Abstract
Objective
Adjacent segment disease, junctional kyphosis/failure and pseudarthrosis can negatively impact the mid to long-term outcome in spinal deformity surgery. These complications might be influenced by upper instrumented vertebra (UIV) fixation techniques. In this study we analyze key biomechanical properties of three different UIV fixation techniques and define their ideal clinical use based on patient-specific risk profiles using a finite element analysis (FEA) model.
Methods
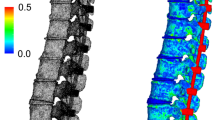
A T9-pelvis posterior instrumented spinal fusion was assumed. Three different FEA models were created based on the UIV fixation technique: T9 pedicle screws (PS); T9 cortical bone screws (CBS); T9 transverse process hooks (TPH). The three FEA models consisted of T8–T10 bone and ligamentous anatomy derived from a CT scan of a healthy patient as well as spinal implants consisting of either pedicle screws, cortical bone screws or transverse process hooks as well as cobalt chromium rods. The FEA models were constrained at T10, axial load as assumed for a healthy 80 kg male during flexion, extension and lateral bending were applied. As surrogate markers for risk of proximal junctional kyphosis, proximal junctional failure, adjacent segment disease and pseudarthrosis the following biomechanical parameters were calculated: UIV range of motion (ROM); intradiscal stress at UIV/UIV + 1; UIV intravertebral stress and screw pull out forces. One-way ANOVA analyses have been performed to compare biomechanical outcome parameters between the three construct variants under investigation.
Results
UIV-ROM was restricted during flexion/extension/lateral bending by: PS: 73%/80%/86%, CBS: 71%/81%/85% and TPH: 62%/76%/85%. Average intradiscal stress at UIV/UIV + 1 during flexion/extension/lateral bending was (Mega Pascal, MPa): PS 0.42/0.44/0.38, CBS 0.49/0.4/0.44, TPH 0.66/0.51/0.58; average intravertebral stress of the UIV superior endplate during flexion/extension/lateral bending was (MPa): PS 2.23/2.12/2.21, CBS 1.87/1.98/1.8, TPH 1.67/0.98/1.53. Screw pull-out forces (N) at UIV during flexion/extension/lateral bending were: PS 476/320/375, CBS 444/245/308. Statistically significant differences were found for intradiscal stress as well as vertebral body average stress (p = 0.02 and p = 0.02).
Conclusion
Different UIV fixation techniques carry different biomechanical properties. Pedicle screw fixation is the most rigid, leading to the highest UIV stress and UIV screw pull out forces. Cortical bones screw fixation is similarly rigid; however, UIV stress and UIV screw pull out is significantly lower. Transverse process hook fixation is the least rigid, with the lowest UIV stress, however highest intradiscal stress at UIV/UIV + 1. Thus, these biomechanical differences may help select optimal UIV fixation techniques according to patient specific risk factors.







Similar content being viewed by others
References
Wang H, Ma L, Yang D et al (2017) Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine 96:e6032
Liu F-Y, Wang T, Yang S-D et al (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383
Kim JS, Phan K, Cheung ZB et al (2019) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Global Spine J 9:32–40
Matsumura A, Namikawa T, Kato M et al (2018) Effect of different types of upper instrumented vertebrae instruments on proximal junctional kyphosis following adult spinal deformity surgery: pedicle screw versus transverse process hook. Asian Spine J 12:622
Wang T, Cai Z, Zhao Y et al. Development of a three-dimensional finite element model of thoracolumbar kyphotic deformity following vertebral column decancellation. Applied bionics and biomechanics 2019; 2019:
Xuan J, Chen J, He H et al (2017) Cortical bone trajectory screws placement via pedicle or pedicle rib unit in the pediatric thoracic spine (T9–T12): a 2-dimensional multiplanar reconstruction study using computed tomography. Medicine 96:e5852
Kim YJ, Lenke LG, Bridwell KH et al (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29:333–342
Matsukawa K, Yato Y, Hynes RA et al (2017) Cortical bone trajectory for thoracic pedicle screws: a technical note. Clin Spine Surg 30:E497–E504
Jendoubi K, Khadri Y, Bendjaballah M et al (2018) Effects of the insertion type and depth on the pedicle screw pullout strength: a finite element study. Appl Bionics Biomech 2018:1–9
Huang J, **e G, Liu Z (2008) FEA of hyperelastic rubber material based on Mooney-Rivlin model and Yeoh model. China Rubber Ind 8:22–26
Kurutz M (2010) Finite element modelling of human lumbar spine. Finite Element Analysis. IntechOpen, London
Kim YJ, Lenke LG (2005) Thoracic pedicle screw placement: free-hand technique. Neurol India 53:512
Rancourt D, Shirazi-Adl A, Drouin G et al (1990) Friction properties of the interface between porous-surfaced metals and tibial cancellous bone. J Biomed Mater Res 24:1503–1519
Bess S, Harris JE, Turner AW et al (2017) The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine 26:125–133. https://doi.org/10.3171/2016.6.SPINE151477
Rodnoi P, Le H, Hiatt L et al (2021) Ligament Augmentation with mersilene tape reduces the rates of proximal junctional kyphosis and failure in adult spinal deformity. Neurospine 18:580–586. https://doi.org/10.14245/ns.2142420.210
Safaee MM, Deviren V, Dalle Ore C et al (2018) Ligament augmentation for prevention of proximal junctional kyphosis and proximal junctional failure in adult spinal deformity. J Neurosurg Spine 28:512–519. https://doi.org/10.3171/2017.9.SPINE1710
Kim YJ, Bridwell KH, Lenke LG et al (2006) Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine 31:2329–2336
Wilke H-J, Herkommer A, Werner K et al (2017) In vitro analysis of the segmental flexibility of the thoracic spine. PLoS ONE 12:e0177823
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine 30:1643–1649
Helgeson MD, Shah SA, Newton PO et al (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35:177–181
Tsutsui S, Hashizume H, Yukawa Y et al (2021) Optimal anchor at the uppermost instrumented vertebra in long fusion from the pelvis to the lower thoracic spine in elderly patients with degenerative spinal deformity: hook versus pedicle screw. Clin Spine Surg 35:E280–E284
Ha Y, Maruo K, Racine L et al (2013) Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 19:360–369
Cammarata M, Aubin C-É, Wang X et al (2014) Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine 39:E500–E507
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 37:1479–1489
Wang H, Ding W, Ma L et al (2017) Prevention of proximal junctional kyphosis: are polyaxial pedicle screws superior to monoaxial pedicle screws at the upper instrumented vertebrae? World Neurosurg 101:405–415
Smith MW, Annis P, Lawrence BD et al (2015) Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J 15:2142–2148
Funding
Funding for this study was received by EN and MM from Medtronic.
Author information
Authors and Affiliations
Contributions
EN, MM, ND, BY, LGL, MF, VA, SKC: conception, drafting, data analysis, manuscript preparation. AS: conception, drafting (original draft and final approval), data collection, manuscript preparation.
Corresponding author
Ethics declarations
Ethical approval
Approval by IRB and informed consent were not required for this study.
Conflict of interest
None of the authors have a conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nevzati, E., Moser, M., Dietz, N. et al. Clinically relevant biomechanical properties of three different fixation techniques of the upper instrumented vertebra in deformity surgery. Spine Deform 10, 1017–1027 (2022). https://doi.org/10.1007/s43390-022-00506-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00506-8