Abstract
This study investigated the relationship of weather and air pollution with the onset of Bell’s palsy. The Korean Health Insurance Review and Assessment Service-National Sample Cohort (HIRA-NSC) data from 2002 through 2013 were used. The 3,935 Bell’s palsy patients were matched with 15,740 control participants. The meteorological data, including daily mean temperature (°C), daily mean highest temperature (°C), daily mean lowest temperature (°C), daily mean temperature difference (°C), relative humidity (%), spot atmospheric pressure (hPa), sulfur dioxide (SO2) (ppm), nitrogen dioxide (NO2) (ppm), ozone (O3) (ppm), carbon monoxide (CO) (ppm), and PM10 (particulate matter ≤ 10 μg/m3) for 60 days, 30 days, 14 days, 7 days, and 3 days prior to the index date were analyzed for Bell’s palsy cases and controls. Conditional logistic regression analysis was used to estimate the odds ratios (ORs) of the association between the meteorological data and Bell’s palsy. The mean NO2 and PM10 concentrations for 60 days were higher, while that of O3 was lower in the Bell’s palsy group than in the control group (both P < 0.001). The Bell’s palsy group showed 16.63-fold higher odds of NO2 for 60 days (0.1 ppm) than the control group (95% CI = 10.18–27.16, P < 0.001). The ORs of PM10, and O3 for 60 days showed inconsistent results according to the included variables. Bell’s palsy was related to high concentrations of NO2.
Similar content being viewed by others
Introduction
Bell’s palsy is defined as idiopathic peripheral facial paralysis1. The incidence of Bell’s palsy is approximately 11–40 per 100,000 person/year worldwide1. In Korea, approximately 0.12% of the population, regardless of age, suffers from facial palsy2. Viral infection and vascular compromise are thought to be related to Bell’s palsy3. Because both viral and cardiovascular causes might be influenced by meteorological factors, such as temperature and air pollution4,5,6,7, meteorological factors may have indirect effects on Bell’s palsy. In Korea, there is a traditional assumption that cold exposure causes Bell’s palsy8,9.
However, previous studies reported conflicting results regarding the association of Bell’s palsy and cold exposure3,10,11,12,13. Some researchers reported a high incidence of Bell’s palsy in cold weather10,11. On the other hand, others demonstrated a high incidence of Bell’s palsy in warm weather or no difference in incidence based on the weather conditions3,12,13. Most previous studies based their analysis on regional incidence rates without the consideration of individual factors, and they had small study populations3,10,11,12,13. To the best of our knowledge, no previous study has evaluated the effect of air pollution on Bell’s palsy. When the PubMed and EMBASE databases were searched through November 2019 for studies using the keyword phrase ‘(Bell’s palsy) AND (air pollution)’, two papers were identified; however, neither was relevant13,14.
The hypothesis of the present study was that meteorological conditions, including air pollution, could increase the incidence of Bell’s palsy. To test this hypothesis, the exposures of patients with Bell’s palsy and a control group to meteorological conditions were compared.
Results
The demographic factors, hypertension, diabetes, and dyslipidemia were identical between the Bell’s palsy and control groups. The mean meteorological and air pollution measurements for 60 days before the index date were evaluated. Only nitrogen dioxide (NO2), ozone (O3), and PM10 (particulate matter ≤10 μg/m3) showed differences (Table 1, each of P < 0.001).
The odds ratio (OR) of the 60-day NO2 exposure level (0.1 ppm) prior to the onset of Bell’s palsy was 16.63 (95% CI = 10.18–27.16, P < 0.001, Table 2). The OR of the 60-day PM10 exposure level (10 μg/m3) prior to the onset of Bell’s palsy was 1.07 (95% confidence interval [95% CI] = 1.04–1.11, P < 0.001), while that of O3 was 0.18 (95% CI = 0.10–0.31, P < 0.001). The daily mean temperature, daily mean highest temperature, daily mean lowest temperature, daily mean temperature difference, relative humidity, spot atmospheric pressure, SO2, and CO were not different between the Bell’s palsy and control groups (S1 Table). After performing several analyses of the associations between various levels of exposure to NO2, O3, and PM10 and Bell’s palsy, 60-day exposure levels of NO2, O3, and PM10 prior to the onset of Bell’s palsy were selected based on the Akaike information criterion (AIC) and Bayesian information criterion (BIC) values (S2 Table).
In the various models (models 1–7, Table 2), the results for NO2 were consistent, while those of O3 and PM10 were changed according to the variables included in the different models.
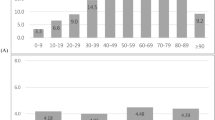
In the subgroup analyses, the 60-day exposure level of NO2 (0.1 ppm) was associated with an increased risk of Bell’s palsy in young women (OR = 68.17, 95% CI = 10.94–424.57, P < 0.001), middle-aged men (OR = 27.84, 95% CI = 11.22–69.10, P < 0.001), middle-aged women (AOR = 12.53, 95% CI = 4.96–31.66, P < 0.001), old men (OR = 12.93, 95% CI = 2.87–58.24), and old women (OR = 20.05, 95% CI = 6.20–64.82) groups (Table 3). However, statistical significance was not reached in the group of young men. According to the region of residence, there was an association between the exposure to NO2 with an elevated risk of Bell’s palsy in both urban and rural residents (S3 Table).
Discussion
The concentrations of NO2 for 60 days before the onset of Bell’s palsy were higher in Bell’s palsy patients than in the control group in this study. Other meteorological factors, such as temperature, humidity, atmospheric pressure, SO2, and CO, were not associated with Bell’s palsy. The results for O3 and PM10 were inconsistent (S4 Table). To the best of our knowledge, there has been no study on the association of air pollutants with Bell’s palsy.
The oxidative stress and inflammatory response to NO2 exposure may directly influence the development of Bell’s palsy. The cumulative effects of high concentrations of NO2 might contribute to the increased risk of Bell’s palsy. It was reported that patients with Bell’s palsy had higher levels of oxidative stress and antioxidant activity than patients in the control group15,16,17. Patients with Bell’s palsy had increased blood levels of thiol and disulfide activity levels compared to control participants16. In addition, the serum levels of malondialdehyde and the antioxidants glutathione, catalase, and superoxide dismutase were elevated in Bell’s palsy patients17. The increased level of oxidative stress may elevate an individual’s susceptibility to inflammatory neuropathy. Bell’s palsy is likely accompanied by an inflammatory response. The neutrophil-to-lymphocyte ratio was found to be higher in Bell’s palsy patients, and the ratio was correlated with the House-Brackmann grade of facial palsy and facial nerve enhancement on temporal gadolinium-enhanced magnetic resonance imaging18. NO2 can oxidize other organic compounds, including unsaturated fatty acids, thereby inducing free radical reactions19. The expression of numerous genes related to oxidative stress, including heme-oxygenase 1, was increased after NO2 exposure in primary human bronchial epithelial cells20. Moreover, systemic inflammation can be induced by NO2 exposure. A previous study reported that the serum interleukin-6 concentration was increased 1.20-fold after relatively higher levels of NO2 exposure (95% CI = 1.1–1.3, P = 0.001)21.
The elevated cardiovascular risk due to NO2 might represent an indirect link between NO2 and the risk of Bell’s palsy. NO2 is known to be associated with the risk of cardiovascular diseases, such as stroke and myocardial infarction, and cardiovascular mortality22,23. A meta-analysis study reported that there was increased cardiovascular mortality following long-term NO2 exposure (hazard ratio = 1.03, 95% CI = 1.02–1.05)23. Among several air pollutants, namely, CO, NO2, PM10, PM 2.5, and SO2, only NO2 was associated with an increased risk of hospital admissions for non-myocardial infarction-related cardiovascular disease (2.0%, 95% CI = 1.1–2.9) and heart failure (4.4%, 95% CI = 2.0–6.8)24. Another longitudinal follow-up study demonstrated an excess relative risk of hospital admissions of 2.8% for myocardial infarction and 4.9% for hemorrhagic stroke22. Several epidemiological studies have suggested the association of cardiovascular diseases with Bell’s palsy25,26. The incidence of peripheral arterial occlusive disease was 1.5 times higher in Bell’s palsy patients than in the control group25. Patients with Bell’s palsy had a 2.02-fold higher risk of stroke than the control group (95% CI = 1.42–2.86)26.
Similarly, PM10 was found to induce oxidative damage by increasing the intracellular level of hydrogen peroxide and decreasing catalase activity in human lung epithelial A549 cells27. In addition, PM suppressed the anti-inflammatory functions and innate immune neutrophils to endotoxins of lipopolysaccharides28. PM10 also had detrimental effects on cardiovascular diseases. A 10 µg/m3 increase in PM10 concentration was related to a 10.10% increase in the incidence of ST-elevation myocardial infarction29. This increase in the incidence of cardiovascular disease could be related to the risk of Bell’s palsy. However, we did not find a consistent result of association between PM10 and Bell’s palsy after adjustment for NO2 and O3. There was no previous study evaluated the relation between PM10 and Bell’s palsy, as far as our knowledge. However, possible explanations of the inconsistency in this study include the higher impact of NO2 than that of PM10 on the risk of Bell’s palsy and relatively small differences on the PM10, which could attenuate the statistical power. More studies are required to explore the relationship between PM10 and Bell’s palsy.
Because we could not find any previous study that evaluated the association between O3 and Bell’s palsy, we were unable to explain their inverse association. We believe this might be affected by the negative relationship between NO2 and O3, as O3 could be created from NO2 by photolysis via ultraviolet light30. Actually, the relative concentration of NO2 is higher than that of O3 in Korea31. Therefore, the dominant effect of NO2 on Bell’s palsy might be able to conceal the effects of O3 on Bell’s palsy. On the other hand, there is a possibility that O3 might actually reduce the risk of Bell’s palsy, as ozone therapy has been reported to affect facial nerve palsy32.
Other meteorological conditions, including temperature, atmospheric pressure, and humidity, did not show associations with Bell’s palsy in the present study. In accordance with our results, some prior studies demonstrated that there was no association between weather conditions and the onset of Bell’s palsy13,33. On the other hand, other previous studies reported relationships between Bell’s palsy and low temperature and atmospheric pressure34,35,36. However, many previous studies did not assess individual-level factors, such as comorbidities. Instead, these studies only analyzed the regional incidence of Bell’s palsy according to seasons or months34,35,36. In addition, the effects of air pollutants could be influenced by weather conditions. For instance, the synergistic effects of temperature and air pollutants on mortality due to cardiovascular or respiratory diseases have been reported37,38. Thus, air pollutants should be included when evaluating the effects of weather conditions on health outcomes. However, most previous studies did not concurrently consider air pollutants and weather conditions.
Unlike previous studies, this study matched and adjusted for individual-level demographic factors and past medical histories. The region of residence was matched between the Bell’s palsy group and the control group. In addition, the subgroup analyses according to region of residence demonstrated consistently high ORs for the association of the risk of Bell’s palsy with NO2 exposure in both the urban and rural groups (Table S3). A number of weather conditions, such as temperature, humidity, and atmospheric pressure, and the air pollutants, namely, SO2, NO2, O3, CO, and PM10, were simultaneously analyzed. There are several additional merits of the present study. With regard to the meteorological conditions, the accuracy of the measurements was guaranteed by using an automated synoptic observing system and a manual system hourly in 94 and 273 places, respectively (Supplementary S5). In addition, longitudinal measurements extending 60 days before the index dates were analyzed. The best fit models for the associations of NO2, O3, and PM10 air pollutants with Bell’s palsy were identified with the AIC and BIC (Table S2). Moreover, the large, representative sample cohort enabled the analysis of a number of meteorological conditions with satisfactory statistical power. A large, nationwide, representative study was carried out based on National Health Insurance System (NHIS) data. Because all Korean citizens are legally registered and their medical records are managed by the NHIS, no participants were missing in the present study.
However, because the NHIS data are based on hospital or clinical visits, it is possible that subclinical cases could have been excluded from the present study. In addition, although there were numerous participants, the number of young (<30 years old) patients was relatively smaller than the number of older patients, which could be a cause of the nonsignificant association between exposure to air pollutants and Bell’s palsy in this age group (Table 3). Although we considered several demographic factors and comorbidities, there are still possible confounding factors that were not considered, including smoking and alcohol consumption. PM2.5 information was not available in this study because it was only measured after 2015 in Korea. Moreover, the intrinsic limitation of the analysis of meteorological exposure in an epidemiological study existed because the measures of meteorological exposures were based on residential areas and could not account for indoor exposure. However, outdoor exposure to nitrogen is thought to have a higher impact on health outcomes than indoor exposure39. Lastly, because the Bell’s palsy group was matched with a control group who lived in another urban/rural place, the other environmental factors specific to the respective residential areas, including air pollution or meteorological factors, could have influenced the increased risk of Bell’s palsy.
In conclusion, the exposure to NO2 for 60 days before the onset of Bell’s palsy was higher in Bell’s palsy patients than in the control group, while the results for exposure to O3 and PM10 were inconsistent. Other meteorological conditions, including temperature, humidity, atmospheric pressure, SO2, and CO, were not related to the onset of Bell’s palsy.
Materials and Methods
Participant Selection
This study was approved by the ethics committee of Hallym University (2017-I102). All methods were performed according the guidelines and regulations of the ethics committee of Hallym University. Written informed consent was waived by the Institutional Review Board. We describe the Korean Health Insurance Review and Assessment Service - National Sample Cohort (HIRA-NSC), meteorological data, and air pollution data in supplemental file 5.
From a total of 1,125,691 patients with 114,369,638 medical claim codes, the participants who were defined as having Bell’s palsy were selected for inclusion (n = 3,996). The Bell’s palsy participants were matched 1:4 with participants who had never been diagnosed with Bell’s palsy (control group). Age group, sex, income group, region of residence, and past medical histories (hypertension, diabetes, and dyslipidemia) were matched between the Bell’s palsy and control groups. In matching the region of residence (urban/rural), participants who lived in urban areas were matched with control participants who lived in another urban place. The same method was used for those who lived in rural areas. The control group participants were sorted using a random number generator. The matched control participants were presumed to be enrolled concurrently with each Bell’s palsy participant (index date). The Bell’s palsy participants for whom we could not identify sufficient numbers of matching participants were excluded (n = 61). Finally, 1:4 matching resulted in the inclusion of 3,935 Bell’s palsy participants and 15,740 control participants (Fig. 1).
Schematic illustration of the participant selection process that was used in the present study. Out of a total of 1,125,691 participants, 3,935 of Bell’s palsy participants were matched with 15,740 control participants for age, sex, income, region of residence, and past medical histories. Then, the Bell’s palsy and control participants were matched with the same meteorological data before the index date.
We analyzed the meteorological data for the mean exposures 60 days, 30 days, 14 days, 7 days, and 3 days before the index date in both Bell’s palsy and control groups.
Variables
Independent variable
The daily mean temperature (°C), daily mean highest temperature (°C), daily mean lowest temperature (°C), daily mean temperature difference (°C), relative humidity (%), spot atmospheric pressure (hPa), sulfur dioxide (SO2) (ppm), NO2 (ppm), O3 (ppm), CO (ppm), and PM10 (μg/m3) for 14 days, 10 days, 7 days, 5 days, and 3 days before the index date were analyzed (Table S2).
Covariates
The age groups were classified using 5-year intervals. The income groups were divided into 11 classes (class 1 [lowest income]-11 [highest income]). The region of residence was classified as urban and rural areas.
The past medical histories of the participants were defined using the 10th revision of the International Statistical Classification of Diseases (ICD-10) codes. Hypertension (I10 and I15), diabetes (E10-E49), and dyslipidemia (E78) were acknowledged if the participants were treated ≥2 times.
Dependent variable
Bell’s palsy was defined using the ICD-10 code (G510). Among the cases with this ICD-10 code, the participants who were treated ≥2 times and who were treated with steroids were defined as having Bell’s palsy.
Statistical Analyses
The rate of general characteristics between Bell’s palsy and the control group were compared using the chi-square test. The mean meteorological data 14 days before the index date was compared using an independent t-test.
To analyze the ORs of meteorological data for Bell’s palsy, conditional logistic regression was performed. The crude (simple) and adjusted (multiple) models were analyzed. The models were stratified by age, sex, income, region of residence, hypertension, diabetes, and dyslipidemia. The 95% CI was described. We describe the independent variables and the methods used to reach the final model in Supplemental Tables 2, 3, and 4.
We estimated a single pollutant model for NO2, O3, and PM10. Additionally, we calculated a combined model.
The participants were sub-grouped according to age and sex (young [0–29 years old], middle aged [30–59 years old], and elderly [60+ years old]; men, and women). An identical model was used in these analyses.
Two-tailed analyses were performed. and statistical significance was defined as P values less than 0.05. SPSS version 22.0 (IBM, Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) were used to conduct statistical analyses.
References
De Diego-Sastre, J. I., Prim-Espada, M. P. & Fernandez-Garcia, F. The epidemiology of Bell’s palsy. Rev. de. neurologia 41, 287–290 (2005).
Chang, Y. S., Choi, J. E., Kim, S. W., Baek, S. Y. & Cho, Y. S. Prevalence and associated factors of facial palsy and lifestyle characteristics: data from the Korean National Health and Nutrition Examination Survey 2010-2012. BMJ Open. 6, e012628, https://doi.org/10.1136/bmjopen-2016-012628 (2016).
Zhao, H. et al. Bell’s Palsy: Clinical Analysis of 372 Cases and Review of Related Literature. Eur. Neurol. 77, 168–172, https://doi.org/10.1159/000455073 (2017).
Boonarkart, C., Suptawiwat, O., Sakorn, K., Puthavathana, P. & Auewarakul, P. Exposure to cold impairs interferon-induced antiviral defense. Arch. Virol. 162, 2231–2237, https://doi.org/10.1007/s00705-017-3334-0 (2017).
Sun, Z., Chen, C., Xu, D. & Li, T. Effects of ambient temperature on myocardial infarction: A systematic review and meta-analysis. Env. Pollut. 241, 1106–1114, https://doi.org/10.1016/j.envpol.2018.06.045 (2018).
Mo, J. H. Association of Particulate Matter With ENT Diseases. Clin. Exp. Otorhinolaryngol. 12, 237–238, https://doi.org/10.21053/ceo.2019.00752 (2019).
Park, M., Lee, J. S. & Park, M. K. The Effects of Air Pollutants on the Prevalence of Common Ear, Nose, and Throat Diseases in South Korea: A National Population-Based Study. Clin. Exp. Otorhinolaryngol. 12, 294–300, https://doi.org/10.21053/ceo.2018.00612 (2019).
Jang, I.-S. Is it appropriate to exclude cold exposure from the risk factors of Bell’s palsy? Korean J. M. eridian Acupoint 23, 51–54 (2006).
Kim, H. S. et al. Association Between High Neutrophil to Lymphocyte Ratio and Delayed Recovery From Bell’s Palsy. Clin. Exp. Otorhinolaryngol. 12, 261–266, https://doi.org/10.21053/ceo.2018.01018 (2019).
Movahedian, B., Ghafoornia, M., Saadatnia, M., Falahzadeh, A. & Fateh, A. Epidemiology of Bell’s palsy in Isfahan, Iran. Neurosci. 14, 186–187 (2009).
Campbell, K. E. & Brundage, J. F. Effects of climate, latitude, and season on the incidence of Bell’s palsy in the US Armed Forces, October 1997 to September 1999. Am. J. Epidemiol. 156, 32–39 (2002).
Narci, H., Horasanli, B. & Ugur, M. Seasonal Effects on Bell’s Palsy: Four-Year Study and Review of the Literature. Iran. Red. Crescent Med. J. 14, 505–506 (2012).
Danielides, V. et al. Weather conditions and Bell’s palsy: five-year study and review of the literature. BMC Neurol. 1, 7, https://doi.org/10.1186/1471-2377-1-7 (2001).
de, D. J., Prim, M. P., Madero, R., Marcos, S. & Gavilan, J. Effect of atmospheric factors on the incidence of Bell’s palsy. Eur. Arch. Otorhinolaryngol. 259, 53–55, https://doi.org/10.1007/pl00007530 (2002).
Terzi, S. et al. Oxidative Stress and Antioxidant Status in Patients with Bell’s Palsy. J. Med. Biochem. 36, 18–22, https://doi.org/10.1515/jomb-2016-0033 (2017).
Babademez, M. A. et al. Thiol/disulphide homeostasis in Bell’s palsy as a novel pathogenetic marker. Clinical otolaryngology: official journal of ENT-UK; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial. Surg. 42, 239–244, https://doi.org/10.1111/coa.12701 (2017).
Bozan, N. et al. Serum levels of oxidative stress indicators and antioxidant enzymes in Bell palsy. Ear, nose, throat J. 97, E11–E14 (2018).
Kum, R. O. et al. Elevated neutrophil-to-lymphocyte ratio in Bell’s palsy and its correlation with facial nerve enhancement on MRI. Otolaryngology–head neck surgery: Off. J. Am. Acad. Otolaryngology-Head Neck Surg. 152, 130–135, https://doi.org/10.1177/0194599814555841 (2015).
Episodes, D. o. H. A. G. o. t. M. A. o. A. P. Third Report-Oxides of nitrogen. (1993).
Mirowsky, J. E., Dailey, L. A. & Devlin, R. B. Differential expression of pro-inflammatory and oxidative stress mediators induced by nitrogen dioxide and ozone in primary human bronchial epithelial cells. Inhalation Toxicol. 28, 374–382, https://doi.org/10.1080/08958378.2016.1185199 (2016).
Perret, J. L. et al. The Dose-Response Association between Nitrogen Dioxide Exposure and Serum Interleukin-6 Concentrations. Int J Mol Sci 18, https://doi.org/10.3390/ijms18051015 (2017).
Collart, P., Dubourg, D., Leveque, A., Sierra, N. B. & Coppieters, Y. Short-term effects of nitrogen dioxide on hospital admissions for cardiovascular disease in Wallonia, Belgium. Int. J. cardiology 255, 231–236, https://doi.org/10.1016/j.ijcard.2017.12.058 (2018).
Atkinson, R. W., Butland, B. K., Anderson, H. R. & Maynard, R. L. Long-term Concentrations of Nitrogen Dioxide and Mortality: A Meta-analysis of Cohort Studies. Epidemiol. 29, 460–472, https://doi.org/10.1097/EDE.0000000000000847 (2018).
Milojevic, A. et al. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart 100, 1093–1098, https://doi.org/10.1136/heartjnl-2013-304963 (2014).
Liou, L. S. et al. Increased risk of peripheral arterial occlusive disease in patients with Bell’s palsy using population data. PLoS one 12, e0188982, https://doi.org/10.1371/journal.pone.0188982 (2017).
Lee, C. C. et al. Increased stroke risk in Bell’s palsy patients without steroid treatment. Eur. J. Neurol. 20, 616–622, https://doi.org/10.1111/j.1468-1331.2012.03765.x (2013).
Yi, S., Zhang, F., Qu, F. & Ding, W. Water-insoluble fraction of airborne particulate matter (PM10) induces oxidative stress in human lung epithelial A549 cells. Environ. Toxicol. 29, 226–233, https://doi.org/10.1002/tox.21750 (2014).
Zhang, Y., Geng, S., Prasad, G. L. & Li, L. Suppression of Neutrophil Antimicrobial Functions by Total Particulate Matter From Cigarette Smoke. Front. Immunol. 9, 2274, https://doi.org/10.3389/fimmu.2018.02274 (2018).
Akbarzadeh, M. A. et al. The association between exposure to air pollutants including PM10, PM2.5, ozone, carbon monoxide, sulfur dioxide, and nitrogen dioxide concentration and the relative risk of develo** STEMI: A case-crossover design. Environ. Res. 161, 299–303, https://doi.org/10.1016/j.envres.2017.11.020 (2018).
Finlayson-Pitts, B. J. & James N. P. Jr. Atmospheric Chemistry: Fundamentals and Experimental Techniques. John Wiley & Sons, doi: (1987).
Kim, D.-S., Jeong, J. & Ahn, J. Characteristics in Atmospheric Chemistry between NO, NO 2 and O 3 at an Urban Site during MAPS (Megacity Air Pollution Study)-Seoul, Korea. J. Korean Soc. Atmos. Environ. 32, 422–434 (2016).
Ozbay, I. et al. Effects of ozone therapy on facial nerve regeneration. Braz. J. Otorhinolaryngol. 83, 168–175, https://doi.org/10.1016/j.bjorl.2016.02.009 (2017).
Jeon, E. J. et al. Effects of meteorological factors on the onset of Bell’s palsy. Auris, nasus, larynx 40, 361–365, https://doi.org/10.1016/j.anl.2012.10.008 (2013).
De Diego, J. I., Prim, M. P., Madero, R. & Gavilan, J. Seasonal patterns of idiopathic facial paralysis: a 16-year study. Otolaryngology–head neck surgery: Off. J. Am. Acad. Otolaryngology-Head Neck Surg. 120, 269–271, https://doi.org/10.1016/S0194-5998(99)70418-3 (1999).
Hsieh, R. L., Wang, L. Y. & Lee, W. C. Correlation between the incidence and severity of Bell’s palsy and seasonal variations in Taiwan. Int. J. Neurosci. 123, 459–464, https://doi.org/10.3109/00207454.2013.763804 (2013).
Kokotis, P. & Katsavos, S. Effects of Wind Chill Factor, Temperature and Other Meteorological Parameters on the Incidence of Bell’s Palsy: Results Based on a Retrospective, 7-Year Long, Greek Population Study. Neuroepidemiology 45, 44–49, https://doi.org/10.1159/000433542 (2015).
Qian, Z. et al. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environ. health Perspect. 116, 1172–1178, https://doi.org/10.1289/ehp.10847 (2008).
Stafoggia, M., Schwartz, J., Forastiere, F., Perucci, C. A. & Group, S. Does temperature modify the association between air pollution and mortality? A multicity case-crossover analysis in Italy. Am. J. Epidemiol. 167, 1476–1485, https://doi.org/10.1093/aje/kwn074 (2008).
Esplugues, A. et al. Outdoor, but not indoor, nitrogen dioxide exposure is associated with persistent cough during the first year of life. Sci. Total. Environ. 409, 4667–4673, https://doi.org/10.1016/j.scitotenv.2011.08.007 (2011).
Acknowledgements
This work was supported in part by a research grant (NRF-2018-R1D1A1A02085328 and NRF-2016M3A9E8941669) from the National Research Foundation (NRF) of Korea.
Author information
Authors and Affiliations
Contributions
H.G.C. designed the study, participated in data collection and data interpretation, and revised the manuscript. S.Y.K., J.C., B.P., and H.G.C. participated in the interpretation of the data and drafted and revised the manuscript. C.M. participated in data analysis, interpretation of data, and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, S.Y., Min, C., Choi, J. et al. Air pollution by NO2 is associated with the risk of Bell’s palsy: A nested case-controlled study. Sci Rep 10, 4221 (2020). https://doi.org/10.1038/s41598-020-61232-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-61232-7
- Springer Nature Limited
This article is cited by
-
Effect of temperature and air pressure on the incidence of Bell's palsy in Hangzhou: a distributed lag non-linear analysis
Scientific Reports (2023)
-
The Impact of Air Pollution and Aeroallergens Levels on Upper Airway Acute Diseases at Urban Scale
International Journal of Environmental Research (2022)
-
RETRACTED ARTICLE: Soil and water loss of mountain plants based on sensor and research on visual experience art
Arabian Journal of Geosciences (2021)
-
Assessment of contribution of SO2, CO, and NO2 in different urban land use in Bushehr region, Iran
Arabian Journal of Geosciences (2021)