Abstract
Purpose
To investigate the relationship between the single-point insulin sensitivity estimator (SPISE) index, an insulin sensitivity indicator validated in adolescents and adults, and metabolic profile in overweight/obese children, and to evaluate whether basal SPISE is predictive of impaired glucose regulation (IGR) development later in life.
Methods
The SPISE index (= 600 × HDL0.185/Triglycerides0.2 × BMI1.338) was calculated in 909 overweight/obese children undergoing metabolic evaluations at University of Cagliari, Italy, and in 99 normal-weight, age-, sex-comparable children, selected as a reference group, together with other insulin-derived indicators of insulin sensitivity/resistance. 200 overweight/obese children were followed-up for 6.5 [3.5–10] years, data were used for longitudinal retrospective investigations.
Results
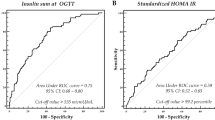
At baseline, 96/909 (11%) overweight/obese children had IGR; in this subgroup, SPISE was significantly lower than in normo-glycaemic youths (6.3 ± 1.7 vs. 7 ± 1.6, p < 0.001). The SPISE index correlated positively with the insulin sensitivity index (ISI) and the disposition index (DI), negatively with age, blood pressure, HOMA-IR, basal and 120 min blood glucose and insulin (all p values < 0.001). A correlation between SPISE, HOMA-IR and ISI was also reported in normal-weight children. At the 6.5-year follow-up, lower basal SPISE—but not ISI or HOMA-IR—was an independent predictor of IGR development (OR = 3.89(1.65–9.13), p = 0.002; AUROC: 0.82(0.72–0.92), p < 0.001).
Conclusion
In children, low SPISE index is significantly associated with metabolic abnormalities and predicts the development of IGR in life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obesity in childhood are conditions epidemically spread worldwide, and the dramatic increase of their incidence in the last decades has become a relevant public health issue around the world [1]. Data show that 17.9% of European children were overweight or obese during the period 2006–2016. The prevalence estimate of obesity was 5.3%, with highest values reported in the Southern European countries [2]. The increasing prevalence in children comes with escalations in both current childhood and future adulthood morbidity and mortality [3], but also in concomitant costs [4].
Early onset obesity is an independent risk factor for the development of insulin resistance and type 2 diabetes (T2D)[16], whereas most of the population-based health surveys include BMI and lipid profile [23], the SPISE index may also be used as a sensitive and easy method to assess insulin sensitivity at the population level.
The SPISE index has been validated in a cross-sectional investigation including a large cohort of over 1200 nondiabetic adults and 29 obese adolescents [23]. In this study, a cut-off value of SPISE below 6.61 was proposed to indicate the presence of insulin resistance, as estimated by the comparison with the clamp-derived M value.
Conversely, our study is the first investigation exploring the SPISE index in the prediction of impaired glucose regulation development in overweight and obese children. Thus, rather than using a previously identified SPISE cut-off obtained in a non-comparable population and study design, in our study we explored whether belonging to the lowest quartile of the SPISE index distribution, i.e. SPISE below 6.08, at baseline was associated with the development of altered glucose metabolism. Thus, a SPISE index cut-off < 6.08 may be proposed as a novel threshold for low insulin sensitivity in children which could predict the development of dysglycaemia later in life in the setting of the real world evidence.
The rationale of the SPISE index to identify insulin resistance is particularly intriguing: TG and HDL represent changes in lipids and lipoproteins that are among the earliest manifestations of insulin resistance [48,49,50]. Indeed, insulin resistance measured by euglycaemic clamp is associated with adverse lipid and lipoprotein changes favoring atherosclerosis even in subjects without diabetes. The addition of BMI, another easy indirect measure of adipose tissue and insulin sensitivity, further enhances the sensitivity of the SPISE index. For all these characteristics, the SPISE index, but not traditional insulin-derived indicators of insulin sensitivity/resistance such ad ISI and HOMA-IR, performed very well as a strong independent predictor of development of IGR in the large population of overweight and obese children included in this study.
In conclusion, this study demonstrates that the SPISE index is a strong indicator of insulin sensitivity in children with and without body weight excess, and that in overweight/obese individuals it predicts the development of impaired glucose regulation later in life independently from potential confounders. Finally, for its characteristics of non-invasive, low-cost and simple to estimate index, the SPISE index may represent an easy surrogate of insulin sensitivity in overweight/obese children to be used as a screening tool for metabolic risk assessment on a large scale.
Availability of data and material
The authors agree to share data upon request.
References
Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 307:483–490. https://doi.org/10.1001/jama.2012.40
Garrido-Migue M, Oliveira A, Cavero-Redondo I, Álvarez-Bueno C, Pozuelo-Carrascosa DP, Soriano-Cano A et al (2019) Prevalence of overweight and obesity among European preschool children: a systematic review and meta-regression by food group consumption. Nutrients. https://doi.org/10.3390/nu11071698
Berenson GS (2012) Health consequences of obesity. Pediatr Blood Cancer 58:117–121. https://doi.org/10.1002/pbc.23373
Hamilton D, Dee A, Perry IJ (2018) The lifetime costs of overweight and obesity in childhood and adolescence: a systematic review. Obes Rev 19:452–463. https://doi.org/10.1111/obr.12649
Fang X, Zuo J, Zhou J, Cai J, Chen C, **ang E et al (2019) Childhood obesity leads to adult type 2 diabetes and coronary artery diseases: A 2-sample Mendelian randomization study. Medicine. https://doi.org/10.1097/MD.0000000000016825
Goran MI, Ball GDC, Cruz ML (2003) Cardiovascular endocrinology 2: Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab 88:1417–1427. https://doi.org/10.1210/jc.2002-021442
Hagman E, Besor O, Hershkop K, Santoro N, Pierpont B, Mata M et al (2019) Relation of the degree of obesity in childhood to adipose tissue insulin resistance. Acta Diabetol 56:219–226. https://doi.org/10.1007/s00592-018-01285-3
Laakso M, Kuusisto J (2014) Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol 10:293–302. https://doi.org/10.1038/nrendo.2014.29
Valaiyapathi B, Gower B, Ashraf AP (2019) Pathophysiology of type 2 diabetes in children and adolescents. Curr Diabetes Rev 16:220–229. https://doi.org/10.2174/1573399814666180608074510
Poulsen P, Levin K, Petersen I, Christensen K, Beck-Nielsen H, Vaag A (2005) Heritability of insulin secretion, peripheral and hepatic insulin action, and intracellular glucose partitioning in young and old Danish twins. Diabetes 54:275–283. https://doi.org/10.2337/diabetes.54.1.275
Boerschmann H, Pflüger M, Henneberger L, Ziegler AG, Hummel S (2010) Prevalence and predictors of overweight and insulin resistance in offspring of mothers with gestational diabetes mellitus. Diabetes Care 33:1845–1849. https://doi.org/10.2337/dc10-0139
Vaag A, Bjørn Jensen C, Poulsen P, Brøns C, Pilgaard K, Grunnet L et al (2006) Metabolic aspects of insulin resistance in individuals born small for gestational age. Horm Res Paediatr 65:137–143. https://doi.org/10.1159/000091519
Ong YY, Sadananthan SA, Aris IM, Tint MT, Yuan WL, Huang JY et al (2020) Mismatch between poor fetal growth and rapid postnatal weight gain in the first 2 years of life is associated with higher blood pressure and insulin resistance without increased adiposity in childhood: The GUSTO cohort study. Int J Epidemiol 49:1591–1603. https://doi.org/10.1093/ije/dyaa143
Payal V, Jora R, Sharma P, Gupta P, Gupta M (2016) Premature birth and insulin resistance in infancy: a prospective cohort study. Indian J Endocrinol Metab 20:497–505. https://doi.org/10.4103/2230-8210.183470
Rogers JM (2019) Smoking and pregnancy: epigenetics and developmental origins of the metabolic syndrome. Birth Defects Res 111:1259–1269. https://doi.org/10.1002/bdr2.1550
Levy-Marchal C, Arslanian S, Cutfield W, Sinaiko A, Druet C, Marcovecchio ML et al (2010) Insulin resistance in children: consensus, perspective, and future directions. J Clin Endocrinol Metab 95:5189–5198. https://doi.org/10.1210/jc.2010-1047
Romualdo MCDS, De Nóbrega FJ, Escrivão MAMS (2014) Insulin resistance in obese children and adolescents. J Pediatr 90:600–607. https://doi.org/10.1016/j.jped.2014.03.005
Lee JM, Okumura MJ, Davis MM, Herman WH, Gurney JG (2006) Prevalence and determinants of insulin resistance among U.S. adolescents: a population-based study. Diabetes Care 29:2427–2432. https://doi.org/10.2337/dc06-0709
Chiarelli F, Marcovecchio ML (2008) Insulin resistance and obesity in childhood. Eur J Endocrinol. https://doi.org/10.1530/EJE-08-0245
Hellman B (2009) Pulsatility of insulin release a clinically important phenomenon. Ups J Med Sci 114:193–205. https://doi.org/10.3109/03009730903366075
Marcovina S, Bowsher RR, Miller WG, Staten M, Myers G, Caudill SP et al (2007) Standardization of insulin immunoassays: report of the American Diabetes Association Workgroup. Clin Chem 53:711–716. https://doi.org/10.1373/clinchem.2006.082214
Duckworth WC, Bennett RG, Hamel FG (1998) Insulin degradation: progress and potential. Endocr Rev 19:608–624. https://doi.org/10.1210/edrv.19.5.0349
Paulmichl K, Hatunic M, Højlund K, Jotic A, Krebs M, Mitrakou A et al (2016) Modification and validation of the triglyceride-to-HDL cholesterol ratio as a surrogate of insulin sensitivity in white juveniles and adults without diabetes mellitus: the single point insulin sensitivity estimator (SPISE). Clin Chem 62:1211–1219. https://doi.org/10.1373/clinchem.2016.257436
Correa-Burrows P, Blanco E, Gahagan S, Burrows R (2020) Validity assessment of the single-point insulin sensitivity estimator (spise) for diagnosis of cardiometabolic risk in post-pubertal hispanic adolescents. Sci Rep 10:1–10. https://doi.org/10.1038/s41598-020-71074-y
Sentinelli F, Bertoccini L, Incani M, Pani MG, David F, Bailett D et al (2020) Association of apelin levels in overweight-obese children with pubertal development, but not with insulin sensitivity: 6.5 years follow up evaluation. Endocr Res 45:233–240. https://doi.org/10.1080/07435800.2020.1804929
Cambuli VM, Incani M, Pilia S, Congiu T, Cavallo MG, Cossu E et al (2009) Oral glucose tolerance test in Italian overweight/obese children and adolescents results in a very high prevalence of impaired fasting glycaemia, but not of diabetes. Diabetes Metab Res Rev 25:528–534. https://doi.org/10.1002/dmrr.980
American Diabetes Association (2021) 2 classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care 44(Suppl 1):S15–S33. https://doi.org/10.2337/dc21-S002
Cacciari E, Milani S, Balsamo A, Spada E, Bona G, Cavallo L et al (2006) Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J Endocrinol Invest 29:581–593. https://doi.org/10.1007/BF03344156
Tanner JM (1986) 1 Normal growth and techniques of growth assessment. Clin Endocrinol Metab 15:411–451. https://doi.org/10.1016/S0300-595X(86)80005-6
Muniyappa R, Lee S, Chen H, Quon MJ (2008) Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. https://doi.org/10.1152/ajpendo.00645.2007
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470. https://doi.org/10.2337/diacare.22.9.1462
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419. https://doi.org/10.1007/BF00280883
Utzschneider KM, Prigeon RL, Faulenbach MV, Tong J, Carr DB, Boyko EJ et al (2009) Oral disposition index predicts the development of future diabetes above and beyond fasting and 2-h glucose levels. Diabetes Care 32:335–341. https://doi.org/10.2337/dc08-1478
George L, Bacha F, Lee SJ, Tfayli H, Andreatta E, Arslanian S (2011) Surrogate estimates of insulin sensitivity in obese youth along the spectrum of glucose tolerance from normal to prediabetes to diabetes. J Clin Endocrinol Metab 96:2136–2145. https://doi.org/10.1210/jc.2010-2813
Yeckel CW, Weiss R, Dziura J, Taksali SE, Dufour S, Burgert TS et al (2004) Validation of insulin sensitivity indices from oral glucose tolerance test parameters in obese children and adolescents. J Clin Endocrinol Metab 89:1096–1101. https://doi.org/10.1210/jc.2003-031503
Cederholm J, Zethelius B (2019) SPISE and other fasting indexes of insulin resistance: risks of coronary heart disease or type 2 diabetes. Comparative cross-sectional and longitudinal aspects. Ups J Med Sci 124:265–272. https://doi.org/10.1080/03009734.2019.1680583
Dudi P, Goyal B, Saxena V, Rabari K, Mirza AA, Naithani M et al (2019) Single point insulin sensitivity estimator as an index for insulin sensitivity for metabolic syndrome: a study in North Indian population. J Lab Physicians 11:244–248. https://doi.org/10.4103/jlp.jlp_163_18
Miyakoshi T, Sagesaka H, Sato Y, Hirbayashi K, Koike H, Yamashita K et al (2019) Reappraisal of attenuated insulin sensitivity in the evolution of non-alcoholic fatty liver disease. Eur J Clin Nutr 73:770–775. https://doi.org/10.1038/s41430-018-0246-3
Endukuru CK, Gaur GS, Yerrabelli D, Sahoo J, Vairappan B (2021) Cut-off values and clinical utility of surrogate markers for insulin resistance and beta-cell function to identify metabolic syndrome and its components among southern Indian adults. J Obes Metab Syndr 29:281–291. https://doi.org/10.7570/JOMES20071
Sagesaka H, Sato Y, Someya Y, Tamura Y, Shimodaira M, Miyakoshi T et al (2018) Type 2 diabetes: when does it start? J Endocr Soc 2:476–484. https://doi.org/10.1210/js.2018-00071
Nobili V, Mantovani A, Cianfarani S, Alisi A, Mosca A, Sartorelli MR et al (2019) Prevalence of prediabetes and diabetes in children and adolescents with biopsy-proven non-alcoholic fatty liver disease. J Hepatol 71:802–810. https://doi.org/10.1016/j.jhep.2019.06.023
Serbis A, Giapros V, Kotanidou EP, Galli-Tsinopoulou A, Siomou E (2021) Diagnosis, treatment and prevention of type 2 diabetes mellitus in children and adolescents. World J Diabetes 12:344–365. https://doi.org/10.4239/wjd.v12.i4.344
World Health Organization (2020) Noncommunicable diseases: Childhood overweight and obesity. https://www.who.int/news-room/q-a-detail/noncommunicable-diseases-childhood-overweight-and-obesity. Accessed on the 16 May 2021
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol Endocrinol Metab Gastrointest Physiol. https://doi.org/10.1152/ajpendo.1979.237.3.e214
Tagi VM, Giannini C, Chiarelli F (2019) Insulin resistance in children. Front Endocrinol 10:342. https://doi.org/10.3389/fendo.2019.00342
Park SE, Park CY, Sweeney G (2015) Biomarkers of insulin sensitivity and insulin resistance: past, present and future. Crit Rev Clin Lab Sci 52:180–190. https://doi.org/10.3109/10408363.2015.1023429
Gutch M, Kumar S, Razi SM, Gupta K, Gupta A (2015) Assessment of insulin sensitivity/resistance. Indian J Endocrinol Metab 19:160–164. https://doi.org/10.4103/2230-8210.146874
Laakso M, Sarlund H, Mykkänen L (1990) Insulin resistance is associated with lipid and lipoprotein abnormalities in subjects with varying degrees of glucose tolerance. Arterioscler Thromb Vasc Biol 10:223–231. https://doi.org/10.1161/01.ATV.10.2.223
Di Bonito P, Pacifico L, Chiesa C, Valerio G, Miraglia Del Giudice E, Maffeis C et al (2017) Impaired fasting glucose and impaired glucose tolerance in children and adolescents with overweight/obesity. J Endocrinol Invest 40:409–416. https://doi.org/10.1007/s40618-016-0576-8
Di Bonito P, Moio N, Scilla C, Cavuto L, Sibilio G, Sanguigno E et al (2012) Usefulness of the high triglyceride-to-HDL cholesterol ratio to identify cardiometabolic risk factors and preclinical signs of organ damage in outpatient children. Diabetes Care 35:158–162. https://doi.org/10.2337/dc11-1456
Funding
Open access funding provided by Università degli Studi dell’Aquila within the CRUI-CARE Agreement. This work was supported by Research Grants from the Department MeSVA, University of L’Aquila (Bando Ricerca FFO 2020 and FFO 2021) to Marco G. Baroni, Sapienza University of Rome “Ricerca Ateneo” to M.G.Cavallo. Ilaria Barchetta is supported by a Grant from Eli Lilly Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed written consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barchetta, I., Dule, S., Bertoccini, L. et al. The single-point insulin sensitivity estimator (SPISE) index is a strong predictor of abnormal glucose metabolism in overweight/obese children: a long-term follow-up study. J Endocrinol Invest 45, 43–51 (2022). https://doi.org/10.1007/s40618-021-01612-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01612-6