Abstract
Valvular heart disease continues to afflict millions of people around the world. In many cases, the only corrective treatment for valvular heart disease is valve replacement. Valve replacement options are currently limited, and the most common constructs utilized are xenogenic tissue heart valves. The main limitation with the use of this valve type is the development of valve deterioration. Emerging evidence suggests that the underlying driver of valve deterioration is a chronic immune-mediated rejection process of the foreign xenogenic-derived tissue. There is an ongoing focus on the development of an immunologically acceptable, unfixed xenogeneic scaffold for future heart valve constructs. Tissue engineering heart valves are a promising method of develo** a durable, non-immunogenic, non-thrombotic, easily implantable, and readily available implant. In this review, we summarize the various decellularization protocols and scaffold designs for tissue engineered heart valve use and highlight the different cell types and methods for recellularization of tissue engineered heart valves.
Lay Summary
Valve replacement surgery is one of the most common procedures performed by cardiac surgeons. Most patients undergoing valve replacement surgery receive a tissue valve. Tissue valves are made from either cow or pig tissue, and unfortunately tend to fail over time requiring reoperation. One reason these valves fail may be due to a slow rejection of the animal tissue by the human immune system. There is an ongoing focus on the development of artificial heart valves using various tissue engineered designs. The purpose of this review is to summarize various designs and techniques for the creation of artificial heart valves.

Similar content being viewed by others
References
Barone A, Benktander J, Teneberg S, Breimer ME. Characterization of acid and non-acid glycosphingolipids of porcine heart valve cusps as potential immune targets in biological heart valve grafts. Xenotransplantation. 2014;21:510–22. https://doi.org/10.1111/xen.12123.
Griffiths LG, Choe LH, Reardon KF, Dow SW, Christopher OE. Immunoproteomic identification of bovine pericardium xenoantigens. Biomaterials. 2008;29:3514–20. https://doi.org/10.1016/j.biomaterials.2008.05.006.
Gates KV, Dalgliesh AJ, Griffiths LG. Antigenicity of bovine pericardium determined by a novel immunoproteomic approach. Sci Rep. 2017;7:2446. https://doi.org/10.1038/s41598-017-02719-8.
McGregor CGA, Carpentier A, Lila N, Logan JS, Byrne GW. Cardiac xenotransplantation technology provides materials for improved bioprosthetic heart valves. J Thorac Cardiovasc Surg. 2011;141:269–75. https://doi.org/10.1016/j.jtcvs.2010.08.064.
Manji RA, Zhu LF, Nijjar NK, Rayner DC, Korbutt GS, Churchill TA, et al. Glutaraldehyde-fixed bioprosthetic heart valve conduits calcify and fail from xenograft rejection. Circulation. 2006;114:318–27. https://doi.org/10.1161/CIRCULATIONAHA.105.549311.
Manji RA, Hara H, Cooper DKC. Characterization of the cellular infiltrate in bioprosthetic heart valves explanted from patients with structural valve deterioration. Xenotransplantation. 2015;22:406–7. https://doi.org/10.1111/xen.12187.
Vesely I. Heart valve tissue engineering. Circ Res. 2005;97:743–55. https://doi.org/10.1161/01.RES.0000185326.04010.9f.
Duncan AC, Boughner D, Vesely I. Dynamic glutaraldehyde fixation of a porcine aortic valve xenograft. I Effect of fixation conditions on the final tissue viscoelastic properties. Biomaterials. 1996;17:1849–56.
Schenke-Layland K, Vasilevski O, Opitz F, König K, Riemann I, Halbhuber KJ, et al. Impact of decellularization of xenogeneic tissue on extracellular matrix integrity for tissue engineering of heart valves. J Struct Biol. 2003;143:201–8.
Grauss RW, Hazekamp MG, Oppenhuizen F, van Munsteren CJ, Gittenberger-de Groot AC, DeRuiter MC. Histological evaluation of decellularised porcine aortic valves: matrix changes due to different decellularisation methods. Eur J Cardiothorac Surg. 2005;27:566–71. https://doi.org/10.1016/j.ejcts.2004.12.052.
Goecke T, Theodoridis K, Tudorache I, Ciubotaru A, Cebotari S, Ramm R, et al. In vivo performance of freeze-dried decellularized pulmonary heart valve allo- and xenografts orthotopically implanted into juvenile sheep. Acta Biomater. 2018;68:41–52. https://doi.org/10.1016/j.actbio.2017.11.041.
Parravicini R, Cocconcelli F, Verona A, Parravicini V, Giuliani E, Barbieri A. Tuna cornea as biomaterial for cardiac applications. Tex Heart Inst J. 2012;39:179–83.
Cebotari S, Mertsching H, Kallenbach K, Kostin S, Repin O, Batrinac A, et al. Construction of autologous human heart valves based on an acellular allograft matrix. Circulation. 2002;106:I63–8.
Bader A, Schilling T, Teebken OE, Brandes G, Herden T, Steinhoff G, et al. Tissue engineering of heart valves: human endothelial cell seeding of detergent acellularized porcine valves. Eur J Cardiothorac Surg. 1998;14:279–84.
Bertipaglia B, Ortolani F, Petrelli L, Gerosa G, Spina M, Pauletto P, et al. Cell characterization of porcine aortic valve and decellularized leaflets repopulated with aortic valve interstitial cells: the VESALIO project (Vitalitate Exornatum Succedaneum Aorticum Labore Ingenioso Obtenibitur). Ann Thorac Surg. 2003;75:1274–82.
Vincentelli A, Wautot F, Juthier F, Fouquet O, Corseaux D, Marechaux S, et al. In vivo autologous recellularization of a tissue-engineered heart valve: are bone marrow mesenchymal stem cells the best candidates? J Thorac Cardiovasc Surg. 2007;134:424–32. https://doi.org/10.1016/j.jtcvs.2007.05.005.
Goldstein S, Clarke DR, Walsh SP, Black KS, O'Brien MF. Transpecies heart valve transplant: advanced studies of a bioengineered xeno-autograft. Ann Thorac Surg. 2000;70:1962–9.
Elkins RC, Goldstein S, Hewitt CW, Walsh SP, Dawson PE, Ollerenshaw JD, et al. Recellularization of heart valve grafts by a process of adaptive remodeling. Semin Thorac Cardiovasc Surg. 2001;13:87–92.
Simon P, Kasimir MT, Seebacher G, Weigel G, Ullrich R, Salzer-Muhar U, et al. Early failure of the tissue engineered porcine heart valve SYNERGRAFT in pediatric patients. Eur J Cardiothorac Surg. 2003;23:1002–6 discussion 1006.
Konertz W, Angeli E, Tarusinov G, Christ T, Kroll J, Dohmen PM, et al. Right ventricular outflow tract reconstruction with decellularized porcine xenografts in patients with congenital heart disease. J Heart Valve Dis. 2011;20:341–7.
Teebken O, Mertsching H, Haverich A. Modification of heart valve allografts and xenografts by means of tissue engineering. Transplant Proc. 2002;34:2333.
Cebotari S, Lichtenberg A, Tudorache I, Hilfiker A, Mertsching H, Leyh R, et al. Clinical application of tissue engineered human heart valves using autologous progenitor cells. Circulation. 2006;114:132–I-137. https://doi.org/10.1161/CIRCULATIONAHA.105.001065.
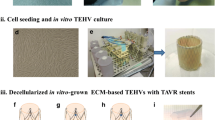
Koenig F, Lee J, Akra B, Hollweck T, Wintermantel E, Hagl C, et al. Is Transcatheter aortic valve implantation of living tissue-engineered valves feasible? An in vitro evaluation utilizing a decellularized and reseeded biohybrid valve. Artif Organs. 2016;40:727–37. https://doi.org/10.1111/aor.12683.
Sutherland FWH, Perry TE, Yu Y, Sherwood MC, Rabkin E, Masuda Y, et al. From stem cells to viable autologous semilunar heart valve. Circulation. 2005;111:2783–91. https://doi.org/10.1161/CIRCULATIONAHA.104.498378.
Weber B, Scherman J, Emmert MY, Gruenenfelder J, Verbeek R, Bracher M, et al. Injectable living marrow stromal cell-based autologous tissue engineered heart valves: first experiences with a one-step intervention in primates. Eur Heart J. 2011;32:2830–40. https://doi.org/10.1093/eurheartj/ehr059.
Syedain ZH, Bradee AR, Kren S, Taylor DA, Tranquillo RT. Decellularized tissue-engineered heart valve leaflets with recellularization potential. Tissue Eng Part A. 2013;19:759–69. https://doi.org/10.1089/ten.TEA.2012.0365.
Motta SE, Fioretta ES, Dijkman PE, Lintas V, Behr L, Hoerstrup SP, et al. Development of an off-the-shelf tissue-engineered sinus valve for transcatheter pulmonary valve replacement: a proof-of-concept study. J Cardiovasc Transl Res. 2018;11:182–91. https://doi.org/10.1007/s12265-018-9800-6.
Schmidt D, Achermann J, Odermatt B, Breymann C, Mol A, Genoni M, et al. Prenatally fabricated autologous human living heart valves based on amniotic fluid derived progenitor cells as single cell source. Circulation. 2007;116:64–I-70. https://doi.org/10.1161/CIRCULATIONAHA.106.681494.
Schmidt D, Mol A, Breymann C, Achermann J, Odermatt B, Gössi M, et al. Living autologous heart valves engineered from human prenatally harvested progenitors. Circulation. 2006;114:125–I-131. https://doi.org/10.1161/CIRCULATIONAHA.105.001040.
VeDepo MC, Detamore MS, Hopkins RA, Converse GL. Recellularization of decellularized heart valves: progress toward the tissue-engineered heart valve. Journal of Tissue Engineering. 2017. https://doi.org/10.1177/2041731417726327.
Dong X, Wei X, Yi W, Gu C, Kang X, Liu Y, et al. RGD-modified acellular bovine pericardium as a bioprosthetic scaffold for tissue engineering. J Mater Sci Mater Med. 2009;20:2327–36. https://doi.org/10.1007/s10856-009-3791-4.
Dijkman PE, Driessen-Mol A, Frese L, Hoerstrup SP, Baaijens FPT. Decellularized homologous tissue-engineered heart valves as off-the-shelf alternatives to xeno- and homografts. Biomaterials. 2012;33:4545–54. https://doi.org/10.1016/j.biomaterials.2012.03.015.
Hof A, Raschke S, Baier K, Nehrenheim L, Selig JI, Schomaker M, et al. Challenges in develo** a reseeded, tissue-engineered aortic valve prosthesis. Eur J Cardiothorac Surg. 2016;50:446–55. https://doi.org/10.1093/ejcts/ezw057.
Zhou J, Ye X, MD WZ, Liu J, Zhang B, Qiu J, et al. Development of decellularized aortic valvular conduit coated by heparin–SDF-1α multilayer. Ann Thorac Surg. 2015;99:612–8. https://doi.org/10.1016/j.athoracsur.2014.09.001.
Ye X, Hu X, Wang H, Liu J, Zhao Q. Polyelectrolyte multilayer film on decellularized porcine aortic valve can reduce the adhesion of blood cells without affecting the growth of human circulating progenitor cells. Acta Biomater. 2012;8:1057–67. https://doi.org/10.1016/j.actbio.2011.11.011.
Ye X, Wang H, Zhou J, Li H, Liu J, Wang Z, et al. The effect of heparin-VEGF multilayer on the biocompatibility of decellularized aortic valve with platelet and endothelial progenitor cells. PLoS One. 2013;8:e54622. https://doi.org/10.1371/journal.pone.0054622.
Huang W, **ao D, Wang Y, Shan Z, Liu X, Lin Q, et al. Fn14 promotes differentiation of human mesenchymal stem cells into heart valvular interstitial cells by phenotypic characterization. J Cell Physiol. 2014;229:580–7. https://doi.org/10.1002/jcp.24480.
Lichtenberg A, Cebotari S, Tudorache I, Sturz G, Winterhalter M, Hilfiker A, et al. Flow-dependent re-endothelialization of tissue-engineered heart valves. J Heart Valve Dis. 2006;15:287–94.
Lichtenberg A, Tudorache I, Cebotari S, Ringes-Lichtenberg S, Sturz G, Hoeffler K, et al. In vitro re-endothelialization of detergent decellularized heart valves under simulated physiological dynamic conditions. Biomaterials. 2006;27:4221–9. https://doi.org/10.1016/j.biomaterials.2006.03.047.
Schenke-Layland K, Opitz F, Gross M, Döring C, Halbhuber KJ, Schirrmeister F, et al. Complete dynamic repopulation of decellularized heart valves by application of defined physical signals-an in vitro study. Cardiovasc Res. 2003;60:497–509. https://doi.org/10.1016/j.cardiores.2003.09.002.
Converse GL, Buse EE, Neill KR, McFall CR, Lewis HN, VeDepo MC, et al. Design and efficacy of a single-use bioreactor for heart valve tissue engineering. J Biomed Mater Res Part B Appl Biomater. 2017;105:249–59. https://doi.org/10.1002/jbm.b.33552.
Tudorache I, Calistru A, Baraki H, Meyer T, Höffler K, Sarikouch S, et al. Orthotopic replacement of aortic heart valves with tissue-engineered grafts. Tissue Eng Part A. 2013;19:1686–94. https://doi.org/10.1089/ten.tea.2012.0074.
Kajbafzadeh A, Ahmadi Tafti SH, Mokhber-Dezfooli M, Khorramirouz R, Sabetkish S, Sabetkish N, et al. Aortic valve conduit implantation in the descending thoracic aorta in a sheep model: the outcomes of pre-seeded scaffold. Int J Surg. 2016;28:97–105. https://doi.org/10.1016/j.ijsu.2016.02.061.
Ghodsizad A, Bordel V, Wiedensohler H, Elbanayosy A, Koerner MM, Gonzalez Berjon JM, et al. Magnetically guided recellularization of decellularized stented porcine pericardium-derived aortic valve for TAVI. ASAIO J. 2014;60:582–6. https://doi.org/10.1097/MAT.0000000000000110.
Kluin J, Talacua H, Smits, Anthal IPM, Emmert MY, MCP B, et al. In situ heart valve tissue engineering using a bioresorbable elastomeric implant – from material design to 12 months follow-up in sheep. Biomaterials. 2017;125:101–17. https://doi.org/10.1016/j.biomaterials.2017.02.007.
Bruder L, Spriestersbach H, Brakmann K, Stegner V, Sigler M, Berger F, et al. Transcatheter decellularized tissue-engineered heart valve (dTEHV) grown on polyglycolic acid (PGA) scaffold coated with P4HB shows improved functionality over 52 weeks due to polyether-ether-ketone (PEEK) insert. J Funct Biomater. 2018;9. https://doi.org/10.3390/jfb9040064.
Availability of Data and Material
Yes
Author information
Authors and Affiliations
Contributions
Sabin J. Bozso performed the literature search and wrote the manuscript. Jimmy J.H. Kang performed the literature search. Anoop Mathew, Michael C. Moon, Darren H. Freed, Jayan Nagendran and Jeevan Nagendran edited the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Description of Future Works
Significant strides have been made in the design artificial heart valves. Ongoing studies will serve to establish the optimal scaffold design, leading to the generation of artificial heart valves that are durable, non-immunogenic, non-thrombotic, easily implantable, and readily available.
Rights and permissions
About this article
Cite this article
Bozso, S.J., Kang, J.J.H., Mathew, A. et al. Comparing Scaffold Design and Recellularization Techniques for Development of Tissue Engineered Heart Valves. Regen. Eng. Transl. Med. 7, 432–439 (2021). https://doi.org/10.1007/s40883-020-00167-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-020-00167-x