Abstract
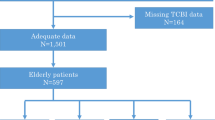
To determine the most appropriate nutritional assessment tool for predicting the occurrence of major adverse cardiovascular events (MACE) within 1 year in elderly ACS patients undergoing PCI from four nutritional assessment tools including PNI, GNRI, CONUT, and BMI. Consecutive cases diagnosed with acute coronary syndrome (ACS) and underwent percutaneous coronary intervention (PCI) in the Department of Cardiovascular Medicine of the Air force characteristic medical center from 1 January 2020 to 1 April 2022 were retrospectively collected. The basic clinical characteristics and relevant test and examination indexes were collected uniformly, and the cases were divided into the MACE group (174 cases) and the non-MACE group (372 cases) according to whether a major adverse cardiovascular event (MACE) had occurred within 1 year. Predictive models were constructed to assess the nutritional status of patients with the Prognostic Nutritional Index (PNI), Geriatric Nutritional Risk Index (GNRI), Controlling nutritional status (CONUT) scores, and Body Mass Index (BMI), respectively, and to analyze their relationship with prognosis. The incremental value of the four nutritional assessment tools in predicting risk was compared using the Integrated Discriminant Improvement (IDI) and the net reclassification improvement (NRI). The predictive effect of each model on the occurrence of major adverse cardiovascular events (MACE) within 1 year in elderly ACS patients undergoing PCI was assessed using area under the ROC curve (AUC), calibration curves, decision analysis curves, and clinical impact curves; comparative analyses were performed. Among the four nutritional assessment tools, the area under the curve (AUC) was significantly higher for the PNI (AUC: 0.798, 95%CI 0.755–0.840 P < 0.001) and GNRI (AUC: 0.760, 95%CI 0.715–0.804 P < 0.001) than for the CONUT (AUC: 0.719,95%CI 0.673–0.765 P < 0.001) and BMI (AUC: 0.576, 95%CI 0.522–0.630 P < 0.001). The positive predictive value (PPV) of PNI: 67.67% was better than GNRI, CONUT, and BMI, and the negative predictive value (NPV): of 83.90% was better than CONUT and BMI and similar to the NPV of GNRI. The PNI, GNRI, and CONUT were compared with BMI, respectively. The PNI had the most significant improvement in the Integrated Discriminant Improvement Index (IDI) (IDI: 0.1732, P < 0.001); the PNI also had the most significant improvement in the Net Reclassification Index (NRI) (NRI: 0.8185, P < 0.001). In addition, of the four nutritional assessment tools used in this study, the PNI was more appropriate for predicting the occurrence of major adverse cardiovascular events (MACE) within 1 year in elderly ACS patients undergoing PCI.
Similar content being viewed by others
Introduction
As the global population continues to age, the over-65s and over-80s will be the fastest-growing segments of the population1. As a result, the elderly population will continue to grow and there will be a further increase in the number of elderly patients with acute coronary syndromes. Acute coronary syndrome (ACS) is an acute ischemic syndrome caused by rupture of unstable atherosclerotic plaques or fresh thrombosis secondary to erosion in the coronary artery2. ACS is an important cause of disability and death in patients3. With the rapid development of percutaneous coronary intervention (PCI), PCI has become the mainstay of treatment for patients with ACS4,5.Despite medical advances such as PCI, ACS still has high mortality, and MACE rates6,7. Along with the increasing number of elderly ACS patients treated with PCI, the regression after PCI has also become a widespread concern. Recent evidence suggests that malnutrition is an important factor in the prognosis of cardiovascular (CV) disease8. However, the nutritional status of patients is often overlooked, despite its association with poor outcomes in patients with cardiovascular disease9,10. Nutritional status affects patient regression after surgery, so early identification of patient nutritional status facilitates clinicians to make early clinical decisions and interventions to optimize clinical management to improve patient prognosis37. One type of modeling is prognostic modeling, which centers on assessing the likelihood of potential outcomes such as disease recurrence, mortality, incapacity, or complications manifesting at some point in the future based on the patient's current state of health38. Clinical prediction models can evaluate and classify the risk of patients based on fundamental clinical features and tests and examinations, thus aiding the identification of medium- and high-risk individuals early on. This can help clinicians create sensible management strategies and measures for controlling risk factors for patients outside of the hospital setting. In addition, the study of interaction prediction in various fields of computational biology provides valuable research directions. The study by Sun et al.39 provided a new deep learning algorithm called Graph Convolutional Networks with Graph Attention Networks (GCNAT), which promises to be a useful biomedical research tool for predicting potential metabolite disease associations in the future. It may be more convenient to analyse the nutritional status of ACS patients and allow us to better predict the risk of MACE in elderly ACS patients. Wang et al.40 developed a novel deep learning prediction model called DMFGAM that could become a powerful tool for predicting hERG channel blockers in the early stages of drug discovery and development. Predictive modelling will be widely used in the future to help clinicians make better diagnoses and treatments.
We constructed a column-line diagram of the clinical prediction model for the occurrence of MACE within 1 year after PCI in elderly ACS patients with each of the four dietary assessment tools. The risk of develo** MACE can be suggested more intuitively. According to the calibration curves, the three prediction models constructed from PNI, GNRI, and CONUT had good calibration ability; the decision analysis curves (DCA) suggested that the models constructed from PNI and GNRI had high clinical validity, while the prediction model constructed from BMI had poor clinical validity. The Clinical Impact Curve (CIC) suggests that the PNI and GNRI constructs have a lower rate of misdiagnosis than the CONUT and BMI constructs. The PNI can better predict the risk of develo** MACE, as reflected more intuitively by the predictive model we constructed.
There are many screening tools for malnutrition, but there is no consensus on which screening tool to use in patients with ACS. Based on our results, we suggest using the PNI score, which uses only 2 laboratory values and is very easy to calculate even without a specific automated calculator. Screening for malnutrition in elderly ACS patients undergoing PCI may identify patients at high risk of adverse cardiovascular outcomes who may benefit from targeted secondary prevention programs with supplementation to improve their prognosis.
Limitations of the study
The present study is a single-centre retrospective study with a relatively small number of patients and therefore has some drawbacks. There is no information in this study about patients' economic status, education, adherence, etc., which might help us to understand the causal factors of malnutrition. We did not compare the prognostic value of a nutritional screening tool with a more sophisticated comprehensive nutritional assessment. This is because malnutrition is a complex problem, especially in the elderly, with diverse etiologies and a wide range of determinants. The validity of assessing nutritional status through simple screening tools (PNI, GNRI, CONUT, and BMI) alone remains uncertain because of the lack of comparison with comprehensive nutritional assessments, such as subjective holistic assessments and mini-nutritional assessments. We only assessed nutritional status on admission and did not examine the relationship between changes in nutritional status over time and the incidence of MACE after PCI in elderly ACS patients. The results still need further validation with large samples and multicenter data. We welcome additions and improvements to this study from other researchers and medical centres in different countries.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACS:
-
Acute coronary syndromes
- PCI:
-
Percutaneous coronary intervention
- MACE:
-
Major adverse cardiovascular event
- PNI:
-
Prognostic Nutritional Index
- GNRI:
-
Geriatric Nutritional Risk Index
- CONUT:
-
Controlling nutritional status
- BMI:
-
Body Mass Index
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- IDI:
-
Integrated discrimination improvement
- NRI:
-
Net reclassification improvement
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- OR:
-
Odds ratios
- CI:
-
Confidence intervals
- SE:
-
Standard error
- GRACE:
-
Global registry of acute coronary events
References
Giacomello, E. & Toniolo, L. Nutrition, diet and healthy aging. Nutrients 14(1), 190. https://doi.org/10.3390/nu14010190 (2021).
Bergmark, B. A. et al. Acute coronary syndromes. Lancet 399(10332), 1347–1358. https://doi.org/10.1016/s0140-6736(21)02391-6 (2022).
Roth, G. A. et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 70(1), 1–25. https://doi.org/10.1016/j.jacc.2017.04.052 (2017).
Damluji, A. A. et al. Management of acute coronary syndrome in the older adult population: A scientific statement from the american heart association. Circulation. 147(3), e32–e62. https://doi.org/10.1161/cir.0000000000001112 (2023).
Zeymer, U. et al. Influence of culprit lesion intervention on outcomes in infarct-related cardiogenic shock with cardiac arrest. J. Am. Coll. Cardiol. 81(12), 1165–1176. https://doi.org/10.1016/j.jacc.2023.01.029 (2023).
Szummer, K., Jernberg, T. & Wallentin, L. From early pharmacology to recent pharmacology interventions in acute coronary syndromes: Jacc state-of-the-art review. J. Am. Coll. Cardiol. 74(12), 1618–1636. https://doi.org/10.1016/j.jacc.2019.03.531 (2019).
Bueno, H. et al. In-hospital coronary revascularization rates and post-discharge mortality risk in non-st-segment elevation acute coronary syndrome. J. Am. Coll. Cardiol. 74(11), 1454–1461. https://doi.org/10.1016/j.jacc.2019.06.068 (2019).
Popiolek-Kalisz, J. & Szczygiel, K. Bioelectrical impedance analysis and body composition in cardiovascular diseases. Curr. Probl. Cardiol. 48(11), 101911. https://doi.org/10.1016/j.cpcardiol.2023.101911 (2023).
Casas-Vara, A. et al. The obesity paradox in elderly patients with heart failure: Analysis of nutritional status. Nutrition. 28(6), 616–622. https://doi.org/10.1016/j.nut.2011.10.006 (2012).
Kunimura, A. et al. Impact of geriatric nutritional risk index on cardiovascular outcomes in patients with stable coronary artery disease. J. Cardiol. 69(1), 383–388. https://doi.org/10.1016/j.jjcc.2016.09.004 (2017).
**ao, Q. et al. Clinical significance of controlling nutritional status score (CONUT) in evaluating outcome of postoperative patients with gastric cancer. Sci. Rep. 12(1), 93. https://doi.org/10.1038/s41598-021-04128-4 (2022).
Huang, Y. et al. The prognostic nutritional index predicts all-cause mortality in critically ill patients with acute myocardial infarction. BMC Cardiovasc. Disord. 23(1), 339. https://doi.org/10.1186/s12872-023-03350-4 (2023).
Jiang, Z. et al. Prevalence and associated factors of malnutrition in patients with Parkinson’s disease using conut and gnri. Parkinsonism Relat. Disord. 95, 115–121. https://doi.org/10.1016/j.parkreldis.2021.11.032 (2022).
Onodera, T., Goseki, N. & Kosaki, G. prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 85(9), 1001–1005 (1984).
Chen, Q. J. et al. Prognostic nutritional index predicts clinical outcome in patients with acute st-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Sci. Rep. 7(1), 3285. https://doi.org/10.1038/s41598-017-03364-x (2017).
Kurtul, A. et al. Usefulness of serum albumin concentration to predict high coronary syntax score and in-hospital mortality in patients with acute coronary syndrome. Angiology. 67(1), 34–40. https://doi.org/10.1177/0003319715575220 (2016).
Suzuki, S. et al. Prognostic significance of serum albumin in patients with stable coronary artery disease treated by percutaneous coronary intervention. PLoS ONE. 14(7), e0219044. https://doi.org/10.1371/journal.pone.0219044 (2019).
Abd Aziz, N. A. S., Teng, N., Abdul Hamid, M. R. & Ismail, N. H. Assessing the nutritional status of hospitalized elderly. Clin. Interv. Aging. 12, 1615–1625. https://doi.org/10.2147/cia.S140859 (2017).
Nuttall, F. Q. Body mass index: Obesity, BMI, and health: A critical review. Nutr. Today. 50(3), 117–128. https://doi.org/10.1097/nt.0000000000000092 (2015).
Bucholz, E. M., Krumholz, H. A. & Krumholz, H. M. Underweight, markers of cachexia, and mortality in acute myocardial infarction: A prospective cohort study of elderly medicare beneficiaries. PLoS Med. 13(4), e1001998. https://doi.org/10.1371/journal.pmed.1001998 (2016).
Ignacio De Ulíbarri, J. et al. CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr. Hosp. 20(1), 38–45 (2005).
Ng, W. L., Collins, P. F., Hickling, D. F. & Bell, J. J. Evaluating the concurrent validity of body mass index (BMI) in the identification of malnutrition in older hospital inpatients. Clin. Nutr. 38(5), 2417–2422. https://doi.org/10.1016/j.clnu.2018.10.025 (2019).
Hayama, T. et al. The preoperative geriatric nutritional risk index (GNRI) is an independent prognostic factor in elderly patients underwent curative resection for colorectal cancer. Sci. Rep. 12(1), 3682. https://doi.org/10.1038/s41598-022-07540-6 (2022).
Cao, L. Y., Cheng, S., Lin, L. & Chen, M. X. Effect of controlling nutritional status score (CONUT) and prognostic nutritional index (PNI) on patients after spinal tuberculosis surgery. Sci. Rep. 12(1), 16056. https://doi.org/10.1038/s41598-022-19345-8 (2022).
Wada, H. et al. Prognostic impact of nutritional status assessed by the controlling nutritional status score in patients with stable coronary artery disease undergoing percutaneous coronary intervention. Clin. Res. Cardiol. 106(11), 875–883. https://doi.org/10.1007/s00392-017-1132-z (2017).
Goldfarb, M. et al. Malnutrition and mortality in frail and non-frail older adults undergoing aortic valve replacement. Circulation. 138(20), 2202–2211. https://doi.org/10.1161/circulationaha.118.033887 (2018).
Yuan, K. et al. Association between malnutrition and long-term mortality in older adults with ischemic stroke. Clin. Nutr. 40(5), 2535–2542. https://doi.org/10.1016/j.clnu.2021.04.018 (2021).
Tonet, E. et al. Nutritional status and all-cause mortality in older adults with acute coronary syndrome. Clin. Nutr. 39(5), 1572–1579. https://doi.org/10.1016/j.clnu.2019.06.025 (2020).
Kalantar-Zadeh, K., Anker, S. D., Horwich, T. B. & Fonarow, G. C. Nutritional and anti-inflammatory interventions in chronic heart failure. Am. J. Cardiol. 101(11a), 89e–103e. https://doi.org/10.1016/j.amjcard.2008.03.007 (2008).
Merker, M. et al. Association of baseline inflammation with effectiveness of nutritional support among patients with disease-related malnutrition: A secondary analysis of a randomized clinical trial. JAMA Netw. Open. 3(3), e200663. https://doi.org/10.1001/jamanetworkopen.2020.0663 (2020).
Sueta, D. et al. Validation of the high mortality rate of malnutrition-inflammation-atherosclerosis syndrome: Community-based observational study. Int. J. Cardiol. 230, 97–102. https://doi.org/10.1016/j.ijcard.2016.12.072 (2017).
Li, X. et al. Caspase-1 and gasdermin d afford the optimal targets with distinct switching strategies in nlrp1b inflammasome-induced cell death. Research 2022, 9838341. https://doi.org/10.34133/2022/9838341 (2022).
Li, X. et al. Rip1-dependent linear and nonlinear recruitments of caspase-8 and rip3 respectively to necrosome specify distinct cell death outcomes. Protein Cell. 12(11), 858–876. https://doi.org/10.1007/s13238-020-00810-x (2021).
Xu, F. et al. Specificity and competition of mrnas dominate droplet pattern in protein phase separation. Phys. Rev. Res. 5(2), 023159. https://doi.org/10.1103/PhysRevResearch.5.023159 (2023).
Yoshihisa, A. et al. Impact of nutritional indices on mortality in patients with heart failure. Open Heart. 5(1), e000730. https://doi.org/10.1136/openhrt-2017-000730 (2018).
Loreggian, L. et al. Baseline conditions and nutritional state upon hospitalization are the greatest risks for mortality for cardiovascular diseases and for several classes of diseases: A retrospective study. Sci. Rep. 12(1), 10819. https://doi.org/10.1038/s41598-022-14643-7 (2022).
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (tripod): The tripod statement. BMJ. 350, g7594. https://doi.org/10.1136/bmj.g7594 (2015).
Hoesseini, A. et al. Key aspects of prognostic model development and interpretation from a clinical perspective. JAMA Otolaryngol. Head Neck Surg. 148(2), 180–186. https://doi.org/10.1001/jamaoto.2021.3505 (2022).
Sun, F., Sun, J. & Zhao, Q. A deep learning method for predicting metabolite-disease associations via graph neural network. Brief Bioinform. https://doi.org/10.1093/bib/bbac266 (2022).
Wang, T., Sun, J. & Zhao, Q. Investigating cardiotoxicity related with herg channel blockers using molecular fingerprints and graph attention mechanism. Comput. Biol. Med. 153, 106464. https://doi.org/10.1016/j.compbiomed.2022.106464 (2023).
Acknowledgements
This study was supported by the Scientific Research Project of Air Force Comprehensive Research on Equipment (KJ2022A000409); the Science and Technology Boosting Programme of Air force characteristic medical center (2022ZTYB14); and the Natural Science Foundation of Bei**g Municipality (7232174).
Author information
Authors and Affiliations
Contributions
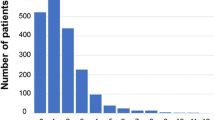
X.-Y.Z. and D.-D.Y. wrote the main manuscript text and K.-J.Z. and H.-J.Z. prepared Figs. 1, 2, 3, 4, 5. F.-F.S. collected the data needed for this study. J.-W.T. and X.-Y.Z. completed the conception and design of this study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, XY., Yang, DD., Zhang, KJ. et al. Comparative analysis of four nutritional scores predicting the incidence of MACE in older adults with acute coronary syndromes after PCI. Sci Rep 13, 20333 (2023). https://doi.org/10.1038/s41598-023-47793-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47793-3
- Springer Nature Limited