastoma. Cell Death Dis. 10, 292 (2019).
Avril, T. et al. Human glioblastoma stem-like cells are more sensitive to allogeneic NK and T cell-mediated killing compared with serum-cultured glioblastoma cells. Brain Pathol. 22, 159–174 (2012).
Tseng, H. C., Bui, V., Man, Y. G., Cacalano, N. & Jewett, A. Induction of split anergy conditions natural killer cells to promote differentiation of stem cells through cell-cell contact and secreted factors. Front. Immunol. 5, 1–24 (2014).
Kaur, K. et al. Novel strategy to expand super-charged NK cells with significant potential to lyse and differentiate cancer stem cells: differences in NK expansion and function between healthy and cancer patients. Front. Immunol. 8, 297 (2017).
Guillerey, C., Huntington, N. D. & Smyth, M. J. Targeting natural killer cells in cancer immunotherapy. Nat. Immunol. 17, 1025–1036 (2016).
Kozlowska, A. K. et al. Resistance to cytotoxicity and sustained release of interleukin-6 and interleukin-8 in the presence of decreased interferon-γ after differentiation of glioblastoma by human natural killer cells. Cancer Immunol. Immunother. 65, 1085–1097 (2016).
Barry, K. C. et al. A natural killer-dendritic cell axis defines checkpoint therapy-responsive tumor microenvironments. Nat. Med. 24, 1178–1191 (2018).
Kaur, K. et al. Probiotic-treated super-charged NK cells efficiently clear poorly differentiated pancreatic tumors in Hu-BLT mice. Cancers (Basel). 12, 63 (2020).
Vitale, M., Cantoni, C., Pietra, G., Mingari, M. C. & Moretta, L. Effect of tumor cells and tumor microenvironment on NK-cell function. Eur. J. Immunol. 44, 1582–1592 (2014).
Yang, W., Li, Y., Gao, R., **u, Z. & Sun, T. MHC class I dysfunction of glioma stem cells escapes from CTL-mediated immune response via activation of Wnt/β-catenin signaling pathway. Oncogene 39, 1098–1111 (2020).
Kaur, K. et al. Super-charged NK cells inhibit growth and progression of stem-like/poorly differentiated oral tumors in vivo in humanized BLT mice; effect on tumor differentiation and response to chemotherapeutic drugs. Oncoimmunology 7, e1426518 (2018).
Myers, J. A. & Miller, J. S. Exploring the NK cell platform for cancer immunotherapy. Nat. Rev. Clin. Oncol. 18, 85–100 (2021).
Stupp, R. et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 10, 459–466 (2009).
Haspels, H. N., Rahman, M. A., Joseph, J. V., Navarro, A. G. & Chekenya, M. Glioblastoma stem-like cells are more susceptible than differentiated cells to natural killer cell lysis mediated through killer immunoglobulin-like receptors-human leukocyte antigen ligand mismatch and activation receptor-ligand interactions. Front. Immunol. 9, 1–17 (2018).
Burger, M. C. et al. CAR-Engineered NK Cells for the Treatment of Glioblastoma: Turning Innate Effectors Into Precision Tools for Cancer Immunotherapy. Front. Immunol. 10, 1–16 (2019).
Hira, V. V. V. et al. Cathepsin K cleavage of SDF-1α inhibits its chemotactic activity towards glioblastoma stem-like cells. Biochim. Biophys. Acta - Mol. Cell Res. 1864, 594–603 (2017).
Aderetti, D. A., Hira, V. V. V., Molenaar, R. J. & van Noorden, C. J. F. The hypoxic peri-arteriolar glioma stem cell niche, an integrated concept of five types of niches in human glioblastoma. Biochim. Biophys. Acta - Rev. Cancer 1869, 346–354 (2018).
Hira, V. V. V. et al. Similarities Between Stem Cell Niches in Glioblastoma and Bone Marrow: Rays of Hope for Novel Treatment Strategies. J. Histochem. Cytochem. 68, 33–57 (2019).
Friebel, E. et al. Single-Cell Map** of Human Brain Cancer Reveals Tumor-Specific Instruction of Tissue-Invading Leukocytes. Cell 181, 1626–1642.e20 (2020).
Kmiecik, J. et al. Elevated CD3+ and CD8+ tumor-infiltrating immune cells correlate with prolonged survival in glioblastoma patients despite integrated immunosuppressive mechanisms in the tumor microenvironment and at the systemic level. J. Neuroimmunol. 264, 71–83 (2013).
Sharifzad, F. et al. HSP70/IL-2 treated NK cells effectively cross the blood brain barrier and target tumor cells in a rat model of induced glioblastoma multiforme (GBM). Int. J. Mol. Sci. 21, 2263 (2020).
Jacob, F. et al. A Patient-Derived Glioblastoma Organoid Model and Biobank Recapitulates Inter- and Intra-tumoral Heterogeneity. Cell 180, 188–204.e22 (2020).
Suvà, M. L. & Tirosh, I. The Glioma Stem Cell Model in the Era of Single-Cell Genomics. Cancer Cell 37, 630–636 (2020).
Wang, Q. et al. Vascular niche IL-6 induces alternative macrophage activation in glioblastoma through HIF-2α. Nat. Commun. 9, 559 (2018).
Shi, Y. et al. Tetraspanin CD9 stabilizes gp130 by preventing its ubiquitin-dependent lysosomal degradation to promote STAT3 activation in glioma stem cells. Cell Death Differ. 24, 167–180 (2017).
Herbener, V. J. et al. Considering the Experimental Use of Temozolomide in Glioblastoma Research. Biomedicines 8, 151 (2020).
Novak, M. et al. CCR5-Mediated Signaling Is Involved in Invasion of Glioblastoma Cells in Its Microenvironment. Int. J. Mol. Sci. 21, 4199 (2020).
Nathanson, D. A. et al. Targeted therapy resistance mediated by dynamic regulation of extrachromosomal mutant EGFR DNA. Sci. (80-.) 343, 72–76 (2014).
Breznik, B., Motaln, H., Vittori, M., Rotter, A. & Turnšek, T. L. Mesenchymal stem cells differentially affect the invasion of distinct glioblastoma cell lines. Oncotarget 8, 25482–25499 (2017).
Dirkse, A. et al. Stem cell-associated heterogeneity in Glioblastoma results from intrinsic tumor plasticity shaped by the microenvironment. Nat. Commun. 10, 1787 (2019).
Kaur, K., Ko, M. W., Ohanian, N., Cook, J. & Jewett, A. Osteoclast-expanded super-charged NK-cells preferentially select and expand CD8+ T cells. Sci. Rep. 10, 20363 (2020).
Acknowledgements
We acknowledge the contribution and support of prof. Tamara Lah Turnšek from National institute of biology Ljubljana. We thank Andrej Porčnik, MD, from University Medical Centre Ljubljana for clinical data of glioblastoma patients. This work was supported by Slovenian Research Agency (Grant programs P1-0245 and P1-0207, Grant project J3-8201, Postdoctoral project Z3-1870, Young researcher grant and Bilateral project BI-US/19-21-021) and by the European Program of Cross-Border Cooperation for Slovenia-Italy Interreg TRANS-GLIOMA. We thank our funding agencies (NIH and NIDCR) and all the donors for supporting the work.
Author information
Authors and Affiliations
Contributions
B.B. designed and performed experiments, analyzed and interpreted data and wrote the paper. M.W.K. designed and performed experiments and analyzed data. C.T., P.C.C., E.S., B.M., A.H., N.A. performed experiments and analyzed data. M.N., V.Ž., J.M. provided samples and analyzed the data. D.N. analyzed and interpreted data. A.J. conceived the project, designed the experiments, analyzed and interpreted the data and wrote the paper. All authors reviewed and approved the submitted version of paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks Serena Pellegatta and the other, anonymous, reviewer for their contribution to the peer review of this work. Primary Handling Editors: Toshiro Moroishi and Eve Rogers. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Breznik, B., Ko, MW., Tse, C. et al. Infiltrating natural killer cells bind, lyse and increase chemotherapy efficacy in glioblastoma stem-like tumorospheres. Commun Biol 5, 436 (2022). https://doi.org/10.1038/s42003-022-03402-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-022-03402-z
- Springer Nature Limited
This article is cited by
-
From glioma gloom to immune bloom: unveiling novel immunotherapeutic paradigms-a review
Journal of Experimental & Clinical Cancer Research (2024)
-
Dysfunctional natural killer cells can be reprogrammed to regain anti-tumor activity
The EMBO Journal (2024)