Abstract
Purpose
To evaluate: (1) clinical and epidemiological characteristics of outpatients transitioned from Pediatrics Endocrine (PED) to Adult Endocrine Department (AED) in a tertiary center; (2) transition process features, and predictors of drop-out.
Methods
Demographic, clinical, and transition features of 170 consecutive patients with pediatric onset of chronic endocrine or metabolic disease (excluded type 1 diabetes) who transitioned from PED to AED (2007–2020) were retrospective evaluated.
Results
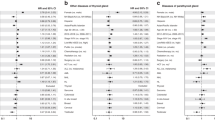
The age at transition was 18.4 ± 4 years (F:M = 1.2: 1), and mean follow-up 2.8 years. The population was heterogeneous; the most (69.4%) was affected by one, 24.1% by two or more endocrine diseases, 6.5% were followed as part of a cancer survivor’s surveillance protocol. The comorbidity burden was high (37, 20.6, and 11.2% of patients had 2, 3, 4, or more diseases). The number of visits was associated with the number of endocrine diseases and the type of them. Adherent subjects had a higher number of comorbidities. Thyroid disorders and more than one comorbidity predicted the adherence to follow-up. Having performed one visit only was predictive of drop-out, regardless of the pathology at diagnosis.
Conclusion
This is the first study that analyzed a specific transition plan for chronic endocrine diseases on long-term follow-up. The proposed “one-size-fits-all model” is inadequate in responding to the needs of patients. A structured transition plan is an emerging cornerstone.
Similar content being viewed by others
Data availability
Available if requested.
References
Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, Slap GB (1993) Transition from child-centered to adult health-care systems for adolescents with chronic conditions. a position paper of the society for adolescent medicine. J Adolesc Health 14:570–576. https://doi.org/10.1016/1054-139X(93)90143-D
Becker J, Ravens E, Pape L, Ernst G (2020) Somatic outcomes of young people with chronic diseases participating in transition programs: a systematic review. J Transit Med 2:1–10. https://doi.org/10.1515/jtm-2020-0003
Crowley R, Wolfe I, Lock K, McKee M (2011) Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 96:548–553. https://doi.org/10.1136/adc.2010.202473
Alassaf A, Gharaibeh L, Grant C, Punthakee Z (2017) Predictors of type 1 diabetes mellitus outcomes in young adults after transition from pediatric care. J Diabetes 9:1058–1064. https://doi.org/10.1111/1753-0407.12536
Cadario F, Prodam F, Bellone S, Trada M, Binotti M, Trada M, Allochis G, Baldelli R, Esposito S, Bona G, Aimaretti G (2009) Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 71:346–350. https://doi.org/10.1111/j.1365-2265.2008.03467.x
Monaghan M, Hilliard M, Sweenie R, Riekert K (2013) Transition readiness in adolescents and emerging adults with diabetes: the role of patient-provider communication. Curr Diab Rep 13:900–908. https://doi.org/10.1007/s11892-013-0420-x
Kapellen TM, Kiess W (2015) Transition of adolescents and young adults with endocrine diseases to adult health care. Best Pract Res Clin Endocrinol Metab 29:505–513. https://doi.org/10.1016/j.beem.2015.03.005
Lotstein DS, Seid M, Klingensmith G, Case D, Lawrence JM, Pihoker C, Dabelea D, Mayer-Davis EJ, Gilliam LK, Corathers S, Imperatore G, Dolan L, Anderson A, Bell RA, Waitzfelder B, SEARCH for diabetes in youth study group (2013) Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 131:1062–1070. https://doi.org/10.1542/peds.2012-1450
Petzold S, Keller A, Keller E, Meigen C, Hirsch W, Kratzsch J et al (2008) A prismatic case: A 31-year old man who did not miss his pituitary. Hormones 7:263–270
Molitch ME, Clemmons DR, Malozowski S, Merriam GR, Vance ML (2011) Evaluation and treatment of adult growth hormone deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:1587–1609. https://doi.org/10.1210/jc.2011-0179
Hanley P, Lord K, Bauer AJ (2016) Thyroid disorders in children and adolescents: a review. JAMA Pediatr 170:1008–1019. https://doi.org/10.1001/jamapediatrics.2016.0486
Hokken-Koelega A, van der Lely AJ, Hauffa B, Häusler G, Johannsson G, Maghnie M, Argente J, DeSchepper J, Gleeson H, Gregory JW, Höybye C, Keleştimur F, Luger A, Müller HL, Neggers S, Popovic-Brkic V, Porcu E, Sävendahl L, Shalet S, Spiliotis B, Tauber M (2016) Bridging the gap: metabolic and endocrine care of patients during transition. Endocr Connect 5:R44–R54. https://doi.org/10.1530/ec-16-0028
Rutishauser C, Sawyer SM, Ambresin AE (2014) Transition of young people with chronic conditions: a cross-sectional study of patient perceptions before and after transfer from pediatric to adult health care. Eur J Pediatr 173:1067–1074. https://doi.org/10.1007/s00431-014-2291-9
Downing J, Gleeson HK, Clayton PE, Davis JRE, Wales JK, Callery P (2013) Transition in endocrinology: The challenge of maintaining continuity. Clin Endocrinol (Oxf) 78:29–35. https://doi.org/10.1111/j.1365-2265.2012.04473.x
Oeffinger KC, Mertens AC, Sklar CA (2007) Chronic health conditions in adult survivors of childhood cancer. Oncol Times 29:26. https://doi.org/10.1056/nejmsa060185
Bondy CA, Bakalov VK (2006) Investigation of cardiac status and bone mineral density in Turner syndrome. Growth Horm IGF Res 16:103–108. https://doi.org/10.1016/j.ghir.2006.03.008
Lanfranco F, Kamischke A, Zitzmann M, Nieschlag E (2004) Klinefelter’s syndrome. Lancet 364:273–283. https://doi.org/10.1016/S0140-6736(04)16678-6
Cannavò S, Cappa M, Ferone D, Isidori AM, Loche S, Salerno M, Maghnie M, Delphi panel members (paediatric, adult endocrinologists) (2022) Appropriate management of growth hormone deficiency during the age of transition: an Italian Delphi consensus statement. J Endocrinol Invest. https://doi.org/10.1007/s40618-022-01880-w
Le Roux E, Menesguen F, Tejedor I, Popelier M, Halbron M, Faucher P, Malivoir S, Pinto G, Léger J, Hatem S, Polak M, Poitou C, Touraine P (2021) Transition of young adults with endocrine and metabolic diseases: the ‘TRANSEND’ cohort. Endocr Connect 10:21–28
Suris JC, Akre C (2015) Key elements for, and indicators of, a successful transition: An international delphi study. J Adolesc Heal 56:612–618. https://doi.org/10.1016/j.jadohealth.2015.02.007
Pedreira CC, Hameed R, Kanumakala S, Zacharin M (2006) Health-care problems of Turner syndrome in the adult woman: a cross sectional study of a victorian cohort and a case for transition. Intern Med J 36:54–57. https://doi.org/10.1111/j.1445-5994.2005.00990.x
Atger-Lallier L, Guilmin-Crepon S, Boizeau P, Zenaty D, Simon D, Paulsen A, Martinerie L, Storey C, Carel J, Léger J (2019) Factors affecting loss to follow-up in children and adolescents with chronic endocrine conditions. Horm Res Paediatr 92:254–261. https://doi.org/10.1159/000505517
Campanini MG (2017) L’ipotiroidismo. Ital J Med 5:7–9. https://doi.org/10.4081/itjm.q.2017.3
Giannouli V, Syrmos N (2017) Exploring attitudes towards endocrine diseases in Greece. Endocrine 55:655–657. https://doi.org/10.1007/s12020-016-1164-6
Sbardella E, Pozza C, Isidori AM, Grossman AB (2019) Endocrinology and adolescence: dealing with transition in young patients with pituitary disorders. Eur J Endocrinol 181:R155–R171. https://doi.org/10.1530/eje-19-0298
Syed IA, Nathan PC, Barr R, Rosenberg-Yunger ZRS, D’Agostino NM, Klassen AF (2016) Examining factors associated with self-management skills in teenage survivors of cancer. J Cancer Surviv 10:686–691. https://doi.org/10.1007/s11764-016-0514-y
Mostoufi-Moab S, Seidel K, Leisenring WM, Armstrong GT, Oeffinger KC, Stovall M, Meacham LR, Green DM, Weathers R, Ginsberg JP, Robison LL, Sklar CA (2016) Endocrine abnormalities in aging survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 34:3240–3247. https://doi.org/10.1200/jco.2016.66.6545
Ruggeri RM, Trimarchi F, Giuffrida G, Certo R, Cama E, Campennì A, Alibrandi A, De Luca F, Wasniewska M (2017) Autoimmune comorbidities in Hashimoto’s thyroiditis: different patterns of association in adulthood and childhood/adolescence. Eur J Endocrinol 176:133–141. https://doi.org/10.1530/eje-16-0737
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the local ethical committee (“Maggiore della Carità” Hospital, Novara).
Informed consent
Informed consent was obtained from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prodam, F., Caputo, M., Romanisio, M. et al. Transition in endocrinology: predictors of drop-out of a heterogeneous population on a long-term follow-up. J Endocrinol Invest 46, 1009–1016 (2023). https://doi.org/10.1007/s40618-022-01975-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01975-4