Abstract
Drug-eluting stents are a commonly used treatment for coronary artery disease. However, the coatings used in drug-eluting stents have some limitations such as poor biocompatibility and drug loading capacity. In recent years, self-assembly methods have emerged as a promising alternative for stent coatings. Self-assembled coatings employ biomaterials and offer several advantages over traditional coatings, including thinner thickness, stronger binding capacity, and better biocompatibility. This review discusses the latest research on self-assembled biomaterial-based coatings for drug-eluting stents. We explore how layer-by-layer coatings and composite coating films have been utilized to load and release drugs with high drug loading capacity and biocompatibility, as well as how they promote endothelial adhesion and growth. Additionally, we examine how self-assembled coatings have been used to release active molecules for anti-coagulation and deliver gene therapy. Moreover, we discuss the potential of self-assembled coatings for future development, including intelligent targeted drug delivery, bionic stent coatings, and 3D printed stent coatings. These advancements have the potential to further improve the effectiveness of drug-eluting stents in treating coronary artery disease.
Similar content being viewed by others
Introduction
Cardiovascular disease has become a leading cause of death in recent years, and its mortality rate has been steadily increasing year by year1,2. Percutaneous coronary intervention is the method to treat blocked coronary arteries. Vascular stent is used in percutaneous coronary intervention which has been one of the most effective medical interventions to deal with coronary artery diseases3,4. The evolution of cardiovascular stent has gone through percutaneous transluminal coronary angioplasty, bare metal stent (BMS), radioactive stent, drug eluting stent (DES), degradable vascular stent, autologous generate stent (Fig. 1). The first successful percutaneous transluminal coronary angioplasty was performed in 1977. The occluded coronary artery was unblocked by inflating a balloon, but there were some limitations, such as vessel closure due to elastic recoil, and inability to provide durable support to the cardiovascular system. BMS as a solution emerged in 1987. Early stents were made from stainless steel (SS) or cobalt chromium and were classified as BMS. Since the stent is considered a foreign object, the body’s immune system may activate an inflammatory response by upregulating inflammatory mediators, leading to neointimal hyperplasia. As a result, the proliferation of vascular smooth muscle cells (VSMCs) can lead to restenosis of blood vessels and a reduction in coronary blood flow. Unfortunately, up to 15% to 20% of patients who undergo BMS implantation may require repeat revascularization within several months5,6. Therefore, the BMS is difficult to be used as a permanent implant. An alternative to BMS is the degradable vascular stent, which provides temporary support for the vessel and is fully resorbed without compromising revascularization7,8. Additionally, it is useful in restoring normal vasoconstriction that may have been lost after stent implantation9. However, further improvements are still needed in its degradation rate and mechanical support. In addition, the latest exploration of cardiovascular stent showed that decellularization and anti-thrombogenic coating of fibrotic conduits generated patent autografts, which remodeled into neoarteries. This offered an effective approach to obtain autografts for clinical therapy. The study also provided a direction for the research of autologously generated stents10. The concept of radioactive stent was proposed to address the issue of restenosis caused by BMS in 1989. Neointimal hyperplasia could be well treated by intravascular brachytherapy. However, the clinical trials showed the edge effect, which could lead to a reduced lumen just beyond the stent edge at an unacceptable rate. Although subsequent efforts have resulted in reduced the edge effect by increasing radioactive stent ends, coinciding with the encouraging development of DES. Most studies of radioactive stents have been abandoned. The use of DES gained the approval by FDA in 200311. DES uses polymer coatings to deliver anti-proliferative drugs, which can prevent restenosis. However, as the polymer coating deteriorates over time, it can lead to denaturation, deformation, shedding, and hypersensitivity reactions due to its poor biocompatibility. These factors can negatively affect the endothelialization process and lead to late stent thrombosis. While the development of degradable polymer coatings has reduced the time that the coating stays on the vascular wall, issues still remain, such as poor biocompatibility, susceptibility to deformation and shedding, and low drug loading capacity. These factors can result in poor endothelialization and an increased risk of thrombosis.
I Percutaneous transluminal coronary angioplasty, unblocking the included coronary arteries by inflating the balloon. In specific, BMS provides support for the unblocked coronary arteries, and radioactive stent can reduce restenosis by intravascular brachytherapy. DES can prevent restenosis through binding anti-proliferative drug with polymer coating, while degradable vascular stent supports the vessel at a set period and can be fully resorbed without affecting revascularization. Autologously generated stent effective produces highly patent autografts that remodeled into neoarteries to obtain autografts for clinical therapy.
To address these issues, significant modifications have been made to stents in various aspects. Among them, the self-assembled stent coating has shown unique advantages over other coatings. Self-assembled coatings can achieve non-polymer drug loading and can be more firmly fixed to the stent’s surface by directly bonding with the metal surface without deformation. The intermediate layer of the self-assembled layer-by-layer (LbL) coating, such as poly-dopamine, efficiently binds biomaterials to the stent surface. The LbL method can be used to create a complex polymer film containing biopolymers, which can be loaded with drugs and released in a controlled manner. This approach improves the drug loading capacity and biocompatibility of the stent, reducing complications after stent implantation (Fig. 2)12.
Anti-fouling by mutual repulsion of negative charges, anti-proliferative by loading drugs to cause cell-cycle arrest in the G1 phase, promoting endothelial adhesion and growth by loading vascular endothelial growth factor (VEGF)-loaded heparin/PLL particle, anti-coagulation by imitating ECs to release active molecules such as nitric oxide (NO), and gene therapy by controllable gene delivery.
Stent surface coating material
The ideal coating of stent would be a degradable material with good biocompatibility, which can promote the adhesion of endothelial cells (ECs) and inhibit the proliferation of VSMCs, and can carry drugs safely and controllably to achieve the required functions of antithrombotic and restenosis, and additionally can be firmly combined with the stent, and not easy to deformation and shedding. At present, DES mainly relies on polymer coating for drug loading. Polymer can be roughly divided into two categories: non-degradable polymer and degradable polymer, while degradable polymer includes degradable chemical polymer and degradable biopolymer.
At present, most of the materials of clinical stent coatings are degradable polymers, which have degradability, biocompatibility, drug delivery and cell response mediating capabilities (such as adhesion, proliferation and differentiation). Degradable chemical polymers (e. g, poly lactic acid (PLA), polycaprolactone, poly (L-lactic) acid (PLLA), polylactide glycolic acid copolymer (PLGA), polystyrene sulfonate (PSS), polyethylene glycol (PEG), disulfide cross-linked low molecular polyethylenimine (ssPEI), silane, etc.) do not have good cell affinity and cannot be completely degraded in vivo. Degradable biopolymers, such as poly-dopamine, poly-l-lysine (PLL), hyaluronic acid, chitosan, phosphorylcholine, and heparin etc., possess higher biocompatibility and other biological functions (such as anti-thrombotic, anti-proliferation, promoting EC adhesion, etc.), which can make up for the shortcomings of degradable chemical polymers4.
Due to the problems associated with non-degradable polymer coatings, such as their lack of degradability and poor biocompatibility leading to hypersensitivity, current research on stent coatings is mainly focused on degradable polymer coatings and non-polymer coatings. The molecules used in self-assembled coatings also fall into these two categories. Molecules commonly used in self-assembled coatings will be introduced in Self-assembled molecules for functional coatings.
The interfacial design of stent coating is essential. Stents are foreign to the human body, which may cause a cascade of immune and inflammatory responses when implanted. Although the emergence of DES has reduced some complications after stenting, chemical polymers used in DES may cause thrombosis and other problems. By choosing a suitable coating interface, the biocompatibility of the interface can be effectively improved and complications can be reduced. For example, the titanium surface was modified with heparin and collagen by the LbL technique13. The modified heparin-collagen interface can effectively improve the compatibility of titanium with blood. The biomolecule-based interfacial coating can effectively inhibit the accumulation of VSMCs without disrupting the endothelialization of vascular ECs. Therefore, by modifying the metal interface of the stent to a biomolecule-based interface, the function of anti-restenosis and thrombosis can be achieved14.
On the other hand, the coating should be able to change the drug release rate to achieve longer drug release from the entire drug delivery system. Through the effective control of the coating interface, the sustained release of the drug and long-term drug treatment effect can be achieved. First, reasonable design of the chemical structure and properties of the carrier molecule is a choice to achieve controllability. Secondly, controllability can be achieved by effectively controlling the thickness and number of layers of the coating15. For example, paclitaxel loaded hyaluronic acid-g-PLGA micellar aggregates formed by self-assembly in aqueous solution can realize the loading of hydrophobic antiproliferative drugs on the hydrophilic biopolymer interface and achieve long-term sustained release. In addition, high drug loading can be achieved through the interaction, such as ionic bonds and hydrogen bonds, of charged drugs with ionizing groups on the membrane interface, and the drug loading can also be easily adjusted by changing the number of layers16.
The stability and safety of the coating are also important factors. Some polymer coatings experience mechanical damage during stent expansion. It is suggested that by rational design of the coating interface, the coating adapt to required strength and ductility of the stent system, so that it can deform with the stent without breaking or falling off. For example, by using self-assembled monolayers (SAMs), paclitaxel can be stably fixed on the coating interface by chemical bonding, and a smooth and uniform coating can be formed on the stent surface. Due to interactions such as hydrogen bonds and covalent bonds at the coating interface, the polymer-free coating formed on the stent does not form defects after the stent is inflated by the balloon. Therefore, the stability and safety of the stent coating are effectively improved17,18.
Self-assembled molecules for functional coatings
Different functional molecules can endow the stent with different properties, and the coating molecules also affect the choice of the self-assembly method of the stent coating. According to the source of the coating molecules, functional molecules are mainly divided into chemical molecules and biomolecules. Chemical molecules come from artificial synthesis, and the size, length and functional groups of the molecules can be designed and synthesized according to the needs. Chemical molecules are mainly used to form self-assembled monolayers. Biomolecules are routinely used to form Layer-by-layer self-assembled monolayers and self-assembled coating based on dopamine.
Self-assembled chemical molecules for functional coatings
Chemical molecules are the main substances used in SAMs, and the coatings based on chemical molecules have good stability, uniformity and low thickness. At the same time, chemical molecule also has good flexibility with the length and headgroups designable according to the needs. Thiols, phosphonic acids and alkanoic acids are commonly used chemical molecules19,20,21,22. Thiols generally have strong chemisorption on Au (Fig. 3a); while coordination complexes can be formed between anions of phosphonic (Fig. 3b) or alkanoic acids (Fig. 3c) and cations of metal oxides. All of them can form biocompatible, tightly packed, and highly oriented self-assembled coatings that can be applied to a variety of metal stents, like Au, Ti and SS. The ordered and stable coatings formed by chemical molecules on the stents can withstand harsh chemical and mechanical conditions23,24. In addition, the ability to design the structure of molecule is the most favorable advantage of chemical molecules. Stents coatings with different properties can be obtained by designing and synthesizing molecules for modification with different headgroups and molecular chain lengths. Chan et al. 25 designed and synthesized one carboxyl-terminated amphiphilic macromolecules and two phosphonate-terminated amphiphilic macromolecules, and proved that different headgroups and molecular chain lengths could affect the grafting density and release ability of amphiphilic macromolecules on the stents surface. The data indicated that amphiphilic macromolecules with longer linker lengths formed monolayers with high surface coverage and thus higher bioactive loading on the substrate. For headgroups, phosphonate had stronger adsorption than carboxylate, and a more stable coating could be obtained by using phosphonate as the head group, therefore, the control of drug release and coating degradation could be achieved simply by changing the head group. On the other hand, variations in the phosphonate linker length had a more significant influence on adsorption than variations between headgroups, and the length of the linker directly affected the thickness, uniformity and roughness of the coating. As a consequence, the hydrophilicity, biocompatibility and hemocompatibility of the stent coating can be controlled by changing the length of the linker. In short, chemical structures that can be designed and synthesized on demand bring more controllability for surface modification of stents.
Self-assembled biomolecules for functional coatings
Compared with chemical molecules, biomolecules have better biocompatibility and safety, and some biomolecules also have therapeutic functions. Accordingly, the modification based on biomolecules is more widely used. Non-degradable polymers are associated with various problems such as late thrombosis and in-stent restenosis (ISR), and it is a good choice to use biomolecules as coating materials that can be degraded and have better biocompatibility. Well adopted biomolecules include dopamine (Fig. 3d), heparin (Fig. 3e), collagen and chitosan (Fig. 3f). Inspired by the adhesion strategy of marine mussels, the self-polymerization of dopamine was proved to be a simple and effective method for surface modification of biomaterials. Due to the strong adhesion and biocompatibility of poly-dopamine, poly-dopamine can be used to bind a variety of functional molecules to the surface of biomedical materials26,27,28,29. As an excellent carrier, poly-dopamine is widely used in self-assembled coatings. It can not only be used alone to form coatings and combine drugs, but also serve as the basis for the formation of self-assembled coatings. First, poly-dopamine adhered to the stents, providing necessary groups and electrostatic adsorption for the subsequent self-assembly process. The self-polymerization of dopamine mainly occurs in alkaline solution (e.g., pH 8.5), which is not suitable for alkali-sensitive materials, and its polymerization takes a long time, and its polymerization process can be improved by electrochemical assistance30,31. Cardiovascular material studies have shown that heparin can prevent intimal hyperplasia and reduce inflammation by inhibiting proliferation and migration of VSMCs. At the same time, heparin has many sulfo and carboxyl groups, which give heparin a negative charge13,32,33,34. The therapeutic function of heparin can inhibit restenosis, and its negative charge makes it suitable for LbL coatings. Collagen, a fibrin, is a major component of mammalian connective tissue, and it contains a large amount of alkaline amino acid lysine that gives the protein a positive net charge at pH 4 (zeta potential ~ +7 mV). Collagen is often used together with heparin to form LbL coatings13,15,35. Chitosan, which is the second largest natural resource after cellulose, widely exists in shrimp shells and cells, and has good biocompatibility and biodegradability. Like collagen, chitosan is often used with heparin through LbL technology to form a coating with anti-adhesion and antibacterial properties11,36,37. Compared with non-degradable polymers, the biocompatibility and therapeutic function of degradable biopolymers can effectively reduce the occurrence of inflammation, thrombosis and restenosis.
Self-assembly methods for functional coating
Thrombosis and restenosis caused by BMS are still the main problems in the clinical application of cardiovascular stents, and surface modification is one of the main methods to solve this problem. A straightforward approach is to use materials with higher biocompatibility and stability to improve the physicochemical properties of stents, such as metal oxides, metal hydroxides, and graphene oxide (GO). However, such coatings are fragile and their function is insufficient, after balloon catheter expansion, the produced small fragments may block the blood vessels4. Although the flexibility, degradability, and abundant functional groups of polymer coatings can help solve these problems, the bonding strength of polymers to stents is weak. It has been reported that polymer coatings are associated with some adverse clinical reactions, such as late stent thrombosis, etc.4,38 Therefore, it may be safer to eliminate the polymer carrier of the stent. Coatings based on self-assembly can provide good drug loading and release effects without polymer carriers. Several common self-assembly coatings include direct coating based on physical adsorption and crystallization (Fig. 4a), self-assembled monolayers (Fig. 4b), layer-by-layer self-assembled monolayers (Fig. 4c), and self-assembled coating based on dopamine (Fig. 4d).
Direct coatings based on physical adsorption and crystallization
Direct coating mainly refers to the coating formed on the surface of the stent by the adhesion or crystalline properties of the drug without a carrier. The fabrication process of direct coating is simple, and it is the basic technology for forming surface coating of metal stents. paclitaxel, as a drug for the treatment of in-stent restenosis (ISR), has been shown to be strongly adsorbed to different materials, including glass, polypropylene, silicones, polytetrafluoroethylene, and metals, etc. 39,40,41 Mani et al. used the natural adhesion properties of paclitaxel to directly coat cobalt-chromium (Co-Cr) alloy, and 56-day in vitro drug release studies proved that paclitaxel could coat Co-Cr alloy without the use of a carrier surface and achieve release (Table 1)41. Besides adsorption, agglomeration and aggregation of crystals is another method of direct coating. One mechanism for agglomerate growth is attributed to growing nuclei colliding and becoming “cemented” together by continuing growth between two or more crystals. Thus, drug coatings can be formed by crystallization. In addition, amorphous drugs are in a metastable state and have higher energy levels, so the chemical stability of crystalline drugs is better than that of amorphous drugs. Therefore, the crystalline drug can improve the chemical stability of the drug coating on the stent, while prolonging the drug release time42,43,44. Levy et al. reported a method of coating rapamycin (RM) on stents by temperature induced bulk crystallization process, and achieved slow-release of RM (Fig. 5a)43. Farah et al. used RM as a model drug and improved the surface crystallization method44. Stents were first coated with seeds, and RM was crystallized using seeds as starting nucleation points. A uniform, continuous and highly crystalline controllable coating was obtained (Fig. 5b), and RM constantly released up to 90 days (Fig. 5c).
Self-assembled monolayers
There have been some reports on the issue of polymer carriers for DES: (1) Food and Drug Administration issued a warning about polymer-coated DES, which may cause late stent thrombosis, where increased oxidative stress levels contribute to thrombosis, or blood clot formation that may occlude the vessel; (2) Several cases about hypersensitivity reactions associated with polymer-coated DES have been reported, with symptoms including rash, dyspnea, urticaria, itching and fever; (3) After balloon catheter dilation, mechanical defects such as cracks, peeling, irregularities, and waving were observed in the polymer coating of commercially available DES45,46,47,48,49,50. Although there are still arguments on advantages and disadvantages of polymer carriers for DES, the development of safer stent-based drug delivery approaches is still a focus of intensive research, towards elimination of the possible adverse reactions of polymer carriers for DES to patients. SAMs, as a typical polymer-free platform with a thickness of 1–10 nm, have significant advantages in reducing the size of stents compared to the micron-scale general coatings (Table 1)38. Moreover, SAMs can provide high graft density and controllable surface structure to the stents, and the structure of coating molecules can be designed according to the needs for controllably improving the surface properties of the stents. SAMs can also expand or contract uniformly with the stent, so it can effectively solve the fracture and fragmentation of the stent coating25,51. Meanwhile, SAMs can be formed on various material substrates such as metals and metal oxides, which is beneficial for their application in stents52. First, based on the strong adsorption between sulfur compounds and Au, Lee et al. utilized SAMs technology to couple functional sulfur compounds on Au layers deposited on stents19. Heparin was also immobilized on functional sulfur compounds. In vitro tests showed that the adsorption amount of the model protein decreased from 0.56 μg/cm2 on the SS surface to 0.20 μg/cm2 on the coated surface, and the platelet adhesion rate decreased from 42% on the SS surface to 13% on the coated surface. Compared to the control group, only about 10% of the total VSMCs adhered to the coated surface and they did not proliferate. It is demonstrated that the coating can enhance biocompatibility and help reduce thrombosis and inhibit restenosis. Ti is a widely used material in the biomedical field, and self-assembled monolayers on Ti are becoming the focus of research. As shown in Fig. 6a, Mani et al. utilized two metal/SAM systems (Au/thiol and Ti/phosphonic acid) to coat hydroxyl-terminated SAMs on Au and Ti surfaces53,54. Therapeutic SAMs were subsequently prepared by adsorbing the model drug flufenamic acid on the SAM-coated metal surface using three different esterification methods, including acid chloride esterification, dry heat esterification, and direct esterification. Experimental results showed that human aortic EC continued to proliferate on the coated metal surface and reached more than 90% confluence on the surface after 7 days. This proved that the coating favors endothelialization without causing adverse effects. SS stents are widely used, so it is very important to study the formation of SAMs on their surfaces. Because the SS surface is not active enough to deposit SAMs, surface pretreatment is required to improve its hydrophilicity. In addition to chemical treatment with water, ethanol, acetone, and chloroform, Mahapatro et al. used gas plasma treatment after chemical treatment, the contact angle value of the metal surface after treatment decreased from 64 deg to 3 deg, and the hydrophilicity of the metal surface was greatly improved55,56,57. Hydroxy-terminated alkanethiol SAMs were formed on SS and ibuprofen was attached to the functional SAMs using Novozume-435 as a biocatalyst (Fig. 6b). In terms of drug release kinetics, unlike the initial burst of drug release in polymer encapsulated drug delivery systems, a steady increase in drug being eluted was observed in SAMs coatings. It was proved that the SAMs coating can effectively achieve stable drug release. In short, due to the strong chemisorption between thiols, phosphonic acids and alkanoic acids with metal stents, they can form biocompatible and closely packed SAMs on the surface of various metal stents19,21,22.
Layer-by-layer self-assembled monolayers
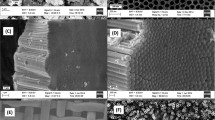
In addition to using polymer-free coatings to solve the problems of polymer coatings, using natural biopolymers to reduce thrombosis and inflammation is another idea. It is important to ensure the structural and functional integrity of the biomolecules during the coating fabrication process. In 1991, Decher et al. 58,59 proposed the electrostatic alternating deposition technique. They used electrostatic interaction to alternately adsorb oppositely charged polyelectrolyte solutions to prepare LbL monolayers. The method has the advantages of simple preparation, maintainability of the activity of biomacromolecules, and adaptability to substrates of any size and shape, so it is increasingly used in medical field60,61. LbL technology can spontaneously form coatings with complete biomolecular structures and functions on the surface of stents. In addition, LbL technology can precisely control the mechanical properties and coating thickness of multilayer films by controlling the number of adsorption layers (Table 1). At the same time, the multi-layer structure also has a larger drug load and sustained release effect. Chen et al. 13 first deposited a layer of positively charged PLL on the Ti surface and treated it with NaOH to change the charge, and then alternately deposited heparin and collagen to form a multilayer film. It was shown that the number of platelets adhered to the coated surface was about half of that of the untreated Ti surface by determination of the lactate dehydrogenase release after lysis of the adherent blood platelets (Fig. 7a). Fluorescent staining for P-selectin proved that the activated platelets on the Ti surface (Fig. 7b і) were much more than those on the coated surface (Fig. 7b іі). These all indicated that the coating enhanced the in vitro anticoagulant properties of Ti and was expected to reduce the risk of thrombosis during long-term implantation. In addition to good biocompatibility, LbL technology could also realize the function of drug loading, Kim et al. 16 used a bioinspired mussel adhesion mechanism to stably modify heparin on the surface of Co-Cr alloy and paclitaxel eluting multilayer composed of anionic poly(lactic-co-glycolic acid) grafted hyaluronic acid micelles, heparin, and PLL were constructed by LbL technology (Fig. 7c), and the substrate was completely covered by the coating with a thickness of about 3 μm (Fig. 7d і and іі). The sustained release of paclitaxel could be as long as 24 days, and the proliferation of human coronary artery VSMCs was successfully prevented. In vitro EC culture results showed that the multilayer modified surface could promote EC adhesion and proliferation. Modification of biomolecules could improve the deficiencies of biomolecules. Yang et al. 62 modified collagen to reduce its inherent thrombotic effect, and developed a recombinant human type III collagen (hCOLIII) that retained its affinity for EC without the presence of platelet binding sites. In this work, hCOLIII and hyaluronic acid were coated on the stent surface by means of LbL technology (Fig. 7e). Compared with the large amount of platelet adhesion of the animal-derived collagen, there was almost no platelet adhesion after the hCOLIII-based coating, and hCOLIII effectively improved the thrombus protection properties. LbL technology-based stent coating can bind biomolecules well and exhibit excellent performance that is expected to be widely used in clinical practice.
a Number of adherent platelet on surfaces of Ti and coating, b Fluorescence microphotographs of activated platelets adhered on (і) Ti, and (іі) coatings13. Copyright © 2009 Elsevier. c Schematic illustration of LbL coating on Co-Cr alloy, d SEM images of assembled coating on stent: (і) coating and (іі) cross-sectional view of coating16. Copyright © 2009 American Chemical Society. e Preparation of coatings by alternate deposition of hyaluronic acid and hCOLIII62. Copyright © 2021 Elsevier.
Self-assembled coating based on dopamine
Different from the several self-assembled coatings introduced above, there are two formation pathways for poly-dopamine (Fig. 8a). The first pathway is chemical action. Dopamine forms a polymeric structure through oxidative polymerization; Second, physical action is another pathway. Due to intermolecular physical action, dopamine molecules and dopamine oxidation intermediates can form mixtures through self-assembly, so poly-dopamine is subject to the combined action of covalent and non-covalent forces63,64. Therefore, we think that the adhesion of the dopamine coating to the substrate is the combined effect of the polymerization of dopamine and the surface self-assembly of small dopamine molecules. Fan et al. 65 immobilized nanoscale copper-based metal organic frameworks (Cu-MOFs) to cardiovascular stents using poly-dopamine as a linker and coating matrix, such coating inhibited platelet aggregation and activation via NO-cGMP signaling pathway, and significantly reduced thrombosis in an in vitro extracorporeal circulation model (Fig. 8b). In addition, the coating could inhibit the proliferation of VSMCs and macrophages, and reduce intimal hyperplasia, which could effectively prevent late thrombosis and restenosis after stent implantation. Tan et al. 66 immobilized heparin/PLL nanoparticles loaded with VEGF on the surface of SS modified with dopamine coating by Schiff’s base reaction. The coating could prevent growth of VSMCs, and exhibited good biocompatibility. Ma et al. 67 first covered the stent surface with poly-dopamine, and then chemically cross-linked the surface with polyamine to form a coating. Based on carbodiimide chemistry, Cu-DOTA and heparin were covalently grafted onto the stent coating, the high chemical stability of both the coating and Cu-DOTA complex imparted the endothelium-mimicking stents with about 62.4% of heparin bioactivity retention and up to 81.3% of catalytic activity of NO after application for 1 month. In addition to using dopamine alone to generate the coating, the performance of the coating could also be improved by copolymerization. Yang et al. 29 used a one-pot method to form a NO-generating coating on SS by the copolymerization of selenocystamine and dopamine (Fig. 8c). With simple production process, high stability and no organic solvent involved, the developed polymer coating could release NO in a controllable and stable manner for more than 60 days. NO generation enhanced the adhesion, proliferation and migration of EC, and achieved rapid in vivo re-endothelialization, effectively reducing ISR and neointimal hyperplasia. The time-consuming fabrication of dopamine coatings is a major disadvantage. To this end, Wang et al. 31 improved the polymerization process of poly-dopamine by means of electrochemical assistance, and formed a continuous and smooth electropolymerized poly-dopamine coating on the surface of the substrate, and then functionalized the coating by VEGF. The electrochemical method had a high deposition rate and efficient dopamine utilization, in vitro and in vivo studies showed that the functionalized coating can prevent the formation of neointima after stent implantation. The advantages of dopamine-based self-assembled coatings are their universal applicability, adhesion stability, and biocompatibility (Table 1).
a The synthesis of poly-dopamine is achieved by the covalent bond-forming oxidative polymerization and the physical self-assembly of dopamine and 5,6-dihydroxyindole63. Copyright © 2012 Wiley. b Preparation of nano Cu-MOFs-immobilized coating on cardiovascular stents by polymerization of dopamine65. Copyright © 2019 Elsevier. c Mussel-inspired selenocystamine-dopamine coatings forms on cardiovascular stents29. Copyright © 2018 Elsevier.
Functionalities and applications of self-assembling approaches
After stent implantation, the main challenges are poor healing following endothelial injury, late thrombosis, and restenosis due to abnormal proliferation of VSMCs. To address these issues, self-assembled stents have been developed, which can load anti-proliferative drugs, promote endothelial adhesion and growth, and mimic ECs to release active molecules such as NO for anti-coagulation. These stents have several advantages, and research has shown promising results. Finally, its progress in gene therapy is also described.
Functionalities
The self-assembled coating has the advantages of strong bonding ability and flexible assembled complex film coating, it can combine anti-corrosion polymer, anti-fouling polymer, biopolymer to the surface of the stent to achieve the purposes of anti-corrosion, anti-fouling, and improving the biocompatibility of polymer coatings.
Corrosion resistance
Magnesium (Mg) alloy degradable stents have shown limited success due to their rapid corrosion rate, which can cause loss of mechanical integrity before optimal vascular remodeling is achieved. However, excellent anti-corrosive coatings can help to slow down the corrosion of Mg alloys79. The heparin-functionalized GO is negatively charged. Chitosan is a positively charged bioactive material. Immobilizing chitosan on Mg alloys can also improve the corrosion resistance80. In addition, there are lots of amino groups on chitosan. The negatively charged heparinized GO can interact with the amino groups to form multilayer coating. Gao, et al. constructed a chitosan/heparinized GO multilayer coating on the AZ31B Mg alloy surface by using LbL method. The SEM images of different samples immersed in SBF for 1, 3, 7, and 14 days showed that increasing the thickness of chitosan/heparinized GO coatings could enhance the corrosion resistance of the Mg alloy and regulate the biodegradable behaviors (Fig. 9c, d)81.
Dopamine is a high-adhesion protein64. Poly-dopamine synthesized via dopamine self-polymerization can combine with various biological molecules82, and is often used as an intermediate layer by LbL assembly for additional surface functionalization to promote biocompatibility and adhesion. To improve the adhesion of hyaluronic acid coatings on Mg substrate, Li et al. used poly-dopamine coating as the intermediate layer to prepare hyaluronic acid coating on the ZE21B alloy83. The results showed that the poly-dopamine/hyaluronic acid coating had better corrosion resistance and more pro-endothelialization ability. Besides, the poly-dopamine/hyaluronic acid coating enhanced blood compatibility, anti-hyperplasia and anti-inflammation functions of the ZE21B alloy (Fig. 9e)4.
Anti-fouling
Anti-fouling function of the stent coating can alleviate the adsorption of platelets and other cells, which is important in the reduction of restenosis and thrombosis. After stent implantation, when blood flow changes and endothelial injuries occur, platelets and other cells that are mostly negatively charged are easily deposited onto positively charged metal stent, leading to restenosis and thrombosis of the vascular. LbL technology can bind anti-fouling polymer, hydrophilic polymer and negatively charged polymer on the stent to improve anti-fouling effect.
Polymers such as PSS have been widely applied in anti-fouling coatings due to their excellent characteristics, such as low surface free energy, low elastic modulus, and low surface roughness84. The anti-fouling polymers can be fixed on the surface of stent by LbL method, and the anti-fouling purpose can be achieved through mutual repulsion of negative charges. Yang et al. prepared a coating on SUS316L SS substrate by electrochemically copolymerizing poly 3,4-ethylenedioxythiophene (PEDOT) (to increase the solubility of PSS) with GO, PSS and heparin. The negative charges of GO, PSS and heparin repel negatively charged proteins and platelets to achieve the purpose of anti-fouling and anti-coagulation (Fig. 10a, b)85.
a Electrochemically copolymerizing positive charges of PEDOT with negative charges of GO, PSS and heparin. b SEM images of human platelets adherent to (i) SUS316L, (ii) PEDOT/ heparin, (iii) PEDOT/PSS, (iv) PEDOT/GO, and (v) PEDOT/GO/ heparin substrates85. Copyright © 2019 MDPI. c The surface modification process: the deposition of thin Au layers, the chemisorption of disulfides, and the coupling of PEG derivatives or heparin by disulfides. d AFM images of the modified surfaces. (i) Au, (ii) Au-S-PEG-SO3, (iii) Au-S-PEG- heparin; RMS roughness:(i) 2.231, (ii) 1.070, (iii) 1.129 nm19. Copyright ©2002 Taylor & Francis.
Surface modification by hydrophilic polymers can weaken the adhesion of proteins, platelets/cells on stent surface86,87,88,89,90,91. PEG has the excluded volume on the surface and the flexible hydrophilic chain which motions to expel proteins/cells. Importantly, it is non-toxicity and non-immunogenecity86,89,92. Sulfonated PEG (PEG-SO3) grafted polyurethane shows enhanced blood compatibility and biostability than PEG alone because of the anti-coagulant active of sulfonate groups93. Lee et al. studied a surface modification method of metallic via a self-assembly technique including the deposition of thin Au layers, the chemisorption of disulfides, and the coupling of PEG derivatives or heparin by disulfides (Fig. 10c). The surface modified with sulfonated PEG or heparinized PEG showed decreased static contact angles, increased hydrophilicity, enhanced blood compatibility and decreased VSMCs adhesion. The images of the modified surfaces revealed that the modified gold surfaces became even smoother than the control (Au) surface (Fig. 10d)19.
Anti-proliferation
Restenosis is a serious complication after stent implantation. After the vascular injury during stent implantation, the accumulated leukocytes and platelets lead to acute inflammatory response and endothelial dysfunction, which will lead to excessive proliferation of VSMCs94. The extracellular matrix (ECM) produced by VSMCs induces thickening of the vessel wall, which leads to neointimal hyperplasia and restenosis95,96. Anti-proliferative drugs were coated on the surface of DES by chemical polymer to prevent restenosis as local treatment intervention. However, there were some problems at the chemical polymer, such as easy to deformation and shedding, poor biocompatibility which result in poor endothelialization and thrombosis. With the wide application of natural biopolymer to make up chemical polymer, there is an urgent problem to be solved, it is difficult to load hydrophobic anti-proliferative drugs in the hydrophilic biopolymer layer to achieve long-term sustained releasing. Self-assembly technology provides a new route for directly attaching and releasing therapeutic molecules from the metal surface without polymers, it can also assemble anti-proliferative drugs and biopolymers to the surface of DES through LbL method to solve this problem.
At present, the main method of ant-proliferation is to load immunosuppressant drugs on the surface of DES, such as paclitaxel, sirolimus and its derivatives including everolimus and otarolimus. Paclitaxel binds β-tubulin dimers and inhibits their depolymerization to stabilize the assembly of microtubules97,98. Low doses of paclitaxel cause cell-cycle arrest in the G1 phase without causing cellular apoptosis (Fig. 11b)99. This results in a cytostatic response with inhibiting VSMC proliferation and migration, this is the key processes of inhibiting neointimal hyperplasia during in-stent restenosis100. Kim et al. conjugated heparin with poly-dopamine, then self-assembled a paclitaxel eluting multilayer composed of heparin, anionic hyaluronic acid-g-PLGA micelles, and PLL on the metal surface via LbL method. The coating could easily control the paclitaxel loading amount on the metal surface and realize the continuous release profiles of paclitaxel over an extended period (Fig. 11a). The multilayer coating successfully arrested the proliferation of human coronary artery VSMC101, and the biocompatibility was also improved. Sirolimus is a macrolide that inhibits the mammalian target, also causes cells to be arrested in the G1 phase102,103. Shen et al. designed an asymmetrical stent system. LbL chitosan/heparin complex film was loaded on the luminal side of stent, and sirolimus was coated by PLLA on the abluminal side. In comparison to traditional circumferentially coated ones, this kind of DES system in the porcine model not only inhibited the proliferation of intimal (Figure 11ci), but also promoted the endothelialization of lumen vessels surrounding the stent (Figure 11cii)104. The above drugs are effective in ant-proliferation, however, they can’t solve the upstream oxidative stress which triggers the restenosis cascade. Therefore, the final patient mortality rates about DES are similar to the BMS105.
a Paclitaxel eluting multilayer composed of heparin, paclitaxel loaded anionic hyaluronic acid-g-PLGA micelles, and PLL on the metal surface via LbL fashion. b Causing cell-cycle arrest in the G1 phase without causing cellular apoptosis by low doses of paclitaxel. c At 7, 14 and 28 days: (i) Histopathology and histomorphometry analysis follow-up. During the entire observation, percentage area of stenosis (%AS) gradually increased while LA decreased in all three groups. At 7 and 14 days, BMS and chtosan/heparin (C/H) LbL-SES were almost the same in measurements of lumen area (LA) and %AS. However, at the 28 days follow-up, LA of C/H LbL-SES was significantly lager, while %AS was significantly lower compared with BMS. At 28 days follow-up, there was no difference between C/H LbL-SES and traditionally circumferential sirolimus-eluting stents (SES) in LA and %AS. BMS suffered the greatest %AS in all three groups at 28 days. LA = lumen area; %AS = percentage of area stenosis (ii) Scanning-electron microscopic follow-up. At 7 days, the endothelium cover on C/H LbL-SES was relatively intact, and regularly arranged spindle-shaped endothelial-like cells could be found. At 14 days, the re-endothelialization process was almost complete in BMS and C/H LbL-SES. At 28 days, the neointima of BMS was somewhat hyperplastic, while endothelial repair in SES still remained poor104. Copyright © 2012 Springer.
Amphiphilic macromolecules, comprised of a branched sugar-based hydrophobic segment and a hydrophilic PEG tail, were of great interest because of its non-toxic treatment of restenosis. Different from paclitaxel and sirolimus, amphiphilic macromolecules can reduce proliferation through competitive inhibition of the receptor-mediated uptake of oxidized low-density lipoprotein (oxLDL)106. Amphiphilic macromolecules can mimic key characteristics of oxidized lipids and target VSMC scavenger receptors107,108. Thus, the possibility of excessive oxLDL induced endothelial proliferation is limited. Amphiphilic macromolecules showed superior cytocompatibility, and good potential in avoiding locally toxic and strong immune response of DES109,110. It should be noted that amphiphilic macromolecules exhibit a concentration-dependent efficacy106, and the concentration of the macromolecules in the coating must be sufficient to achieve the therapeutic effect. Chan et al. designed a macromolecular monolayer via self-assembly, which could afford controllable release of amphiphilic macromolecules to reach the therapeutic effect. While, although the restenosis cascade is mainly driven by VSMC hyperproliferation, it also involves other cell types25.
Anti-thrombogenicity
The main causes of late thrombosis by DES are analyzed as follows. The loaded cytotoxic drugs affected the healing of vascular endothelium111,112; The polymer coating used to load drugs leads to hypereosinophilia, vascular inflammation and thrombosis; The thicker the thickness of the stent coating, the easier to cause thrombosis in vascular113. In order to reduce the risk of thrombosis, the self-assembled cardiovascular stent coating was prepared with thinner thickness and capability of non-polymer-based drug loading. It was modified with poly-dopamine as an intermediate layer to improve its biocompatibility, so that a large amount of biopolymers could be bonded to the coating to prevent thrombus114,115. Among the biopolymers, it was effective to bind active molecules to prevent late thrombosis, such as heparin and NO.
Heparin, one of the major glycoproteins in endothelial glycocalyx, is an anti-coagulant, which can also inhibit migration and proliferation of VSMCs116. The anti-coagulant activity of heparin is achieved mainly by catalyzing the combination of antithrombin III and thrombin117. Lee et al. prepared a 3D printed PLA biodegradable polymeric stent coating with polydopamine, polyethylenimine (PEI) and heparin to prevent thrombosis and restenosis with anti-coagulation property and good blood compatibility (Fig. 12a). They established porcine ex vivo arteriovenous shunt models with PLA, PLADP, and PLADPH, respectively (Fig. 12b). From ex vivo analysis, a large number of platelets were adhered on the PLA and PLADP stent surfaces, but very minimal platelet deposition was observed on PLADPH surfaces (Fig. 12c). They used poly-dopamine and PEI as intermediates to perform surface modification, so as to bond a large amount of heparin, because the carboxyl groups of heparin can react with amino groups like PEI to further cross-link8,118. It should be noticed that heparin treatment can cause thrombocytopenia, which is associated with platelet activation and aggregation67.
a Schematic illustration of preparation of heparinized 3D printed biodegradable PLA stent. (i) 3D printed bare PLA stent, (ii) poly-dopamine coating on bare PLA stent, (iii) PEI immobilization on poly-dopamine coated PLA stent, (iv) heparin grafting on poly-dopamine/PEI layered PLA stent, (v) and visualization of PLADP and PLADPH (poly-dopamine + PEI + heparin) after alcian blue staining of glycosaminoglycans within the heparin. b Ex vivo arteriovenous shunt blood circulation system using porcine animal model. c Neon photograph images for platelet visualization on PLA, PLADP, and PLADPH (n = 3)8. Copyright © 2019 Elsevier. d The coating combines the functions of NO and heparin for improved inhibition of thrombogenic responses (coagulation cascade and platelets) and inhibition of SMC proliferation, thereby reducing the risk of thrombosis and stenosis of the stent67. Copyright © 2021 Elsevier.
NO may be produced by EC to achieve thrombotic homeostasis by preventing platelet activation119. The mechanism to inhibit platelet activity of NO is complex. A main approach is to activate the soluble guanylate cyclase120,121. In addition, NO can anti-platelet activity by inhibiting thromboxane receptor on platelet membranes and can relax the surrounding smooth muscle to increase blood flow122,123. Furthermore, NO can suppress VSMC proliferation and stimulate EC migration96,124. It should be noted that NO inhibitory effect on platelet function is highly dose-dependent, beyond the normal range of NO is related to adverse outcomes and cytotoxicity in the vascular system (Fig. 12d)124. Stenting process inevitably damaged EC, accompanied by impaired endothelial nitric oxide synthase activity and insufficient NO production125. Glycocalyx heparin sulfate, an analog of heparin and the most prominent component on the EC surface, can increase the activity of endothelial nitric oxide synthase126,127. As a result, vascular stents with heparin sulfate-like and NO-generating properties have synergistically enhanced EC functions. However, some problems occurred in these cardiovascular stent coatings in previous studies94,128,129,130,131,132,133, such as the in-sufficient amount of integrated heparin128, uncontrolled NO releasing dose, excessive coating thickness and so on134. Ma et al. designed an amine-bearing coating pAMDA (prepared by polyamine and poly-dopamine) to tailor endothelium-mimicking functionalities. The pAMDA coating was formed by pretreatment with poly-dopamine, followed by surface chemical cross-link with polyamine. The pAMDA coating had a universal and strong adhesive property of catechol-amine coatings, and contained a large number of amino groups from polyamine by which the coating could covalent graft stable Cu-DOTA coordination complex to catalyze the release of NO at a physiological rate, and could bond with enough amount of heparin to effectively inhibit blood coagulation and VSMC proliferation. The high chemical stability of both the Cu-DOTA complex and pAMDA coating imparted the stents with high catalytic activity of NO and heparin bioactivity retention after application for 1 month, and improved anti-restenosis, anti-thrombogenicity, and re-endothelialization of the coating67.
Endothelialization
A crucial factor of ISR and stent thrombosis is lack of a functional endothelial layer after vascular injury135,136,137, so rapid re-endothelialization on the stent surface could reduce thrombus12,136,138. However DES induces nonspecific anti-proliferative effects not only on VSMCs, but also on vascular EC. By LbL method, pro-cellular biopolymers such as endothelial ECM components collagen and natural polymer like chitosan can be loaded on DES to promote endothelialization (Table 2). Furthermore, LbL provides a simple route to load and control release of active molecules such as VEGF to increase the adhesion of EC.
Collagen, as the dominant component in the ECM. A protein sequence derived from hCOLIII provides potent cell adhesion activity139. However, collagen is prone to thrombosis which hinder its application in DES. Yang et al. prepared a new recombinant hCOLIII, which does not present platelets’ binding sites while retaining the cell adhesion activity. They formed an ECM-mimetic multilayer coating together with hyaluronic acid and hCOLIII on the substrate by LbL fashion, which was prepared via the adhesion of poly-dopamine/PEI and the electrostatic interaction between hCOLIII and hyaluronic acid (Fig. 7e). The hCOLIII-based ECM-mimetic coating showed excellent blood compatibility and prominent thrombo-protective property, and the coating promoted the proliferation of EC140.
VEGF can promote the adhesion, proliferation, differentiation, and migration of EC62,141. VEGF is also important in inducing the mobilization, homing, and differentiation of endothelial progenitor cells. After vascular injury, endothelial progenitor cells are mobilized into the blood flow and home to the lesion site to participate in endothelium regeneration142,143. In addition, because of the short half-life, a relatively high concentration of VEGF is necessarily needed. However, the high dosage will lead to severe side effects, like the vascularization in non-targeted, the fast growth of some occult tumors144. Liu et al. prepared a VEGF-loaded heparin/PLL particle, and immobilized it on poly-dopamine coated Ti surface (Fig. 13a). Surface-modified VEGF-loaded particles significantly inhibited platelets activation and adhesion, and were effective in the proliferation and survival of both ECs and endothelial progenitor cells, and the particles could realize control release of VEGF at a long-term (Fig. 13b)145.
a VEGF-loaded heparin/PLL particle. b Migration assay of ECs from dopamine coated surface to Ti-DM, Ti-DM-non-VEGF-loaded particles, and Ti-DM-VEGF-loaded particles surfaces: rhodamine fluorescence staining result. The migration distance was calculated from at least nine images145. Copyright © 2014 Wiley. c The opposite charges of chitosan/heparin LbL coated coronary stent, promoting intimal healing and re-endothelialization. d Typical SEM images (500, insert for 200) of the inner wall of the stented porcine arteries after stent implantation for 1 week, 2 and 4 weeks, respectively12. Copyright © 2009 Elsevier.
Chitosan has good cellular attachment, excellent biocompatibility, and capability of immobilizing biological components146; while heparin is an anti-coagulant reagent used in clinical. Meng et al. prepared a chitosan/heparin coated coronary stent by LBL for their opposite charges. This coating showed good hemocompatibility, and was efficient in promoting intimal healing and re-endothelialization after stent implantation (Fig. 13c, d). In addition, the chitosan/heparin LbL modification is relatively facile and inexpensive, and is more stable during sterilization and storage12.
Targeted gene therapy
The gene eluting stents are currently under development in order to solve the problems about DES like the delayed endothelization which leads to late thrombosis, drug toxicity, and poor polymer biocompatibility147,148. At present, gene delivery vectors include viral vectors, naked plasmids, and non-viral nano-delivery systems149,150,151. While there are some troublesome problems including strong inflammatory reactions, high cytotoxicity, low efficiency in vivo gene transfer, and the potential risk of viral DNA integration to the host’s genom152. The LbL method can load genes on the surface of stent through electrochemical coupling, multilayer electrostatic adsorption charged nanoparticles to achieve controllable releasing of gene, and adhesion biopolymer coatings by poly-dopamine to reduce toxic side effects (Fig. 14a). Self-assembled coating is not only simple to manufacture, but also improves the biocompatibility of coating.
a The preparation of gene eluting stents, phosphorylcholine base coating loading with miRNA126, immobilizing miRNA 145/ssPEI nanoparticles on the hyaluronic acid-coated stent, and constructing the (protamine sulfate/shRNA-pDNA) film152,155,165 b Increasing VEGF and fibroblast growth factor (FGF) to achieve the intelligent self-repair of vascular ECs at the transcriptional level by miRNA126. c Reducing the downstream protein c-Myc by the effective knock-down of the miRNA 145, which retarded the undesired growth of VSMCs near the stents. d Measurement of neointima by hematoxylin & eosin (H&E) staining. The white rabbit iliac arteries were harvested 4 weeks after stent implantation, The panel shows representative arteries from the BMS hyaluronic acid-coated stent, and miRNA 145/ssPEI nanoparticles /hyaluronic acid-immobilized stent groups152. Copyright © 2016 The Korean Society of Cardiology. e PDNA vector with encoding shRNA to target and block TGF-β1 expression. f Histological analysis results at 28 days. (i), (ii): Typical optical photographs of the H&E-stained cross section slices of the rabbit femoral arteries with shRNA-pDNA stents. The scale bar of (i) represents 1 mm. The scale bar of (ii) represents 200 mm. (iii), (iv), (v): (iii)Histological analysis of neointimal thickness, (iv) I/M ratio, (v) the percentage of neointimal stenosis (*P < 0.05)166. Copyright © 2016 Elsevier.
MicroRNAs (miRNAs) mediate messenger RNA silencing through translational repression or degradation after complementary base pairing153. While vascular injury, miRNAs are involved in inflammatory cell recruitment and activation, and dedifferentiation of VSMC, which is the key process driving the vessel response to injury154. MiRNA126 is a specific EC miRNA, it can achieve the intelligent self-repair of vascular ECs at the transcriptional level. MiRNA126 inhibits the expression of Spred-1 to increase VEGF and fibroblast growth factor. In addition, miRNA126 inhibits the expression of vascular cell adhesion molecule-1, reduces the adhesion of inflammatory cell, which is the initiating factors of proliferation of VSMC (Fig. 14b)155. Choline phosphate is a major component of the outer phospholipid molecules of the cell membrane, and it is electrically neutral, which avoids the activation of intrinsic pathway. By surface modification, the biomimetic phosphoric acid is easy to be coupled with the biological macromolecule gene and drugs155. As the slight alkalinity of miRNA126 and the slight acidity of 10% phosphorylcholine solution, Wang et al. prepared a phosphorylcholine base coating loading with miRNA126 by the chemical coupling method easily (Fig. 14b). The miRNA126 loaded bionic micro/nano structured coating coronary stent has a positive significance in the percutaneous coronary intervention of coronary heart disease9. MiRNA 145 is known to be responsible for VSMC proliferation (Fig. 14c). As ssPEI has high branch transfection efficiency as so as viral vectors, Che et al. conjugated dopamine and hyaluronic acid on the stent surface and immobilized miRNA 145/ssPEI nanoparticles on the hyaluronic acid-coated stent to develop an effective and safe gene-eluting system in the treatment of restenosis. Hyaluronic acid enhanced the proliferation and migration of EC156, and miRNA 145 could knock down the initial over-growth of VSMCs near the implanted stent (Fig. 14d)152,157. Small interfering RNA (siRNA) can be used for sequence-specific gene silencing in vascular cells through degrading disease-causing proteins by acting on miRNA. To deliver siRNAs to the vessel wall, the negatively charged siRNA was incorporated into cationic polymers including PEI, PLL, chitosan etc., which were stabilized through Coulomb interactions158,159,160,161. The formation of nanoplexes allowed for subsequent endocytosis into cells. To ensure their stabilization on the stent and controllable release of nanoplexes, Hossfeld, et al. prepared a bioactive stent coating based on hyaluronic acid and chitosan with incorporated chitosan-siRNA nanoplexes by the LbL method, as a new application against ISR162.
The cytokine transforming growth factor-β1 (TGF-β1) is important in myofibroblasts behaviors and restenosis. TGF-β1 influences all aspects to ISR, including inflammatory cell infiltration, transdifferentiation of myofibroblasts, myofibroblasts migration and proliferation, and ECM production (Fig. 14e)163,164. Therefore, the down-regulation of TGF-β1 could be a potential treatment of ISR. In a recent study, a surface-mediated gene delivery system, which involved a plasmid DNA (pDNA) vector with encoding shRNA to target and block TGF-β1 expression (TGF-β1-shRNA-pDNA), was constructed of the positively charged protamine sulfate and the negatively charged pDNA via LbL method. Plasmid DNA is more stable than shRNA and allows long-term treatment effect, and the gene delivery effect could be site-specific165. In vivo animal experiments were conducted using a rabbit femoral artery injury model. The results showed that the (protamine sulfate/shRNA-pDNA) film successfully inhibited the secretion of fibronectin and collagen type I and reduced the proliferation of fibroblasts. Also, the film locally reduced the secretion of ECM protein and inhibited neointimal hyperplasia (Fig. 14f). Such a strategy of inhibiting TGF-β1-associated adverse cellular processes is different from DES and the simple re-endothelialization strategy, and may have great potential for designing new anti-restenosis vascular stents166.
Conclusions and perspectives
Self-assembled functional coatings can effectively improve the performance and function of stents, alleviating the problems of restenosis, thrombosis and anaphylaxis of cardiovascular stents. In this review, we introduce the functional coating molecules, self-assembly methods, functions and applications of self-assembled coatings in detail. For self-assembled coatings, polymer-free coatings can be formed to avoid the use of polymers, which can solve the problems such as restenosis caused by polymer coatings. In addition, self-assembly can effectively improve biocompatibility and stability of coatings by using biomolecules to replace chemical polymer. The encouraging achievements by the self-assembled coated stents can include corrosion resistance, anti-fouling, anti-diffusion, anti-thrombogenicity, endothelialization, and targeted gene therapy. Although stents based on self-assembled coatings have many advantages, advancement of this unique technique is still needed for further improvement of stent coatings. We have the following outlook for its future development:
-
(1)
First, the practical application of stents based on self-assembled coatings should be increased, and more degradable stents based on self-assembled coatings should be developed (Fig. 15a). The current clinical application of DES mainly uses polymer coatings for drug loading167, which has some potential problems. Coatings based on self-assembly are mainly in the experimental stage and, currently have not found practical clinical applications. At the same time, most of them are applied to non-degradable metal stents. Therefore, on the one hand, the clinical application of stents based on self-assembled coatings should be gradually realized. On the other hand, as the next-generation of stents, degradable stents with self-assembled coatings should better reduce thrombosis and restenosis with combined features.
Fig. 15: Perspectives of cardiovascular stents based on self-assembled coatings for future development applications. a New assembly method. The combination of multiple self-assembly modalities allows the fabrication of multi-layer self-assemblies with excellent functions. b New materials. The good deformation ability of new materials such as hydrogel and graphene oxide is utilized to make the stent and coating adjust to the pressure of the vessel wall, so that the stent can better fit the vessel wall. c New treatment. New drugs such as nanodrugs and miRNAs are assembled on the coating to increase cellular metabolism or release biologically active proteins through stably release into the cell. d Low cost and high security. After three-dimensional imaging of diseased blood vessels, 3D printing technology are used to create stents with appropriate shape to avoid damage to the endothelial cells of the diseased vessels.
-
(2)
Second, the types of coating materials used in self-assembly coatings can be increased, such as GO with large specific surface area, good mechanical properties and biocompatibility, artificial or biological modified hydrogels and collagen (Fig. 15b). Therefore, the stents can be endowed with better biocompatibility, anti-thrombotic ability, and anti-restenosis ability. At the same time, it is also important to develop smarter coatings using self-assembly techniques, so that therapeutic benefits can be maximized with the smallest drug dose and minimal side effects. For instance, the firehawk as stent a novel DES with unique design with recessed abluminal grooves have demonstrated minimal volume and antiproliferative drug usage to reduce inflammation and hypersensitive reaction.168
-
(3)
Furthermore, novel treatment modalities based on self-assembled coatings can be explored further (Fig. 15c). First, it is meaningful to explore the combination of self-assembled coatings with a range of drugs, such as specific antibodies, peptides, nucleic acids, and nanomedicines. Second, drugs in use can be modified to enhance and extend their properties through genetic engineering, bioengineering and nanotechnology. In addition to the previously mentioned mimicking of mussel adhesion, more biomimetic coatings can be fabricated using self-assembly techniques. For example, a biofilm bilayer-like microstructure can be formed on the stents surface, which can reduce protein adsorption and cell attachment, and improve the blood compatibility of the stents25,169,170. Self-assembly techniques can be used to create a more realistic vascular environment on the stent surface to reduce restenosis and thrombosis.
-
(4)
Finally, evolution of advanced stents and coatings that are safer, cheaper, and simpler to manufacture are expected (Fig. 15d). As an emerging manufacturing approach, 3D printing technology can be combined to design and manufacture new cardiovascular stents, or shape memory materials such as poly (propylene carbonate) and poly(ε-caprolactone) can be used to achieve independent expansion and contraction of stents with temperature changes. Using these technologies and materials can effectively improve the safety of stents and coatings, reduce their prices and make them easier to be manufactured.
References
He, Y. et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol. 7, 540–548 (2019).
Lv, J. et al. Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J. Am. Coll. Cardiol. 69, 1116–1125 (2017).
Qi, P., Yang, Y., Maitz, F. M. & Huang, N. Current status of research and application in vascular stents. Chin. Sci. Bull. 58, 4362–4370 (2013).
Zhang, Z. Q., Yang, Y. X., Li, J. A., Zeng, R. C. & Guan, S. K. Advances in coatings on magnesium alloys for cardiovascular stents - A review. Bioact. Mater. 6, 4729–4757 (2021).
Nakazawa, G. et al. The Pathology of Neoatherosclerosis in Human Coronary Implants: Bare-Metal and Drug-Eluting Stents. J. Am. Coll. Cardiol. 57, 1314–1322 (2011).
Fischman, D. L. et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N. Engl. J. Med. 331, 496–501 (1994).
Hou, L.-D. et al. A review on biodegradable materials for cardiovascular stent application. Front. Mater. Sci. 10, 238–259 (2016).
Lee, S. J. et al. Heparin coating on 3D printed poly (l-lactic acid) biodegradable cardiovascular stent via mild surface modification approach for coronary artery implantation. Chem. Eng. J. 378, 122116 (2019).
Wang, J. et al. Preparation of the micro/nano structures of the biomimetic coating stent for loading MiRNA126 by four-beam laser interference. Optik 128, 247–252 (2017).
Fischell, D. R., Fischell, T. A., Fischell, R. E., Tepe, G. & Wiskirchen, J. Radioisotope stents. Minim. Invasive Ther. Allied Technol. 11, 149–155 (2002).
Meng, S. et al. The effect of a layer-by-layer chitosan-heparin coating on the endothelialization and coagulation properties of a coronary stent system. Biomaterials 30, 2276–2283 (2009).
Qiu, X. et al. Cellular remodeling of fibrotic conduit as vascular graft. Biomaterials 268, 120565 (2021).
Chen, J. L., Li, Q. L., Chen, J. Y., Chen, C. & Huang, N. Improving blood-compatibility of titanium by coating collagen-heparin multilayers. Appl. Surf. Sci. 255, 6894–6900 (2009).
Park, J. et al. Interface Engineering of Fully Metallic Stents Enabling Controllable H2O2 Generation for Antirestenosis. Langmuir 35, 3634–3642 (2019).
Lin, Q. K. et al. Heparin/collagen multilayer as a thromboresistant and endothelial favorable coating for intravascular stent. J. Biomed. Mater. Res., Part A 96A, 132–141 (2011).
Kim, T. G., Lee, H., Jang, Y. & Park, T. G. Controlled Release of Paclitaxel from Heparinized Metal Stent Fabricated by Layer-by-Layer Assembly of Polylysine and Hyaluronic Acid-g-Poly(lactic-co-glycolic acid) Micelles Encapsulating Paclitaxel. Biomacromolecules 10, 1532–1539 (2009).
Lamichhane, S., Gallo, A. & Mani, G. A Polymer-Free Paclitaxel Eluting Coronary Stent: Effects of Solvents, Drug Concentrations and Coating Methods. Ann. Biomed. Eng. 42, 1170–1184 (2014).
Alkekhia, D., Hammond, P. T. & Shukla, A. Layer-by-Layer Biomaterials for Drug Delivery. Annu. Rev. Biomed. Eng. 22, 1–24 (2020).
Lee, H. J. et al. Improved blood compatibility and decreased VSMC proliferation of surface-modified metal grafted with sulfonated PEG or heparin. J. Biomater. Sci., Polym. Ed. 13, 939–952 (2002).
Boissezon, R., Muller, J., Beaugeard, V., Monge, S. & Robin, J.-J. Organophosphonates as anchoring agents onto metal oxide-based materials: synthesis and applications. Rsc Adv. 4, 35690–35707 (2014).
Raman, A., Dubey, M., Gouzman, I. & Gawalt, E. S. Formation of self-assembled monolayers of alkylphosphonic acid on the native oxide surface of SS316L. Langmuir 22, 6469–6472 (2006).
Raman, A. & Gawalt, E. S. Self-assembled monolayers of alkanoic acids on the native oxide surface of SS316L by solution deposition. Langmuir 23, 2284–2288 (2007).
Tosatti, S., Michel, R., Textor, M. & Spencer, N. D. Self-assembled monolayers of dodecyl and hydroxy-dodecyl phosphates on both smooth and rough titanium and titanium oxide surfaces. Langmuir 18, 3537–3548 (2002).
Slaney, A. M. et al. Biocompatible Carbohydrate-Functionalized Stainless Steel Surfaces: A New Method For Passivating Biomedical Implants. ACS Appl. Mater. Interfaces 3, 1601–1612 (2011).
Chan, J. W., Zhang, Y. Y. & Uhrich, K. E. Amphiphilic Macromolecule Self-Assembled Mono layers Suppress Smooth Muscle Cell Proliferation. Bioconjugate Chem. 26, 1359–1369 (2015).
Kang, S. M. et al. One-Step Multipurpose Surface Functionalization by Adhesive Catecholamine. Adv. Funct. Mater. 22, 2949–2955 (2012).
Wang, J.-L. et al. Facile fabrication of robust superhydrophobic multilayered film based on bioinspired poly(dopamine)-modified carbon nanotubes. Phys. Chem. Chem. Phys. 16, 2936–2943 (2014).
Chien, C.-Y. & Tsai, W.-B. Poly(dopamine)-Assisted Immobilization of Arg-Gly-Asp Peptides, Hydroxyapatite, and Bone Morphogenic Protein-2 on Titanium to Improve the Osteogenesis of Bone Marrow Stem Cells. ACS Appl. Mater. Interfaces 5, 6975–6983 (2013).
Yang, Z. L. et al. Mussel-inspired catalytic selenocystamine-dopamine coatings for long-term generation of therapeutic gas on cardiovascular stents. Biomaterials 178, 1–10 (2018).
Wei, Q., Zhang, F., Li, J., Li, B. & Zhao, C. Oxidant-induced dopamine polymerization for multifunctional coatings. Polym. Chem. 1, 1430–1433 (2010).
Wang, J. L. et al. Electropolymerization of dopamine for surface modification of complex-shaped cardiovascular stents. Biomaterials 35, 7679–7689 (2014).
Reilly, C. F., Fritze, L. M. & Rosenberg, R. D. Heparin inhibition of smooth muscle cell proliferation: a cellular site of action. J. Cell. Physiol. 129, 11–19 (1986).
Koster, A. et al. Hemostatic activation and inflammatory response during cardiopulmonary bypass - Impact of heparin management. Anesthesiology 97, 837–841 (2002).
Linhardt, R. J. 2003 Claude S. Hudson Award address in carbohydrate chemistry. Heparin: Structure and activity. J. Med. Chem. 46, 2551–2564 (2003).
Grant, G. G. S., Koktysh, D. S., Yun, B. G., Matts, R. L. & Kotov, N. A. Layer-By-Layer Assembly of Collagen Thin Films: Controlled Thickness and Biocompatibility. Biomed. Microdevices 3, 301–306 (2001).
Fu, J., Ji, J., Fan, D. & Shen, J. Construction of antibacterial multilayer films containing nanosilver via layer-by-layer assembly of heparin and chitosan-silver ions complex. J. Biomed. Mater. Res., Part A 79A, 665–674 (2006).
Hisham, F., Maziati Akmal, M. H., Ahmad, F., Ahmad, K. & Samat, N. Biopolymer chitosan: Potential sources, extraction methods, and emerging applications. Ain Shams Eng. J. 15, 102424 (2024).
Chen, W. L., Habraken, T. C. J., Hennink, W. E. & Kok, R. J. Polymer-Free Drug-Eluting Stents: An Overview of Coating Strategies and Comparison with Polymer-Coated Drug-Eluting Stents. Bioconjugate Chem. 26, 1277–1288 (2015).
Song, D., Hsu, L. F. & Au, J. L. S. Binding of taxol to plastic and glass containers and protein under in vitro conditions. J. Pharm. Sci. 85, 29–31 (1996).
Lee, B. H. et al. Paclitaxel-coated expanded polytetrafluoroethylene haemodialysis grafts inhibit neointimal hyperplasia in porcine model of graft stenosis. Nephrol., Dial., Transplant. 21, 2432–2438 (2006).
Mani, G. et al. Delivery of paclitaxel from cobalt-chromium alloy surfaces without polymeric carriers. Biomaterials 31, 5372–5384 (2010).
Belu, A., Mahoney, C. & Wormuth, K. Chemical imaging of drug eluting coatings: Combining surface analysis and confocal Raman microscopy. J. Controlled Release 126, 111–121 (2008).
Levy, Y., Khan, W., Farah, S. & Domb, A. J. Surface Crystallization of Rapamycin on Stents Using a Temperature Induced Process. Langmuir 28, 6207–6210 (2012).
Farah, S., Khan, W. & Domb, A. J. Crystalline coating of rapamycin onto a stent: Process development and characterization. Int. J. Pharm. 445, 20–28 (2013).
Iakovou, I. et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA-J. Am. Med. Assoc. 293, 2126–2130 (2005).
Virmani, R., Farb, A., Guagliumi, G. & Kolodgie, F. D. Drug-eluting stents: caution and concerns for long-term outcome. Coron. Artery Dis. 15, 313–318 (2004).
Virmani, R. et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent should we be cautious? Circulation 109, 701–705 (2004).
Virmani, R., Kolodgie, F. D. & Farb, A. Drug-eluting stents: are they really safe? Am. heart hospital J. 2, 85–88 (2004).
Nebeker, J. R. et al. Hypersensitivity cases associated with drug-eluting coronary stents - A review of available cases from the research on adverse drug events and reports (RADAR) project. J. Am. Coll. Cardiol. 47, 175–181 (2006).
Ong, A. T. L. et al. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. J. Am. Coll. Cardiol. 45, 2088–2092 (2005).
Chan, J. W., Huang, A. & Uhrich, K. E. Self-Assembled Amphiphilic Macromolecule Coatings: Comparison of Grafting-From and Grafting-To Approaches for Bioactive Delivery. Langmuir 32, 5038–5047 (2016).
Ulman, A. Formation and structure of self-assembled monolayers. Chem. Rev. 96, 1533–1554 (1996).
Mani, G. et al. Drug delivery from gold and titanium surfaces using self-assembled monolayers. Biomaterials 29, 4561–4573 (2008).
Mani, G., Chandrasekar, B., Feldman, M. D., Patel, D. & Agrawal, C. M. Interaction of Endothelial Cells with Self-Assembled Monolayers for Potential Use in Drug-Eluting Coronary Stents. J. Biomed. Mater. Res., Part B 90B, 789–801 (2009).
Ruan, C. M., Bayer, T., Meth, S. & Sukenik, C. N. Creation and characterization of n-alkylthiol and n-alkylamine self-assembled monolayers on 316L stainless steel. Thin Solid Films 419, 95–104 (2002).
Mahapatro, A. et al. The use of alkanethiol self-assembled monolayers on 316L stainless steel for coronary artery stent nanomedicine applications: an oxidative and in vitro stability study. Nanomed. -Nanotechnol. Biol. Med. 2, 182–190 (2006).
Mahapatro, A. et al. Drug delivery from therapeutic self-assembled monolayers (T-SAMs) on 316L stainless steel. Curr. Trends Med. Chem. 8, 281–289 (2008).
Decher, G. & Hong, J. D. Buildup of ultrathin multilayer films by a self-assembly process, 1 consecutive adsorption of anionic and cationic bipolar amphiphiles on charged surfaces. Makromol. Chem.-Macromol. Symposia 46, 321–327 (1991).
Decher, G. & Hong, J. D. buildup of ultrathin multilayer films by a self-assembly process.2. consecutive adsorption of anionic and cationic bipolar amphiphiles and polyelectrolytes on charged surfaces. Ber. Bunsen-Ges. Phys. Chem. Chem. Phys. 95, 1430–1434 (1991).
Tang, Z. Y., Wang, Y., Podsiadlo, P. & Kotov, N. A. Biomedical applications of layer-by-layer assembly: From biomimetics to tissue engineering. Adv. Mater. 18, 3203–3224 (2006).
Picart, C. Polyelectrolyte multilayer films: From physico-chemical properties to the control of cellular processes. Curr. Med. Chem. 15, 685–697 (2008).
Yang, L. et al. A tailored extracellular matrix (ECM)-Mimetic coating for cardiovascular stents by stepwise assembly of hyaluronic acid and recombinant human type III collagen. Biomaterials 276, 121055 (2021).
Hong, S. et al. Non-covalent self-assembly and covalent polymerization co-contribute to polydopamine formation. Adv. Funct. Mater. 22, 4711–4717 (2012).
Lee, H., Dellatore, S. M., Miller, W. M. & Messersmith, P. B. Mussel-inspired surface chemistry for multifunctional coatings. Science 318, 426–430 (2007).
Fan, Y. H. et al. Immobilization of nano Cu-MOFs with polydopamine coating for adaptable gasotransmitter generation and copper ion delivery on cardiovascular stents. Biomaterials 204, 36–45 (2019).
Tan, J. Y. et al. Heparin/poly-l-lysine nanoplatform with growth factor delivery for surface modification of cardiovascular stents: The influence of vascular endothelial growth factor loading. J. Biomed. Mater. Res.,Part A 108, 1295–1304 (2020).
Ma, Q. et al. Durable endothelium-mimicking coating for surface bioengineering cardiovascular stents. Bioact. Mater. 6, 4786–4800 (2021).
Gu, X. N., **e, X. H., Li, N., Zheng, Y. F. & Qin, L. In vitro and in vivo studies on a Mg–Sr binary alloy system developed as a new kind of biodegradable metal. Acta Biomater. 8, 2360–2374 (2012).
Tang, H. et al. A surface-eroding poly(1,3-trimethylene carbonate) coating for magnesium based cardiovascular stents with stable drug release and improved corrosion resistance. Bioact. Mater. 7, 144–153 (2022).
Boodagh, P., Guo, D. J., Nagiah, N. & Tan, W. Evaluation of electrospun PLLA/PEGDMA polymer coatings for vascular stent material. J. Biomater. Sci. Polym. Ed. 27, 1086–1099 (2016).
Strohbach, A. & Busch, R. Polymers for Cardiovascular Stent Coatings. Int. J. Polym. Sci. 2015, 782653 (2015).
Palanisamy, M. S., Kulandaivelu, R. & Nellaiappan, S. Improving the corrosion resistance and bioactivity of magnesium by a carbonate conversion-polycaprolactone duplex coating approach. N. J. Chem. 44, 4772–4785 (2020).
Jenney, C. R., DeFife, K. M., Colton, E. & Anderson, J. M. Human monocyte/macrophage adhesion, macrophage motility, and IL-4-induced foreign body giant cell formation on silane-modified surfaces in vitro. J. Biomed. Mater. Res 41, 171–184 (1998).
Kirchner, C. et al. Cytotoxicity of colloidal CdSe and CdSe/ZnS nanoparticles. Nano Lett. 5, 331–338 (2005).
Liu, J. & **, T. Enhanced Anti-corrosion Ability and Biocompatibility of PLGA Coatings on MgZnYNd Alloy by BTSE-APTES Pre-treatment for Cardiovascular Stent. J. Mater. Sci. Technol. 32, 845–857 (2016).
Shin, S. R. et al. Graphene-based materials for tissue engineering. Adv. Drug Deliv. Rev. 105, 255–274 (2016).
Tong, L. B. et al. Enhanced corrosion and wear resistances by graphene oxide coating on the surface of Mg-Zn-Ca alloy. Carbon 109, 340–351 (2016).
Tatavarty, R., Ding, H., Lu, G., Taylor, R. J. & Bi, X. Synergistic acceleration in the osteogenesis of human mesenchymal stem cells by graphene oxide-calcium phosphate nanocomposites. Chem. Commun. 50, 8484–8487 (2014).
Mei, Y. et al. Map** the Interactions among Biomaterials, Adsorbed Proteins, and Human Embryonic Stem Cells. Adv. Mater. 21, 2781–2786 (2009).
Bai, K. et al. Fabrication of chitosan/magnesium phosphate composite coating and the in vitro degradation properties of coated magnesium alloy. Mater. Lett. 73, 59–61 (2012).
Gao, F. et al. Fabrication of chitosan/heparinized graphene oxide multilayer coating to improve corrosion resistance and biocompatibility of magnesium alloys. Mater. Sci. Eng. C. Mater. Biol. Appl 104, 109947 (2019).
Shao, C. et al. Mussel-Inspired Cellulose Nanocomposite Tough Hydrogels with Synergistic Self-Healing, Adhesive, and Strain-Sensitive Properties. Chem. Mater. 30, 3110–3121 (2018).
Li, J.-a, Chen, L., Zhang, X.-q & Guan, S.-k. Enhancing biocompatibility and corrosion resistance of biodegradable Mg-Zn-Y-Nd alloy by preparing PDA/HA coating for potential application of cardiovascular biomaterials. Mater. Sci. Eng.: C. 109, 110607 (2020).
Loriot, M., Linossier, I., Vallée-Réhel, K. & Faÿ, F. Influence of Biodegradable Polymer Properties on Antifouling Paints Activity. Polymers 9, 36 (2017).
Yang, M. C. et al. Electrochemical Polymerization of PEDOT-Graphene Oxide-Heparin Composite Coating for Anti-fouling and Anti-clotting of Cardiovascular Stents. Polymers 11, 1520 (2019).
Mori, Y. et al. A new antithrombogenic material with long polyethyleneoxide chains. Trans. Am. Soc. Artif. Intern Organs 28, 459–463 (1982).
Harder, P., Grunze, M., Dahint, R., Whitesides, G. M. & Laibinis, P. E. Molecular conformation in oligo(ethylene glycol)-terminated self-assembled monolayers on gold and silver surfaces determines their ability to resist protein adsorption. J. Phys. Chem. B 102, 426–436 (1998).
Holmberg, K. et al. Effects on protein adsorption, bacterial adhesion and contact angle of grafting PEG chains to polystyrene. J. Adhes. Sci. Technol. 7, 503–517 (1993).
Gombotz, W. R., Wang, G. H., Horbett, T. A. & Hoffman, A. S. Protein adsorption to poly(ethylene oxide) surfaces. J. Biomed. Mater. Res 25, 1547–1562 (1991).
Lee, H. J. et al. Platelet and bacterial repellence on sulfonated poly(ethylene glycol)-acrylate copolymer surfaces. Colloids Surf., B 18, 355–370 (2000).
Ko, Y. G. et al. Immobilization of poly(ethylene glycol) or its sulfonate onto polymer surfaces by ozone oxidation. Biomaterials 22, 2115–2123 (2001).
Puranik, A. S., Dawson, E. R. & Peppas, N. A. Recent advances in drug eluting stents. Int J. Pharm. 441, 665–679 (2013).
Han, D. K., Jeong, S. Y., Kim, Y. H., Min, B. G. & Cho, H. I. Negative cilia concept for thromboresistance: synergistic effect of PEO and sulfonate groups grafted onto polyurethanes. J. Biomed. Mater. Res 25, 561–575 (1991).
Naghavi, N., de Mel, A., Alavijeh, O. S., Cousins, B. G. & Seifalian, A. M. Nitric oxide donors for cardiovascular implant applications. Small 9, 22–35 (2013).
Scott, R. A. & Panitch, A. Macromolecular approaches to prevent thrombosis and intimal hyperplasia following percutaneous coronary intervention. Biomacromolecules 15, 2825–2832 (2014).
Rao, J. et al. Nitric Oxide-Producing Cardiovascular Stent Coatings for Prevention of Thrombosis and Restenosis. Front. Bioeng. Biotechnol. 8, 578 (2020).
Halkin, A. & Stone, G. W. Polymer-Based Paclitaxel-Eluting Stents in Percutaneous Coronary Intervention. J. Interv. Cardiol. 17, 271–282 (2004).
Rowinsky, E. K. & Donehower, R. C. Paclitaxel (Taxol). N. Engl. J. Med. 332, 1004–1014 (1995).
Ranade, S. V. et al. Physical characterization of controlled release of paclitaxel from the TAXUSTM Express2TM drug-eluting stent. J. Biomed. Mater. Res A 71, 625–634 (2004).
Wiskirchen, J. et al. The effects of paclitaxel on the three phases of restenosis: smooth muscle cell proliferation, migration, and matrix formation: an in vitro study. Invest. Radiol. 39, 565–571 (2004).
Wu, S. et al. Hydrogel Patterning with Catechol Enables Networked Electron Flow. Adv. Funct. Mater. 31, 2007709 (2021).
Thanigaraj, S., Wollmuth, J. R., Zajarias, A., Chemmalakuzhy, J. & Lasala, J. M. From randomized trials to routine clinical practice: an evidence-based approach for the use of drug-eluting stents. Coron. Artery Dis. 17, 673–679 (2006).
Tan, A. et al. Inception to actualization: next generation coronary stent coatings incorporating nanotechnology. J. Biotechnol. 164, 151–170 (2013).
Shen, L. et al. Assessment of an asymmetrical coating stent with sirolimus released from ablumial matrix in porcine model. Clin. Res Cardiol. 101, 917–927 (2012).
Mitra, A. K. & Agrawal, D. K. In stent restenosis: bane of the stent era. J. Clin. Pathol. 59, 232–239 (2006).
Chan, J. W., Lewis, D. R., Petersen, L. K., Moghe, P. V. & Uhrich, K. E. Amphiphilic macromolecule nanoassemblies suppress smooth muscle cell proliferation and platelet adhesion. Biomaterials 84, 219–229 (2016).
Wang, J., Plourde, N. M., Iverson, N., Moghe, P. V. & Uhrich, K. E. Nanoscale amphiphilic macromolecules as lipoprotein inhibitors: the role of charge and architecture. Int J. Nanomed. 2, 697–705 (2007).
Lewis, D. R. et al. Sugar-based amphiphilic nanoparticles arrest atherosclerosis in vivo. Proc. Natl Acad. Sci. USA 112, 2693–2698 (2015).
Chnari, E., Lari, H. B., Tian, L., Uhrich, K. E. & Moghe, P. V. Nanoscale anionic macromolecules for selective retention of low-density lipoproteins. Biomaterials 26, 3749–3758 (2005).
Gu, L., Faig, A., Abdelhamid, D. & Uhrich, K. Sugar-based amphiphilic polymers for biomedical applications: from nanocarriers to therapeutics. Acc. Chem. Res 47, 2867–2877 (2014).
Curcio, A. et al. Effect of stent coating alone on in vitro vascular smooth muscle cell proliferation and apoptosis. Am. J. Physiol. Heart Circ. Physiol. 286, H902–H908 (2004).
Joner, M. et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J. Am. Coll. Cardiol. 48, 193–202 (2006).
Zhu, Y., Gao, C., Liu, X., He, T. & Shen, J. Immobilization of biomacromolecules onto aminolyzed poly(L-lactic acid) toward acceleration of endothelium regeneration. Tissue Eng. 10, 53–61 (2004).
Kolandaivelu, K. et al. Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings. Circulation 123, 1400–1409 (2011).
Polimeni, A. et al. Stent Thrombosis After Percutaneous Coronary Intervention: From Bare-Metal to the Last Generation of Drug-Eluting Stents. Cardiol. Clin. 38, 639–647 (2020).
Clowes, A. W. & Clowes, M. M. Kinetics of cellular proliferation after arterial injury. IV. Heparin inhibits rat smooth muscle mitogenesis and migration. Circ. Res 58, 839–845 (1986).
Theunissen, H. J. et al. Dissociation of heparin-dependent thrombin and factor Xa inhibitory activities of antithrombin-III by mutations in the reactive site. J. Biol. Chem. 268, 9035–9040 (1993).
Biran, R. & Pond, D. Heparin coatings for improving blood compatibility of medical devices. Adv. Drug Deliv. Rev. 112, 12–23 (2017).
Seabra, A. B., Justo, G. Z. & Haddad, P. S. State of the art, challenges and perspectives in the design of nitric oxide-releasing polymeric nanomaterials for biomedical applications. Biotechnol. Adv. 33, 1370–1379 (2015).
Francis, S. H., Busch, J. L., Corbin, J. D. & Sibley, D. cGMP-dependent protein kinases and cGMP phosphodiesterases in nitric oxide and cGMP action. Pharm. Rev. 62, 525–563 (2010).
Kraehling, J. R. & Sessa, W. C. Contemporary Approaches to Modulating the Nitric Oxide-cGMP Pathway in Cardiovascular Disease. Circ. Res 120, 1174–1182 (2017).
Fuentes, E. & Palomo, I. Role of oxidative stress on platelet hyperreactivity during aging. Life Sci. 148, 17–23 (2016).
Lundberg, J. O., Gladwin, M. T. & Weitzberg, E. Strategies to increase nitric oxide signalling in cardiovascular disease. Nat. Rev. Drug Discov. 14, 623–641 (2015).
de Mel, A., Murad, F. & Seifalian, A. M. Nitric oxide: a guardian for vascular grafts? Chem. Rev. 111, 5742–5767 (2011).
Zhou, Y., Lu, Z., Wang, X., Selvaraj, J. N. & Zhang, G. Genetic engineering modification and fermentation optimization for extracellular production of recombinant proteins using Escherichia coli. Appl. Microbiol. Biotechnol. 102, 1545–1556 (2018).
Kouretas, P. C. et al. Non-anticoagulant heparin increases endothelial nitric oxide synthase activity: role of inhibitory guanine nucleotide proteins. J. Mol. Cell Cardiol. 30, 2669–2682 (1998).
Dandona, P. et al. Heparin inhibits reactive oxygen species generation by polymorphonuclear and mononuclear leucocytes. Thromb. Res. 96, 437–443 (1999).
Qiu, H. et al. Biomimetic engineering endothelium-like coating on cardiovascular stent through heparin and nitric oxide-generating compound synergistic modification strategy. Biomaterials 207, 10–22 (2019).
Yang, L. et al. Catechol-mediated and copper-incorporated multilayer coating: An endothelium-mimetic approach for blood-contacting devices. J. Control Release 321, 59–70 (2020).
Luo, R. et al. Multifunctional coatings that mimic the endothelium: surface bound active heparin nanoparticles with in situ generation of nitric oxide from nitrosothiols. J. Mater. Chem. B 6, 5582–5595 (2018).
Simon-Walker, R. et al. Glycocalyx-inspired nitric oxide-releasing surfaces reduce platelet adhesion and activation on titanium. ACS Biomater. Sci. Eng. 3, 68–77 (2017).
Wu, B., Gerlitz, B., Grinnell, B. W. & Meyerhoff, M. E. Polymeric coatings that mimic the endothelium: combining nitric oxide release with surface-bound active thrombomodulin and heparin. Biomaterials 28, 4047–4055 (2007).
Zhou, Z. & Meyerhoff, M. E. Preparation and characterization of polymeric coatings with combined nitric oxide release and immobilized active heparin. Biomaterials 26, 6506–6517 (2005).
Yang, Y. et al. Endothelium-Mimicking Multifunctional Coating Modified Cardiovascular Stents via a Stepwise Metal-Catechol-(Amine) Surface Engineering Strategy. Research 2020, 9203906 (2020).
Lim, W. H. et al. Stent coated with antibody against vascular endothelial-cadherin captures endothelial progenitor cells, accelerates re-endothelialization, and reduces neointimal formation. Arterioscler Thromb. Vasc. Biol. 31, 2798–2805 (2011).
Kong, D. et al. Enhanced inhibition of neointimal hyperplasia by genetically engineered endothelial progenitor cells. Circulation 109, 1769–1775 (2004).
Werner, N. et al. Intravenous transfusion of endothelial progenitor cells reduces neointima formation after vascular injury. Circ. Res. 93, e17–e24 (2003).
Werner, N. & Nickenig, G. Clinical and therapeutical implications of EPC biology in atherosclerosis. J. Cell Mol. Med. 10, 318–332 (2006).
Hua, C. et al. Characterization by high-resolution crystal structure analysis of a triple-helix region of human collagen type III with potent cell adhesion activity. Biochem. Biophys. Res. Commun. 508, 1018–1023 (2019).
Yang, L. et al. A tailored extracellular matrix (ECM) - Mimetic coating for cardiovascular stents by stepwise assembly of hyaluronic acid and recombinant human type III collagen. Biomaterials 276, 121055 (2021).
Poh, C. K., Shi, Z., Lim, T. Y., Neoh, K. G. & Wang, W. The effect of VEGF functionalization of titanium on endothelial cells in vitro. Biomaterials 31, 1578–1585 (2010).
Asahara, T. et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science 275, 964–967 (1997).
Padfield, G. J., Newby, D. E. & Mills, N. L. Understanding the role of endothelial progenitor cells in percutaneous coronary intervention. J. Am. Coll. Cardiol. 55, 1553–1565 (2010).
Folkman, J. Angiogenesis-dependent diseases. Semin Oncol. 28, 536–542 (2001).
Liu, Y. et al. Tailoring of the dopamine coated surface with VEGF loaded heparin/poly-L-lysine particles for anticoagulation and accelerate in situ endothelialization. J. Biomed. Mater. Res. A 103, 2024–2034 (2015).
Wang, B., Hua, J., You, R., Yan, K. & Ma, L. Electrochemically deposition of catechol-chitosan hydrogel coating on coronary stent with robust copper ions immobilization capability and improved interfacial biological activity. Int J. Biol. Macromol. 181, 435–443 (2021).
Hong, Y. J., Jeong, M. H., Ahn, Y. & Kang, J. C. The efficacy and safety of drug-eluting stents in patients with acute myocardial infarction: results from Korea Acute Myocardial Infarction (KAMIR). Int J. Cardiol. 163, 1–4 (2013).
Paul, A., Shao, W., Shum-Tim, D. & Prakash, S. The attenuation of restenosis following arterial gene transfer using carbon nanotube coated stent incorporating TAT/DNA(Ang1+Vegf) nanoparticles. Biomaterials 33, 7655–7664 (2012).
Brito, L. A., Chandrasekhar, S., Little, S. R. & Amiji, M. M. Non-viral eNOS gene delivery and transfection with stents for the treatment of restenosis. Biomed. Eng. Online 9, 56 (2010).
Li, J. M. et al. Local arterial nanoparticle delivery of siRNA for NOX2 knockdown to prevent restenosis in an atherosclerotic rat model. Gene Ther. 17, 1279–1287 (2010).
Che, H. L. et al. Suppression of post-angioplasty restenosis with an Akt1 siRNA-embedded coronary stent in a rabbit model. Biomaterials 33, 8548–8556 (2012).
Che, H. L. et al. Novel Fabrication of MicroRNA Nanoparticle-Coated Coronary Stent for Prevention of Post-Angioplasty Restenosis. Korean Circ. J. 46, 23–32 (2016).
Ambros, V. The functions of animal microRNAs. Nature 431, 350–355 (2004).
McDonald, R. A. et al. Reducing In-Stent Restenosis: Therapeutic Manipulation of miRNA in Vascular Remodeling and Inflammation. J. Am. Coll. Cardiol. 65, 2314–2327 (2015).
Harris, T. A., Yamakuchi, M., Kondo, M., Oettgen, P. & Lowenstein, C. J. Ets-1 and Ets-2 regulate the expression of microRNA-126 in endothelial cells. Arterioscler Thromb. Vasc. Biol. 30, 1990–1997 (2010).
Gouëffic, Y. et al. Hyaluronan induces vascular smooth muscle cell migration through RHAMM-mediated PI3K-dependent Rac activation. Cardiovasc Res. 72, 339–348 (2006).
Muthiah, M. et al. Substrate-mediated delivery of microRNA-145 through a polysorbitol-based osmotically active transporter suppresses smooth muscle cell proliferation: implications for restenosis treatment. J. Biomed. Nanotechnol. 10, 571–579 (2014).
Salva, E. & Akbuğa, J. In vitro silencing effect of chitosan nanoplexes containing siRNA expressing vector targeting VEGF in breast cancer cell lines. Pharmazie 65, 896–902 (2010).
Nolte, A. et al. Small-interfering RNA-eluting surfaces as a novel concept for intravascular local gene silencing. Mol. Med. 17, 1213–1222 (2011).
Okuda, T. et al. Time-dependent complex formation of dendritic poly(L-lysine) with plasmid DNA and correlation with in vitro transfection efficiencies. Org. Biomol. Chem. 1, 1270–1273 (2003).
Ziady, A. G. et al. Transfection of airway epithelium by stable PEGylated poly-L-lysine DNA nanoparticles in vivo. Mol. Ther. 8, 936–947 (2003).
Hossfeld, S. et al. Bioactive coronary stent coating based on layer-by-layer technology for siRNA release. Acta Biomater. 9, 6741–6752 (2013).
Forte, A., Della Corte, A., De Feo, M., Cerasuolo, F. & Cipollaro, M. Role of myofibroblasts in vascular remodelling: focus on restenosis and aneurysm. Cardiovasc Res. 88, 395–405 (2010).
Lu, P., Wang, S., Cai, W. & Sheng, J. Role of TGF-β1/Smad3 signaling pathway in secretion of type I and III collagen by vascular smooth muscle cells of rats undergoing balloon injury. J. Biomed. Biotechnol. 2012, 965953 (2012).
Goh, D. et al. Nanotechnology-based gene-eluting stents. Mol. Pharm. 10, 1279–1298 (2013).
Zhang, H., Ren, K. F., Chang, H., Wang, J. L. & Ji, J. Surface-mediated transfection of a pDNA vector encoding short hairpin RNA to downregulate TGF-beta1 expression for the prevention of in-stent restenosis. Biomaterials 116, 95–105 (2017).
Beshchasna, N. et al. Recent Advances in Manufacturing Innovative Stents. Pharmaceutics 12, 149 (2020).
Saito, Y., Grubman, D., Cristea, E. & Lansky, A. The Firehawk Stent: A Review of a Novel Abluminal Groove-Filled Biodegradable Polymer Sirolimus-Eluting Stent. Cardiol. Rev. 28, 208–212 (2020).
Nartita, R., Ionita, D. & Demetrescu, I. Sustainable Coatings on Metallic Alloys as a Nowadays Challenge. Sustainability 13, 20 (2021).
Geng, Z. et al. Novel Bionic Topography with MiR-21 Coating for Improving BoneImplant Integration through Regulating Cell Adhesion and Angiogenesis. Nano Lett. 20, 7716–7721 (2020).
Acknowledgements
This work was financially supported by National Key Research and Development Program of China (2019YFC1604601, 2019YFC1604600); the National Natural Science Foundation of China (21974029, 22105042); Science and Technology Development Planning Project of Qingdao (Shinan District), China (2022-2-004-YY); Clinical Medicine + X Research Project of the Affiliated Hospital of Qingdao University (X202101027).
Author information
Authors and Affiliations
Contributions
F.Z. and F.L. contributed equally to this work. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhao, F., Liu, F., Gao, C. et al. Interfacing exogenous stents with human coronary artery by self-assembled coating: designs, functionalities and applications. NPG Asia Mater 16, 28 (2024). https://doi.org/10.1038/s41427-024-00548-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41427-024-00548-6
- Springer Japan KK