Abstract
Radiomics is a method to mine large numbers of quantitative imaging features and develop predictive models. It has shown exciting promise for improved cancer decision support from early detection to personalized precision treatment, and therefore offers a desirable new direction for pancreatic cancer where the mortality remains high despite the current care and intense research. For radiomics, interobserver segmentation variability and its effect on radiomic feature stability is a crucial consideration. While investigations have been reported for high-contrast cancer sites such as lung cancer, no studies to date have investigated it on CT-based radiomics for pancreatic cancer. With three radiation oncology observers and three radiology observers independently contouring on the contrast CT of 21 pancreatic cancer patients, we conducted the first interobserver segmentation variability study on CT-based radiomics for pancreatic cancer. Moreover, our novel investigation assessed whether there exists an interdisciplinary difference between the two disciplines. For each patient, a consensus tumor volume was generated using the simultaneous truth and performance level expectation algorithm, using the dice similarity coefficient (DSC) to assess each observer’s delineation against the consensus volume. Radiation oncology observers showed a higher average DSC of 0.81 ± 0.06 than the radiology observers at 0.69 ± 0.16 (p = 0.002). On a panel of 1277 radiomic features, the intraclass correlation coefficients (ICC) was calculated for all observers and those of each discipline. Large variations of ICCs were observed for different radiomic features, but ICCs were generally higher for the radiation oncology group than for the radiology group. Applying a threshold of ICC > 0.75 for considering a feature as stable, 448 features (35%) were found stable for the radiation oncology group and 214 features (16%) were stable from the radiology group. Among them, 205 features were found stable for both groups. Our results provide information for interobserver segmentation variability and its effect on CT-based radiomics for pancreatic cancer. An interesting interdisciplinary variability found in this study also introduces new considerations for the deployment of radiomics models.
Similar content being viewed by others
Introduction
Pancreatic cancer is a critical global health care problem. Its low detectability rate and late-stage onset of symptoms contribute to a poor prognosis with a 5-year overall survival rate at 9% for patients diagnosed from 2008 to 20141. Despite decades of research, pancreatic cancer remains an extremely lethal cancer with the highest mortality rate of all major cancers in the US2. Radiomics, a new big-data based “omics” branch, has introduced a new direction to facilitate early cancer detection and personalized precision treatment. While it holds potentials to be especially helpful for pancreatic cancer where other research alone yielded limited success, the low contrast and poor conspicuity of pancreatic tumor poses a special challenge. Although there have been developments in abdominal CT imaging, such as dual- and tri-phase contrast imaging and energy spectrum CTs, which have improved the accuracy in defining local tumor extension for pancreatic cancer, tumor segmentation is still particularly challenging3.
Radiomics has demonstrated the potential to serve as a tool for the detection, characterization, diagnosis, and prognosis for many cancers4,5,6,7. With the advancement of machine learning capabilities along with growing interest in personalized medicine, radiomics analysis has become an exciting and current area of research. Radiomics could desirably be applied to pancreatic cancer to aid in early detection and help improve treatment efficacy. The typical radiomic workflow begins with the acquisition of medical images, from which a volume of interest, which is often the tumor, can be segmented for feature extraction. These radiomic features are the input data for statistical or machine learning algorithms to select, integrate, and build predictive models. A critical branch of radiomics research relates to the reproducibility of radiomics analysis8. These include challenging issues such as the lack of standardized feature extraction parameters, motion induced effects, volume delineation variation, image acquisition/reconstruction variability, and other factors that lead to non-inherent variability9,10,11. Uncertainties in segmentation are particularly critical since it is one of the upstream steps in the radiomics workflow, therefore affecting all downstream processes. Among these uncertainties relating to segmentation are interobserver variability which has been relatively well-researched for other cancer types such as lung cancer, and interdisciplinary variability, which we wish to introduce in this work.
The effect of interobserver variability on radiomic feature stability and reproducibility has been studied in cancer sites such as lung, breast, glioblastoma, and liver12,13,14,15,16,17,18,19,20,21,22. One can expect that the interobserver variability is organ dependent and hence plays a role of varying dominance in the radiomics reproducibility, and therefore needs to be separately characterized for low contrast regions such as the pancreas23,24,25,26 than high contrast regions such as the lung. In this work, we investigated the segmentation and resulting radiomic feature variations due to the interobserver variability. Contrast enhanced CT images were used for the study as it remains the standard and most used imaging modality for visualizing the pancreas26.
In this study, our expert observers included both radiation oncologists and radiologists. These two disciplines also represent the dominating disciplines from which the vast majority of radiomic investigations were conducted27,28,29,30,31. Exploring whether an interdisciplinary segmentation variability exists for radiomic research would also be interesting and illuminating. Interdisciplinary variation on segmentation is a new concept and an area of limited study. A recent publication from Nq et al. shows there is significant specialty-dependent variation in contouring post-operative tumor cavities for targeting adjuvant oral cancer therapy32. To date, no study has explored the effects of interdisciplinary segmentation variability in the context of radiomics. Thus, in this study we aim to investigate the robustness of radiomic features due to both interobserver and interdisciplinary segmentation variability using contrast-enhanced CT for pancreatic cancer. The study aims both to contribute to the discussion of reproducibility related challenges in the radiomics approach, and to pave ways for radiomics-based applications in pancreatic cancer decision making.
Results
Segmentation variability
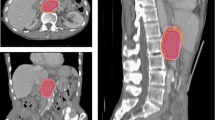
Interobserver and interdisciplinary segmentation variability were observed. Figure 1 illustrates two example cases delineated by all observers with varying degrees of agreement between observers. For the case on the left, a high volume agreement was observed among observers. For the patient on the right, a low agreement was observed. Anecdotally, on this patient, the three radiation oncology observers delineated significantly larger volumes than the three radiology observers. For the patient cohort overall, the radiology observers were also found to contour more conservatively than the radiation oncology observers, yielding a mean volume of. 35.6 ± 15.0 cm3 versus 54.1 ± 15.9 cm3 (p < 0.0001).
The dice similarity coefficient (DSC) was calculated per patient to quantify the agreement between each observer contour with the consensus contour. Figure 2 shows the distribution of DSC values with mean and standard deviations within each discipline for each patient CT image. The mean DSC for radiation oncology observers and radiology observers were 0.81 ± 0.06 and 0.69 ± 0.16, respectively. Using the grading scale defined in the color legend of Fig. 2, 6 cases of high agreement (DSC > 0.85) were observed for radiation oncology, with no average DSC values falling below medium agreement (DSC < 0.7), compared to the 4 cases of very low agreement from radiology contours (DSC < 0.5). As shown in the distribution plot in Fig. 2, the radiation oncology group showed both a higher average agreement with the consensus segmentation (indicated by higher average DSCs) and a higher agreement with each other (indicated by the tighter standard deviations), when compared with the radiology group. A paired two-tailed independent T-test calculated a p-value of 0.0038 indicating a statistical significance of the different DSC values between the two disciplines’ observers.
Dice Similarity Coefficient. Center vertical plot shows the mean DSC values (solid dot) with standard deviations (line through dot) for each CT image, separated discipline. Tables adjacent to the plot indicate the numerical values of the mean and standard deviation. DSC values were obtained by pair-wise comparison of the observer contour and STAPLE consensus contour. The legend illustrates the distribution of thresholds used to identify different levels of agreement.
Radiomic feature robustness
A total of 1277 features were analyzed for robustness using the intraclass correlation coefficient (ICC) (2,1) calculated both with all 6 observers and separately with the observers of a single discipline. Of these, 143 were extracted from the original image as described in the methods section: 24 first-order, 17 shape, 22 intensity–volume histogram (IVH), and 80 texture features. As examples, the ICC values from radiation oncology contours for first order and shape features are shown in Fig. 3. ICC values from both discipline for all other original features are presented in Supplementary Figures S1–S7.
Comparing the single-discipline observer ICCs, varying degrees of difference were observed for different types of original radiomic features between radiation oncologist observers and radiology observers. For either discipline, relatively low ICCs were observed for some features. Overall, radiomic feature ICCs were lower within the radiology observers than the radiation oncology observers, indicating poorer robustness. Applying ICC ≥ 0.75 as the threshold for features considered robust, 48/143 (34%) original features were robust based on radiation oncology ICCs and 35/143 (24%) were robust based on radiology ICCs.
To observe the overall distribution of ICC values and compare between the two disciplines for all radiomic features, Fig. 4 shows the spread of single-discipline ICC values for all features based on image filters. Similar to the ICC values for the original features shown in Fig. 4, ICC values derived from either discipline also varied widely for all image types. The higher-order images included Laplacian of Gaussian (LoG), and 8 permutations of 3D wavelets (LLL, HLL, LHL, HHL, LLH, HLH, LHH, and HHH for low or high-pass in each of the three cardinal directions, respectively). The radiation oncology group showed higher average ICCs than the radiology group for all feature categories. Comparing different feature categories, wavelet features showed higher ICCs than original and LoG features, and LoG features showed the lowest ICCs. Out of 1277 features, 448 features (35%) and 214 features (17%) of radiation oncology and radiology derived features were considered robust, respectively. 205 of these features were robust for both disciplines.
The ICC statistics calculated for all features are also listed in Tables 1 and 2 for the radiation oncology and the radiology group, respectively. The feature count and number of robust features are reported for each feature class within each image filter type. As with Figs. 3 and 4, varying robustness were observed for different features and for different feature classes. The top three features with the highest ICCs within each image filter category are listed in Tables 3 and 4 for radiation oncology and radiology groups, respectively. Generally, these top robust features tend to come from certain texture categories such as those based on the run length matrix and the size zone matrix.
A Wilcoxon Signed-rank Test was used to measure the statistical difference between radiation oncology and radiology based ICC values for each image filter. All filters indicated a significant difference with p-values < 0.0001.
Feature ranking correlation between two disciplines
To evaluate relative feature robustness assessed by either discipline, we plotted the original feature ranking within each feature type for the two disciplines in Fig. 5. In other words, in Fig. 5a, for first order features, we plot out their robustness ranking based on radiation oncology observers and radiology observers. The feature rankings are similarly plotted out for other feature classes comparing the two disciplines. A perfect agreement between the two disciplines would result in a 45-degree linear regression of R2 = 1. Texture features included gray-level co-occurrence matrix (GLCM), gray-level run length matrix (GLRLM), gray-level size zone matrix (GLSZM), neighboring gray tone difference matrix (NGTDM), and neighboring gray-level dependence matrix (NGLDM). Among different feature classes, the highest degree of robustness ranking agreement was observed for intensity and histogram and shape features, with a R2 value of 0.93. Shape features also showed a good agreement with a R2 value of 0.74. Texture features showed poorer agreements, with the worst agreements seen for GLCM features and GLSZM features.
Discussion
To our knowledge, this is the first study addressing the degree of interobserver and interdisciplinary variation in tumor delineation and its effect on CT-derived radiomic feature stability in pancreatic cancer. Using the consensus contours generated based on six expert observers using the Simultaneous Truth and Performance Level Estimation (STAPLE) algorithm, the DSC values between individual observer’s and the consensus contours show considerable interobserver delineation variation for pancreatic cancer. Furthermore, significant interdisciplinary differences are observed between radiation oncology and radiology observer DSCs. These results are also reflected in the large variance of ICC values regardless of image filter and the statistically significant variance between disciplinary-based derived features. Not surprisingly, lower overall ICC values were observed for radiomic features derived from contours with lower DSC values with the consensus volume. This correlation suggests that radiomic feature robustness, and therefore, subsequent radiomic analyses, could be strongly influenced by interobserver delineation variability. But as the radiomic feature showed widely varying degrees of robustness against the interobserver delineation variability, excluding the unstable features in radiomic feature selection appear important for pancreatic cancer model development.
While Belli et al. assessed radiomic feature robustness due to interobserver variation in pancreatic cancer, FDG-PET/CT based contouring was used20. Thus, no direct comparison can be drawn with our study as the first of its kind to assess feature robustness due to interobserver variation from contrast-enhanced CT imaging. For low-contrast tumors such as pancreatic cancer, inter-observer delineation uncertainty could be quite different based on anatomy (CT imaging) versus on take-up (PET imaging). Therefore, it is not surprising that our study found lower ICCs than what was previously reported in the PET study. In Luisa Belli et al.’s study evaluating interobserver variability for 73 radiomic features from PET/CT images, 47% of radiomic features were considered robust using an ICC cutoff of 0.80. When considering only features from the non-filtered image in our study, 34% (Radiation Oncology) and 24% (Radiology) were considered robust with an ICC cutoff of 0.75. This difference can be attributed to the utilization of PET imaging, which likely improved tumor conspicuity. Comparing our results for pancreatic cancer with previous studies investigating radiomic feature robustness against segmentation variability in other sites such as breast, non-small cell lung cancer, glioblastoma, and liver, the ICCs are also considerably lower12,13,14,15,16,17,18,19,20,21,22. In comparison, Pavic et al. found 90% and 56% of radiomic features considered stable with an ICC cutoff of 0.80 despite interobserver variation in non-small cell lung cancer and head and neck squamous cell cancer, respectively12. The results indicate that although all these studies confirm that contour variability impacts radiomic feature stability and features show varying degrees of robustness, interobserver variability will likely be more dominating among different sources of uncertainty to impact radiomic feature reproducibility for pancreatic cancer than for other high-contrast cancers such as lung cancer.
Interestingly, our investigation also revealed a significant interdisciplinary delineation variation. This is to our knowledge the first study to investigate the existence of a specialty difference in segmentation for radiomics. Our results agree with previous report from Nq et al. on radiotherapy target delineation for post-operative head and neck cancer patients32 that a specialty difference does exist. We observe that the tumor volumes from the radiation oncology group tend to be larger than those from the radiology group. Despite our efforts to standardize the contouring experience, this could have resulted from radiation oncologists’ tendency to “not miss the target” in their training despite the common contouring guideline in this study to exclude any uncertain area. In addition, we found higher consistency among the radiation oncology group than among the radiology group, possibly stemming from the practice difference that volume segmentation is a routine activity in radiation oncology, but in radiology volume labeling is more important than whole volume segmentation. Among different classes of original radiomic features, the relative agreement between the two disciplines is better for first-order features and shape features than the texture features. These novel findings are important as vast majority of the current radiomic models are developed based on delineated volumes either from radiology or radiation oncology. Such interdisciplinary delineation uncertainties should be considered when the segmentation is done by a different specialty in model deployment than in model development. Some studies have suggested the use of semiautomatic segmentation to improve radiomic feature robustness against volume delineation14,15,16. However, the current semiautomatic segmentation methods’ effectiveness in low contrast regions such as that of pancreatic cancer in CT imaging may be more challenging.
There are some limitations to our study to consider. Intraobserver variability was not investigated in our study. The threshold ICC value of 0.75 was selected based on literature investigating radiomic feature robustness due to interobserver variation in other tumor sites12,13,14,15,16,17,18,19,20,21. With ICC thresholds between 0.7 and 0.9 seen in the literature, our study chose a threshold of 0.75 on the lower end, adding a small conservative margin to account for the increased difficulty in contouring pancreatic cancer compared to those in the aforementioned studies. The significance of this threshold with respect to its effect on radiomics analysis, however, has not been investigated. Additionally, our study evaluated feature robustness, but its effect on the latter phases of radiomics analysis and how best to address it were not included. Also, this investigation is based solely on CT images while MRI and PET images also provide additional information and are sometimes fused to CT for pancreatic tumor evaluation. However, as CT remains the dominating radiological imaging modality in clinical practice for pancreatic cancer, we chose to focus the current study on CT-based radiomics. In our study, CT scans of limited scanner types and acquisition parameters were selected to isolate the observer variability from variabilities of imaging factors. Similarly, a fixed window/level setting was imposed in our study, ensuring different observers’ contours were not affected by varying window/level settings individual observers may choose. Yet by doing so, our findings reflect the results obtained with our specific image acquisition, reconstruction, and display parameters, and may need validation before generalized to other cases. In addition, our radiomic feature results from 5 mm isotropic voxels could be affected by edge and partial volume effects, though the tumor volumes are relatively large with a mean volume of 50.4 cm3.
Overall, the results of our investigation contribute to the conversation necessitating more rigorous evaluation of volume reproducibility prior to radiomic feature analysis. Our site-specific findings for pancreatic cancer are important as feature robustness against segmentation uncertainty will likely play a more dominating role in the reproducibility of radiomics for such cancers. The novel discovery on interdisciplinary variations also introduces new considerations for the deployment of radiomics-based predictive models.
Methods
Study cohort
Under the approval of the Institutional Review Board of University of Nebraska Medical Center (IRB#091-01-EP and IRB#127-18-EP), the diagnostic contrast-enhanced CT scans from 21 pancreatic cancer patients were used for this study. The patients whose images were investigated in this study were all enrolled with informed consents in the Rapid Autopsy Pancreas Program at University of Nebraska Medical Center. To date, the program has collected unique tissue specimens within hours of death from over a hundred enrolled pancreatic cancer patients over the past decade. Retrospective analyses in this study were performed in accordance with the relevant guidelines and regulations as approved by the Research Ethics Committee of University of Nebraska Medical Center. From the patients with available contrast-enhanced CT images at the time of diagnosis, we selected the maximum number of patients imaged with the same line of CT scanners from a single vendor and acquired with the same acquisition protocol and slice thickness to minimize the effect of other uncertainty-contributing factors. This resulted in the 21 patients used in the study. These 21 patients included 1 stage IIA, 2 stage IIB, 1 stage III, and 17 stage IV patients.
Image acquisition and volume segmentation
For the 21 patients included in the study, the image acquisition was performed using one of the following three CT scanner models: Lightspeed VCT, Lightspeed Pro 16, and Lightspeed RT16 (GE Healthcare, Boston, Massachusetts, USA). Patients received ISOVUE injection with bolus triggering arterial phase imaging about 30 s and venous phase about 60 s after injection. A slice thickness of 5 mm was used for all patient acquisitions, and the in-plane resolution was between 0.6 and 0.9 mm.
Six expert observers, comprised of three radiation oncologists and three radiologists, each contoured the entire cohort. The three radiation oncologists have 21, 8, and 6 years of experience within their specialty, respectively, and the three radiologists have 19, 7, and 4 years of experience within their specialty, respectively. All observers in the study are experts in assessing/treating pancreatic tumors as their clinical and/or research specialization. For each patient, the tumor was contoured using the iPlan software (Brainlab AG, Feldkirchen, Germany). To standardize the delineation for individual observers, the following segmentation instructions were given:
-
Tumor: Only contour what you feel certain is the gross tumor. Where it is uncertain, exclude.
-
Exclude major vessels, stents, markers, and lymph nodes, if applicable.
-
A window width of 400 with level at 50 has been preset for all cases. Do not change the window/level.
-
Use only the assigned CT for contouring. Do not rely on the help of MR, or other CT data.
-
Complete contours independently.
All contours were visually inspected by a non-observer investigator. In a couple of instances, an individual contour deviated substantially from that of other observers’. The observer was asked to review their contour, with the option to edit if so chose, while still blinded from other observers’ contours.
Consensus volume generation and segmentation variability assessment
For each patient, a consensus volume was created using the STAPLE algorithm as a ground truth surrogate33. The STAPLE algorithm creates a consensus volume based on the volume delineations from all 6 observers.
The dice similarity coefficient (DSC) was used to quantify the degree of volume overlap between two volumes34. The calculation of the DSC value is defined in Eq. 1,
where of A and B are the two volumes for which the DSC is to be calculated, and \(\cap\) indicates the intersection of the two volumes. The DSC is between 0 and 1, with 1 indicating two identical contours and 0 indicating two completely different contours.
Because the DSC requires a pair-wise comparison, it was calculated for each observer contour to quantify the overlap with the consensus volume. A value of 1 indicates complete spatial overlap with the consensus volume, whereas a DSC of 0 indicates no overlap. For illustration purposes, the following scale was used to categorize the level of volume agreement: DSC ≥ 0.85 [High Agreement], 0.85 > DSC ≥ 0.70 [Medium Agreement], 0.7 > DSC ≥ 0.5 [Low Agreement], DSC < 0.5 [Very Low Agreement]. All DSC values were calculated using the Computational Environment for Radiological Research (CERR) in Matlab R2018b35.
Image processing and radiomic feature extraction
For this study, a panel of 1277 radiomic features were calculated using an adapted version of CERR implemented in Matlab R2018b. These features consisted of: first order (n = 24), shape (n = 17), texture (n = 80), and intensity–volume histogram (IVH) (n = 22), on the original image and with 9 filters applied: Laplacian of Gaussian (LoG, n = 126), and 8 permutations of 3D wavelets (LLL, HLL, LHL, HHL, LLH, HLH, LHH, and HHH totaling n = 1008). As the shape features stay invariant with image filters, they were excluded in counting LoG and wavelet features. Individual calculated values can be found in the Supplementary Dataset for all features extracted using CERR, which followed the recommendations provided by the image biomarker standardization initiative (IBSI)36. Before feature extraction, the voxels were made isotropic by resampling the images to 5 × 5 × 5 mm3 voxels using sinc interpolation. Images were discretized using a bin width of 25 and the texture matrices were calculated for all three dimensions (resulting in 26 directions, or 13 symmetrical directions) with a voxel offset of 1 for neighboring voxels.
Radiomic feature robustness evaluation
The intraclass correlation coefficient (ICC) was used to quantitatively evaluate the robustness of radiomic features due to interobserver variations. An ICC (2,1) was selected to account for two-way random effects with single measurements when assessing the absolute agreement37,38,39. ICC values were also calculated separately based on discipline (radiation oncology vs. radiology) to assess interdisciplinary effects.
Radiomic features with ICC values greater than 0.75 were considered reproducible and robust. All ICC values were calculated using the ‘irr’ package in RStudio40.
Ethics approval
The study was approved by the Institutional Review Board of University of Nebraska Medical Center (IRB#091-01-EP and IRB#127-18-EP).
Conclusion
Volume segmentation variability affects radiomic feature stability for CT-based radiomics studies in pancreatic cancer, as has been shown for other cancer sites. Considerably lower interobserver ICCs were found than for high-contrast cancer sites, suggesting a more dominating role segmentation uncertainty plays in radiomics for pancreatic cancer. A novel interdisciplinary variability is also observed on segmentation, introducing new considerations for the deployment of radiomics-based predictive models.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 69, 7–34. https://doi.org/10.3322/caac.21551(2019) (2019).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 71(1), 7–33 (2021).
Khan, F. et al. Treatment Planning in Radiation Oncology 4th edn, 1005–1006 (Wolters Kluwer, 2016).
Chaddad, A., Daniel, P., Desrosiers, C., Toews, M. & Abdulkarim, B. Novel radiomic features based on joint intensity matrices for predicting glioblastoma patient survival time. IEEE J. Biomed. Health Inform. 23, 795–804. https://doi.org/10.1109/JBHI.2018.2825027 (2019).
Linning, E. et al. Radiomics for classifying histological subtypes of lung cancer based on multiphasic contrast-enhanced computed tomography. J. Comput. Assist. Tomogr. 43(2), 300–306. https://doi.org/10.1097/RCT.0000000000000836 (2019).
Khalvati, F. et al. Prognostic value of CT radiomic features in resectable pancreatic ductal adenocarcinoma. Sci. Rep. 9, 5449. https://doi.org/10.1038/s41598-019-41728-7 (2019).
Zhou, J. et al. Predicting the response to neoadjuvant chemotherapy for breast cancer: wavelet transforming radiomics in MRI. BMC Cancer 20, 100. https://doi.org/10.1186/s12885-020-6523-2 (2020).
Traverso, A., Wee, L., Dekker, A. & Gillies, R. Repeatability and reproducibility of radiomic features: a systematic review. Int. J. Radiat. Oncol. Biol. Phys. 102(4), 1143–1158. https://doi.org/10.1016/j.ijrobp.2018.05.053 (2018).
Rizzo, S. et al. Radiomics: the facts and the challenges of image analysis. Eur. Radiol. Exp. 2(1), 36. https://doi.org/10.1186/s41747-018-0068-z (2018).
Kumar, V. et al. Radiomics: the process and the challenges. Magn. Reson. Imaging 30(9), 1234–1248. https://doi.org/10.1016/j.mri.2012.06.010 (2012).
Du, Q. et al. Radiomic feature stability across 4D respiratory phases and its impact on lung tumor prognosis prediction. PLoS ONE 14(5), e0216480. https://doi.org/10.1371/journal.pone.0216480 (2019).
Pavic, M. et al. Influence of inter-observer delineation variability on radiomics stability in different tumor sites. Acta Oncol. 57, 1070–1074 (2018).
Granzier, R. W. Y. et al. MRI-based radiomics in breast cancer: feature robustness with respect to inter-observer segmentation variability. Sci. Rep. 10, 14163. https://doi.org/10.1038/s41598-020-70940-z (2020).
Parmar, C. et al. Robust Radiomics feature quantification using semiautomatic volumetric segmentation. PLoS ONE 9(7), e102107. https://doi.org/10.1371/journal.pone.0102107 (2014).
Qiu, Q. et al. Reproducibility of radiomic features with GrowCut and GraphCut semiautomatic tumor segmentation in hepatocellular carcinoma. Transl. Cancer Res. 6(9), 940–948 (2017).
Homayounieh, F. et al. Semiautomatic segmentation and radiomics for dual-energy CT: a pilot study to differentiate benign and malignant hepatic lesions. AJR Am. J. Roentgenol. 215(2), 398–405. https://doi.org/10.2214/AJR.19.22164 (2020).
Owens, C. A. et al. Lung tumor segmentation methods: Impact on the uncertainty of radiomics features for non-small cell lung cancer. PLoS ONE 13(10), e0205003. https://doi.org/10.1371/journal.pone.0205003 (2018).
Choi, H. J. et al. Inter- and intra-observer variability in contouring of the prostate gland on planning computed tomography and cone beam computed tomography. Acta Oncol. (Stockh. Swed.) 50, 539–546. https://doi.org/10.3109/0284186X.2011.562916 (2011).
Tixier, F., Um, H., Young, R. J. & Veeraraghavan, H. Reliability of tumor segmentation in glioblastoma: impact on the robustness of MRI-radiomic features. Med. Phys. 66(8), 3582–3591. https://doi.org/10.1002/mp.13624 (2019).
Haarburger, C. et al. Radiomics feature reproducibility under inter-rater variability in segmentations of CT images. Sci. Rep. 10, 12688. https://doi.org/10.1038/s41598-020-69534-6 (2020).
Belli, M. L. et al. Quantifying the robustness of [18F]FDG-PET/CT radiomic features with respect to tumor delineation in head and neck and pancreatic cancer patients. Phys. Med. 49, 105–111. https://doi.org/10.1016/j.ejmp.2018.05.013 (2018).
Traverso, A. et al. Sensitivity of radiomic features to inter-observer variability and image pre-processing in Apparent Diffusion Coefficient (ADC) maps of cervix cancer patients. Radiother. Oncol. 143, 88–94. https://doi.org/10.1016/j.radonc.2019.08.008 (2019).
Caravatta, L. et al. Inter-observer variability of clinical target volume delineation in radiotherapy treatment of pancreatic cancer: a multi-institutional contouring experience. Radiat. Oncol. 9, 198. https://doi.org/10.1186/1748-717X-9-198 (2014).
Vinod, S. K., Jameson, M. G., Min, M. & Holloway, L. C. Uncertainties in volume delineation in radiation oncology: a systematic review and recommendations for future studies. Radiother. Oncol. 121(2), 169–179. https://doi.org/10.1016/j.radonc.2016.09.009 (2016).
Versteijne, E. et al. Considerable interobserver variation in delineation of pancreatic cancer on 3DCT and 4DCT: a multi-institutional study. Radiat. Oncol. 12, 58. https://doi.org/10.1186/s13014-017-0777-0 (2017).
Joo, J. M. et al. Preoperative CT classification of the resectability of pancreatic cancer: interobserver agreement. Radiology 293, 2. https://doi.org/10.1148/radiol.2019190422 (2019).
Zhao, B. et al. Reproducibility of radiomics for deciphering tumor phenotype with imaging. Sci. Rep. 6, 23428. https://doi.org/10.1038/srep23428 (2016).
Zhang, Y. et al. Radiomics-based prognosis analysis for non-small cell lung cancer. Sci. Rep. 7, 46349. https://doi.org/10.1038/srep46349 (2017).
Vallières, M. et al. Radiomics strategies for risk assessment of tumour failure in head-and-neck cancer. Sci. Rep. 7, 10117. https://doi.org/10.1038/s41598-017-10371-5 (2017).
Elhalawani, H. et al. Investigation of radiomic signatures for local recurrence using primary tumor texture analysis in oropharyngeal head and neck cancer patients. Sci. Rep. 8, 1524. https://doi.org/10.1038/s41598-017-14687-0 (2018).
Lu, Y. et al. Machine learning-based radiomic, clinical and semantic feature analysis for predicting overall survival and MGMT promoter methylation status in patients with glioblastoma. Magn. Reson. Imaging 74, 161–170. https://doi.org/10.1016/j.mri.2020.09.017 (2020).
Nq, S. P. et al. A prospective in silico analysis of interdisciplinary and interobserver spatial variability in post-operative target delineation of high-risk oral cavity cancers: does physician specialty matter?. Clin. Transl. Radiat. Oncol. 12, 40–46. https://doi.org/10.1016/j.ctro.2018.07.006 (2018).
Warfield, S. K., Zou, K. H. & Wells, W. M. Simultaneous truth and performance level estimation (STAPLE): an algorithm for the validation of image segmentation. IEEE Trans. Med. Imaging 23(7), 903–921. https://doi.org/10.1109/TMI.2004.828354 (2004).
Dice, L. R. Measures of the amount of ecologic association between species. Ecology 26, 297–302 (1945).
Apte, A. P. et al. Technical note: Extension of CERR for computational radiomics: a comprehensive MATLAB platform for reproducible radiomics research. Med. Phys. 45(8), 3713–3720 (2018).
Kwanenburg, A., Leger, S., Vallières, M. & Löck, S. Image biomarker standardisation initiative. eprint https://arxiv.org/abs/1612.07003 [cs.CV] (2016).
Koo, T. K. & Mae, Y. L. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15(2), 155–163. https://doi.org/10.1016/j.jcm.2016.02.012 (2016).
McGraw, K. O. & Wong, S. Forming inferences about some intraclass correlation coefficients. Psychol. Methods 1, 30–46 (1996).
Shrout, P. E. & Fleiss, J. L. Intraclass correlations: uses in assessing rater reliability. Psychol. Bull. 86, 420–428 (1979).
RStudio Team. RStudio: Integrated Development for R. RStudio, PBC, Boston. http://www.rstudio.com/ (2020).
Funding
Funding was provided by Center for Scientific Review(2P50CA127297-06A1).
Author information
Authors and Affiliations
Contributions
D.Z., C.L., and M.B. conceived the project. J.W. curated and analyzed the data. C.L., M.B., N.B., D.Z., L.Y., and V.D. performed expert contouring. J.W., S.W., D.Z. wrote the paper. M.A.H. provided expert knowledge and funding support. All authors edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wong, J., Baine, M., Wisnoskie, S. et al. Effects of interobserver and interdisciplinary segmentation variabilities on CT-based radiomics for pancreatic cancer. Sci Rep 11, 16328 (2021). https://doi.org/10.1038/s41598-021-95152-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95152-x
- Springer Nature Limited
This article is cited by
-
Notch appearance as a novel radiological predictor of transient expansion and good outcome of expanding schwannoma after radiotherapy
Discover Oncology (2024)
-
Deep neural network-based segmentation of normal and abnormal pancreas on abdominal CT: evaluation of global and local accuracies
Abdominal Radiology (2023)