Abstract
Importance
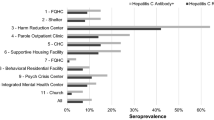
Hepatitis C virus (HCV) care cascade data by race/ethnicity for US correctional populations are sparse.
Objective
To evaluate the HCV care cascade by race/ethnicity for a state correctional population.
Design, Setting, and Participants
This retrospective cohort study used Connecticut Department of Correction data for incarcerated individuals tested, diagnosed, and treated for chronic HCV infection with direct-acting antivirals (DAAs) from 2019 to 2023.
Main Outcomes and Measures
HCV care cascade outcomes, including testing, treatment, and cure rates, were compared by race/ethnicity. Poisson regression was used to estimate prevalence ratios (PRs), with adjustment for demographic and legal status factors.
Results
A total of 24,867 patients tested for HCV (88.9% men, mean (SD) age 35.6 (11.8), 32.7% White, 37.9% Black, 28.4% Hispanic, 0.6% Asian, 0.4% American Indian/Alaska Native (AIAN), 34.7% sentenced ≥ 1 year). Both HCV exposure and chronic HCV were highest for White (27.1% and 15.2%) and lowest for Black individuals (4.6% and 2.6%) (P < 0.01, for both outcomes). While incarcerated, 63.2% of chronic HCV patients started DAAs, and treatment rates did not significantly differ by race/ethnicity (P > 0.05). For those treated and having post-treatment lab data available, cure rates were 98.8% or better for all racial/ethnic groups (P > 0.05). In the adjusted regression analyses, HCV treatment initiation was lower for those sentenced < 1 year (PR, 0.76; 95% CI, 0.67–0.87) and unsentenced (PR, 0.85; 95% CI, 0.80–0.91) than those sentenced ≥ 1 year. The adjusted prevalence of advanced fibrosis stage/activity grade was not significantly associated with race/ethnicity.
Conclusions
In this cohort study, less than two-thirds of chronic HCV patients initiated DAA treatment during their incarceration, and for those with available data, nearly all were cured. While there were disparities in HCV exposure and chronic HCV infection, significant racial/ethnic differences were not observed for treatment initiation or cure rates. Further efforts are needed to increase HCV treatment, especially for patients with shorter incarceration periods.

Similar content being viewed by others
Data Availability
Data were obtained for quality improvement of clinical care and are not publicly available.
References
Rosenberg ES, Rosenthal EM, Wall EW, Barker L, Hofmeister MG, Sullivan PS, et al. Prevalence of hepatitis C virus infection in US States and the District of Columbia, 2013 to 2016. JAMA Netw Open. 2018;1(8):e186371.
Centers for Disease Control and Prevention. Viral hepatitis: numbers and rates of death with hepatitis C listed as a cause of death among residents, by state or jurisdiction - United States, 2017 - 2021. 2023. https://www.cdc.gov/hepatitis/statistics/2021surveillance/hepatitis-c/table-3.7.htm. [cited 2023 September 23].
Word Health Organization. Hepatitis C. 2023. https://www.who.int/news-room/fact-sheets/detail/hepatitis-c. [cited 2023 September 23].
Office of Management and Budget, The White House. Budget of the US government. Fiscal Year 2024. 2023. https://www.whitehouse.gov/wp-content/uploads/2023/03/budget_fy2024.pdf. [cited 2023 September 23].
Fleurence RL, Collins FS. A national hepatitis C elimination program in the United States: a historic opportunity. JAMA. 2023;329(15):1251–2.
US Department of Health and Human Services. Viral hepatitis national strategic plan. 2021. https://www.hhs.gov/sites/default/files/Viral-Hepatitis-National-Strategic-Plan-2021-2025.pdf. [cited 2023 September 23].
Carson EA. Prisoners in 2021 - statistical tables. 2022. https://bjs.ojp.gov/sites/g/files/xyckuh236/files/media/document/p21st.pdf. [cited 2023 September 23].
Flaniagin A, Frey T, Christiansen SL. Updated guidance on the reporting of race and ethnicity in medical and scientific journals. JAMA. 2021;326(7):621–7.
Federal Bureau of Investigation, US Department of Justice. Crime in the United States, 2019. 2020. https://ucr.fbi.gov/crime-in-the-u.s/2019/crime-in-the-u.s.-2019/topic-pages/persons-arrested. [cited 2023 September 23].
Trickey A, Fraser HLAG, Peacock A, Colledge S, Walker J, Leung J, et al. The contribution of injecting drug use as a risk factor for hepatitis C virus transmission globally, regionally, and at country level: a modelling study. Lancet Gastroeneterol Hepatol. 2019;4(6):435–44.
Homberg SD, Spradling PR, Moorman AC, Denniston MM. Hepatitis C in the United States. New Engl J Med. 2013;368(20):1859–61.
Yehia BR, Schranz AJ, Umscheid CA, Re VL3. The treatment cascade for chronic hepatitis C virus infection in the United States: a systematic review and meta-analysis. PLoS One. 2014 July 2; 9(7): e101554.
Akiyama MJ, Kronfli N, Cabezas J, Sheehan Y, Thurairajah PH, Lines R, et al. Hepatitis C elimination among people incarcerated in prisons: a challenges and recommendations for action within a health systems framework. Lancet Gastrolenterol Hepatol. 2021;6(5):391–400.
Winter RJ, Holmes JA, Papaluca TJ, Thompson AJ. The importance of prisons in achieving hepatitis C elimination: insights from the Australia experience. Viruses. 2022;14:497.
Kaufman HW, Meyer WA III, Huang X. Hepatitis C care cascade incarcerated or detained persons and general population in California, 2011–2021. Ann Gastroenterol Dig Syst. 2023;6(1):1071.
Hale AJ, Mathur S, Dejace J, Lidofsky SD. Statewide assessment of the hepatitis C virus care cascade for incarcerated persons in Vermont. Public Health Rep. 2023;138(2):265–72.
Chan J, Kaba F, Schwartz J, Bocour A, Akiyama MJ, Rosner Z, et al. The hepatitis C virus care cascade in the New York City jail system during the direct acting antiviral treatment era, 2014–2017. EClinicalMedicine. 2020;5(27):100567.
Cuadrado A, Llerena S, Cobo C, Pallas JR, Mateo M, Cabezas J, et al. Microenvronment eradication of hepatitis C: a novel treatment paradigm. Am J Gastroenterol. 2018;113:1639–48.
Kronfli N, Dussault C, Klein MB, Lebouche B, Sebastiani G, Cox J. The hepatitis C virus cascade of care in a Quebec provincial prison: a retrospective cohort study. CMAJ Open. 2019;7(4):E674–9.
Papaluca T, McDonald L, Craigie A, Gibson A, Desmond P, Wong D, et al. Outcomes of treatment for hepatitis C in prisoners using a nurse-led, statewide model of care. J Hematol. 2019;70:839–46.
Winter RJ, Sheehan Y, Papaluca T, MacDonald GA, Rowland J, Colman A, et al. Consensus recommendations on the management of hepatitis C in Australia’s prisons. Med J Australia. 2023;218(5):231–7.
Yang TH, Fang YJ, Hsu SJ, Chiu MC, Yu JJ, Kuo CC, et al. Microelimination of chronic hepatitis C y universal screening plus direct-acting antivirals for incarcerated persons in Taiwan. Open Forum Infect Dis. 2020;7(8):ofaa301.
Johnson A, Shearer J, Thompson C, Jelley R, Aldridge J, Allsop C, et al. Impact of 5 years of hepatitis C testing and treatment in the North East of England prisons. J Viral Hepat. 2023;30:914–21.
Mongale E, Allen S, Brew I, Ludlow-Rhodes A, Royal N, Waldron J, et al. Development and optimisation of a reception testing protocol designed to eliminate HCV in the UK prison population. JHEP Reports. 2023;6(1):100937. https://doi.org/10.1016/j.jhepr.2023.100937. eCollection 2024 Jan.
Coutinho LMS, Scazufca M, Menezes PR. Methods for estimating prevalence ratios in cross-sectional studies. Rev Saude Publica. 2008;42(6):992–8.
Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with general population. J Epidemiol Community Health. 2009;63(11):912–9.
Maruschak LM, Berzofsky M, Unangst J. Medical problems of state and federal prisoners and jail inmates, 2011–12. 2016. https://bjs.ojp.gov/content/pub/pdf/mpsfpji1112.pdf. [cited 2023 September 23].
Maruschak LM, Bronson J, Alper M. Medical problems reported by prisoners. 2021. https://bjs.ojp.gov/sites/g/files/xyckuh236/files/media/document/mprpspi16st.pdf. [cited 2023 September 23].
Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and release from US correctional facilities, 1997. Am J Public Health. 2002;92(11):1789–94.
Liang TJ, Ward JW. Hepatitis C in injection-drug users - a hidden danger of the opioid epidemic. N Engl J Med. 2018;378(13):1169–71.
Busschots D, Kremer C, Bielen R, Koc OM, Heyens L, Nevens F, et al. Hepatitis C prevalence in incarcerated settings between 2013–2021: a systematic review and meta-analysis. BMC Public Health. 2022;22(1):2159.
Salari N, Darvishi N, Hemmati M, Shohaimi S, Ghyasi Y, Hossaini F, et al. Global prevalence of hepatitis C in prisoners: a comprehensive systematic review and meta-analysis. Adv Virol. 2022;14(167):1025–39.
Thompson WW, Symum H, Sandul A, Gupta N, Patel P, Nelson N, et al. Vital signs: hepatitis C treatment among insured adults - United States, 2019–2020. Morb Mortal Wkly Rep. 2022;71(32):1011–7.
American Association for the Study of Liver Diseases, Infectious Diseases Society of America. HCV testing and treatment in correctional settings.2022. https://www.hcvguidelines.org/unique-populations/correctional. [cited 2023 September 23].
Kapadia SN, Zhang H, Gonzalez CJ, Sen B, Franco R, Hutchings K, et al. Hepatitis C treatment initiation among US Medicaid enrollees. JAMA Netw Open. 2023;6(8):e2327326.
Acknowledgements
The authors would like to thank the following CTDOC staff who assisted with the data preparation: Mary Lansing; Arielle Reich; Annie M. Mendez, CCHP; Dawn Rios, BSN, RN, CIC; Ada Rodríguez, LPN; Sanjita Sharma; Kirsten Shea; and Daniel Wrobel, RN, CCHP. From Quest Diagnostics, we would like to thank Amy B. Haley and Jennifer A. Maldonado for assisting with compiling the Quest HCV lab data. From Diamond Pharmacy, we would like to thank Christopher Cicuto, PharmD, for assisting with compiling the HCV DAA treatment data.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design, and writing. BSK performed all data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This observational study was performed as part of the agency’s quality improvement efforts; therefore, IRB approval was not required.
Consent to Participate
All individual patients consented to clinical care provided to them.
Consent for Publication
Only aggregate data are reported; therefore, consent to publish was not required.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kennedy, B.S., Richeson, R.P. & Houde, A.J. Hepatitis C Virus Care Cascade by Race/Ethnicity in a Statewide Correctional Population, 2019–2023. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02058-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-02058-1